Chiropractor, Dr. Alexander Jimenez looks at the Purpose of vastus medialis oblique, which is widely believed to be a patellar stabilizer.
You will find still an overabundance of study Articles of interest to the function and dysfunction of the vastus medialis oblique (VMO), particularly in connection with its role as a lively patella stabilizer and the role that it plays in patella-femoral pain syndromes (PFPS). Indeed, it is among the most studied muscles in sports medicine and rehabilitation. Disseminating the sheer volume of printed content can become confusing; the significance of the VMO in preventing PFPS remains debated by experts in contradictory reports on the specific contribution that VMO performs in patella control and pain syndromes.
PFPS is a pathology related to the contact and tracking between the patella and the underlying femur and the trochlear groove that is housed in the distal end of the femur. PFPS is a frequent injury to the knee. It affects sports and moves that demand high patella forces whilst the knee is flexed like stair climbing, running mountains, biking and weight training(1).
It has been estimated that 14-17percent(2,3)or 25\%(4) of knee injuries presenting to the sports medicine practitioner requires the patella-femoral joint. It has been argued for quite a long time that VMO deficiency could lead to patella tracking difficulties and be the precursor to PFPS, and so exercises for the VMO are necessary to counteract PFPS(5,6).
Part one of this of this article unpacks Much of the presented study to discuss the appropriate anatomy and biomechanics of the VMO as it is now understood. In the next part, we look at how VMO dysfunction can relate to PFPS, how it may become dysfunctional in the existence of knee pain, and which exercises can be utilized to rehabilitate the dysfunctional VMO.
Table of Contents
Anatomy & Biomechanics
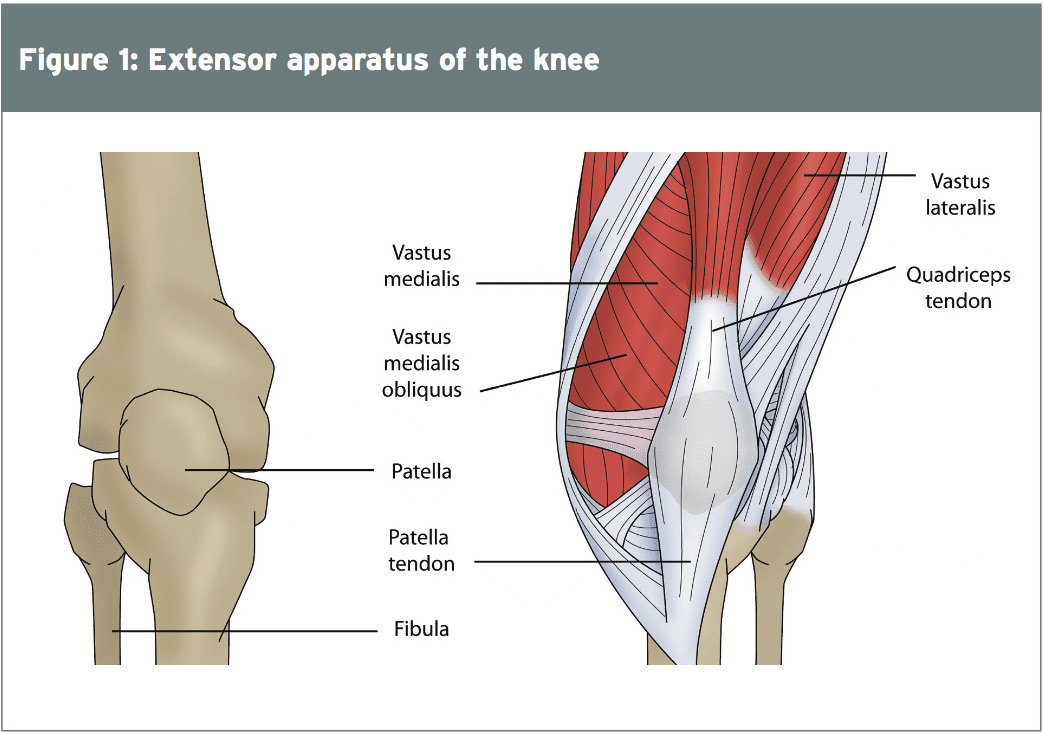
Vastus medialis (VM) is just one of four quadriceps muscles (rectus femoris, vastus medialis, vastus lateralis and vastus Intermedius) which creates the extensor Device of the knee (see Figure 1). All four components function as extensors of the knee, with the rectus femoris with the additional function of flexion of the hip. The four heads of the quadriceps offer varying levels of force production towards knee extension with the rectus femoris/vastus intermedius providing 35 percent of their pressure, the vastus lateralis supplying 40% and the vastus medialis providing 25 percent(7).
 The VM muscle arises from the medial Border of the linea asperalies on the anterior surface of the femur, and extends from approximately the lower end of the trochanteric line into the top third of the medial supracondylar line. It has a unique body in it ‘wraps’ around the femur from back to front(8). Moreover, it has been indicated the VM is split into two different components separated with a fascial plane)(9,10).
The VM muscle arises from the medial Border of the linea asperalies on the anterior surface of the femur, and extends from approximately the lower end of the trochanteric line into the top third of the medial supracondylar line. It has a unique body in it ‘wraps’ around the femur from back to front(8). Moreover, it has been indicated the VM is split into two different components separated with a fascial plane)(9,10).
- The exceptional or longitudinal Component (VML)
2. The oblique or inferior component (VMO)
The VMO originates partly from the The more proximal VML fibres run 15-20°medially and fit on the medial margin and anterior surface of the aponeurosis, which merges with the aponeurosis of the vastus intermedius muscle(14).
In their own cadaveric studies they didn’t locate a delineation between the VML and VMO fibres and no different facial plane was found between the muscles, indicating that these are not in fact two separate muscles. They also found that only a small number of fibres (22%) inserted directly on the actual patella with the vast majority of fibres terminating onto the quadriceps tendon. They argue that the VMO and VML are the exact same muscle based on their anatomical studies.
 Nevertheless, further evidence Indicating a differentiation between the VMO and VML was emphasized by studies that have discovered the VMO and VML have separate innervations. In a dissection study on 30 individual vastus medialis muscles and their nerves, it was revealed that a consistent bipartite nerve supply from the posterior division of the femoral nerve originated(17).
Nevertheless, further evidence Indicating a differentiation between the VMO and VML was emphasized by studies that have discovered the VMO and VML have separate innervations. In a dissection study on 30 individual vastus medialis muscles and their nerves, it was revealed that a consistent bipartite nerve supply from the posterior division of the femoral nerve originated(17).
A short and slim nerve referred to as The ‘lateral division’, provides the top lateral portion of the muscle. Another part, a ‘lateral division’, provides the centre and lower portion of the muscle. There’s an increase in the quantities of nerve fibres Providing the muscle as the muscular moves More distally, with the lowermost muscle fibres receiving the richest nerve source. This is supported by additional research that reveal that VMO and VML are electrophysiologically different entities(18,19).
Functional Roles Of VMO & VML
For several years, it has been believed that the primary job of the VMO is to not just contribute to knee extension torque but also to provide medial patella support from the trochlear groove of the femur during knee flexion and extension motions(9,21-29). It has been suggested that this muscle is the main active medial stabiliser of the patella, which counteracts the lateral pulling forces acting on the patella out of vastus lateralis (VL), the lateral retinaculum and the iliotibial tract(30).
Together with the knee at full extension, the patella is located over the trochlear groove. In this position, the patella has no underlying bone support in your natural ‘station’ formed by the trochlear groove and is therefore free to move medially and laterally.
Once the patella enters the trochlear groove, it gains stability in the medial and lateral direction by the bony margins of the trochlear groove. It’s thought that the VMO contributes to orientating the patella to the groove together with contracting during knee flexion. This mechanism seems counterintuitive when it’s known that the quadriceps are knee extensors. Throughout knee flexion that the quadriceps should stay relaxed since they are direct antagonists to the knee flexors such as the hamstrings.
This occurrence of VMO contraction through knee flexion was analyzed by researchers also it was discovered that in the healthy knee, the existence of obliquely oriented muscle fibers along with a medial tendon insertion site clarifies the modulation of forces acting on the patella as the knee goes out from extension to flexion.
Since the knee bends, a medially oriented (as opposed to superiorly orientated) pull from VMO could cause the patella to bend (or pull inferiorly, not superiorly) further and interpret in the medial, distal, and posterior directions relative the femur and its own trochlear groove(32). This type of pull would ‘drag’ the patella to the trochlea groove and create a secure patellofemoral joint.
These findings however pose the next obvious question: If those anatomical findings are observed in the ‘healthy’ knee, does this infer that these anatomical findings are not within knees with PFPS? That is, do patients develop PFPS due to altered morphology and anatomical structure as opposed as a result of real weakening of the VMO muscle?
A number of studies have highlighted the role which VMO plays in cutting patellofemoral compression forces — an important consideration in patients with patella chondral or osteochondral defects. In a different cadaveric research (and in most computational modelling studies) it had been determined that improving VMO function reduces the load carried from the lateral cartilage of the patellofemoral joint(36).
Increasing the pressure applied from the VMO consistently decreased the percentage of the joint compression put on the lateral cartilage and also always increased the maximum lateral strain. Moreover, this lateral compression reduction is even more evident from the existence of a lateral cartilage lesion, highlighting the value of VMO conditioning in reducing knee pain in people suffering from lateral compression problems with all the patella.
This study also revealed that the slight gain in the compression because the VMO induce increased contributed into the lateral pressure increase becoming more consistent than the lateral pressure reduction, even though the decline in the maximum lateral pressure was still important. When the VMO force was raised from the weak to strong scenarios the additional forces were decreased to keep a consistent expansion moment and minimize differences in compression (36,37). But many of these direct EMG, cadaveric and biomechanical computation studies have assessed the role of VMO in relation to VL in isolation, and in non-weight bearing conditions with motion of the femur constrained(38).
Powers et al (2003)(39) discovered that the patellofemoral kinematics change since the limb moves out of non-weight posture to weight-bearing positions. Additionally, isolation studies don’t consider the function of other physiological considerations like tibial torsion, valgus knee meltdown as a result of inadequate hip muscle control, overpronation of the rearfoot and midfoot, femoral anteversion abnormalities and inherent genu valgus(40).
Likewise, a decline in hip abductor and external rotator strength contributes to larger variance in hip-to-knee position during operational tasks(43). These may all contribute to monitoring problems and lateral patella compression forces, even at the presence of a functional VMO.
Furthermore, a number of these studies also use an experimental group that actually has knee pain. It may be possible that the knee pain itself changes lower limb kinetics and kinematics and isolated VMO into VL function.
Finally, additional more compelling factors at the hip and pelvis may result in abnormal patellofemoral loading, which then can cause the onset of patellofemoral pain syndromes. Frontal plane hip control (with abductors to protect against a Trendelenburg gait or rectal collapse) and sagittal plane control (using gluteals to restrain anterior pelvic tilt and following hip flexion moments) are critical to prevent aberrant movement, which might result in increases in joint compression and patellofemoral loading.
Conclusion
This article has highlighted exactly how difficult it can be to fully comprehend the authentic functional role that VMO performs in patellofemoral control. At best , we can simply presume that the VMO has a medial stabilization effect on the patella during knee flexion and extension movements. In part 2 nevertheless, we’ll discuss how VMO dysfunction does exist in the presence of knee pain — ie that VMO dysfunction might be the end result of knee pain, and not the true cause. However, the existence of VMO dysfunction alone alarms the therapists that some form of VMO re-strengthening may be necessary to fully rehabilitate the athlete with knee soreness.
References
1. Manual Therapy; 1996. 1:60-6.
2. Gend Med; 2008. 5:405–14.
3. British Journal of Sports Med; 2002. 36:95–101.
4. Clinical Journal of Sport Med; 1997. 7:28-31.
5. Sykes K and Wong YM (2001) Electrical activity of vastus medialis oblique muscle in straight leg raise exercise with different angle of hip rotation. Physiotherapy, 89: 423–430.
6. American Journal Physical Medicine Rehabilitation, 2001, 80: 804–808.
7. Journal of Orthopaedic Research; 1998.16:136–143.
8. Clinical Anat, 2005. 18(4), 281-289.
9. Orthopedics; 1980. 3:880-883.
10. Clinical Anat. 2009,22: 183–199.
11. International Research Journal of Biological Sciences. 2012. 1(5), 70-73.
12. Anat Rec. 1997, 249:135–142.
13. Journal of Bone and Joint Surgery [Am] A 1968. ;50:1535.
14. Aust Journal of Physiotherapy, 1997, 43: 277–281.
15. Surgical and Radiologic Anatomy. 1989. 11,17-22.
16. Journal of Arthroplasty; 2008. 23:600–604.
17. Journal of Anatomy. 1990. 170, pp. 193-198
18. Journal of Physical Therapy Science. 2014. 26: 101–104, 2014
19. Clinical Biomechanics. 2012 July ; 27(6):  525–531.
20. Journal of Anatomy. 1995. 187, pp. 403-411,
21. Physical Therapy; 1995. 75:672-683.
22. Müller W: The knee: form, function, and ligament reconstruction. Springer-Verlag,1983, pp 76–77.
23. Medicine and Science in Sports Exercise, 2007, 39: 1153–1159.
24. Journal of Bone and Joint Surgery. 53A, 1971. 749-758.
25. Clinical Biomechanics, 2000. 15(5), pp. 335–339.
26. Journal of Bone Joint Surgery Am; 1990.72:1424–1429.
27. American Journal of Sports Med. 2004. 30: 447–456.
28. British Journal of Sports Medicine. 2004.38: 295–299.
29. Orthop Clin North Am. 1992; 23:619–30.
30. Clinical Sports Med; 2010. 29:379-98.
31. Journal of Orthopaedic Research. 2009;27:561–570
32. Journal of Biomechanics. 2010 January 19; 43(2): 235
33. Journal of Bone and Joint Surgery [Br];1995. 77:225–231
34. Balcarek et al (2014) Vastus Medialis Obliquus Muscle Morphology in Primary and Recurrent Lateral Patellar Instability. Biomed Research International.
35. Knee Surgery, Sports Traumatology, Arthroscopy, 2012. 20(2). , pp. 331–336.
36. Journal of Orthopaedic Research; 2009. 27(5): 578–583.
37. Journal of Biomechanics. 2010; 43: 612-617.
38. Journal of orthopaedic & sports physical therapy. 2010. 40(2); 42-51.
39. Journal of Orthop Sports Phys Ther. 2003;33:677-685.
40. Journal of Orthop Sports Phys Ther; 1998. 28:345–54
41. Journal Orthop Research; 1988.6:499–508.
42. Physical Ther. 1995;75:24-30.
43. Physiother Res Int. 2009; http://dx.doi.org/10.1002/jor.2066310.1002/pri.449
Post Disclaimer
Professional Scope of Practice *
The information herein on "VMO: Patella Stabilization Key" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.