Automobile collisions, work, sports, and personal accidents can cause neck injuries that can affect other areas, leading to long-term health problems. Neck injuries involving soft tissue damage frequently persist after the incident. One of the injuries includes vocal cord damage caused by impact to the larynx. The larynx, or voicebox, is an organ that is behind the Adam’s apple. A neck injury impacting the larynx can affect the ability to speak and breathe and cause vocal cord paralysis. Treatment can involve surgery, voice therapy, physical therapy, and chiropractic.
Table of Contents
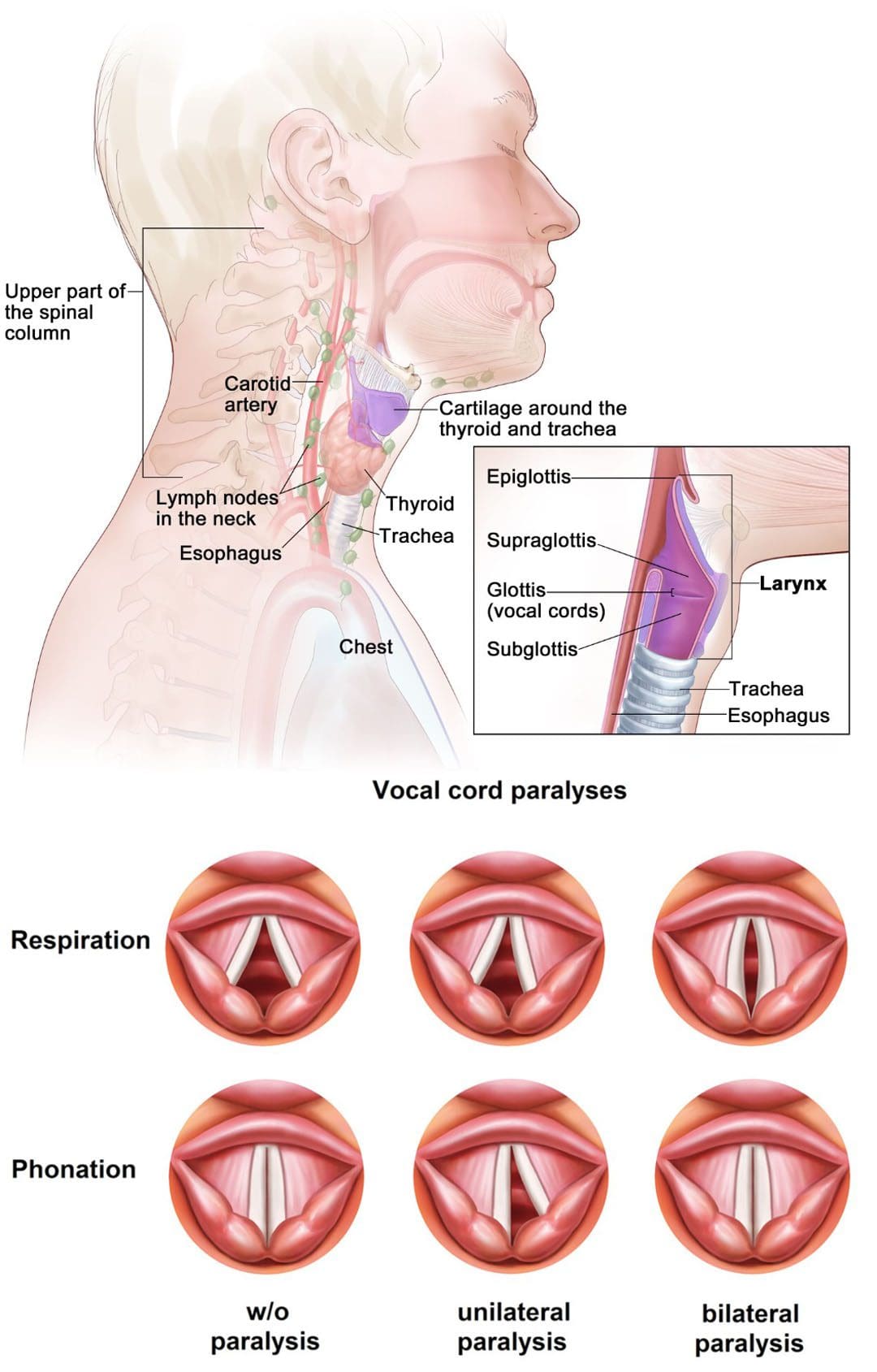
Vocal Cord Injury
The vocal cords are two flexible bands of muscle tissue at the entrance of the trachea. The vocal cords are normally in a relaxed open position to allow breathing. When talking, the bands combine and vibrate to make a sound. Surgery, viral infections, certain cancers, and neck trauma can cause vocal cord paralysis. In this condition, nerve damage blocks or inhibits impulses from transmitting to the voice box. The muscles, usually one of them, become paralyzed, preventing swallowing and ingesting saliva through the windpipe/trachea. In rare cases, both muscles are unable to move.
Symptoms
Signs and symptoms can include:
- Difficulty breathing
- Shortness of breath.
- Hoarse breathing.
- Noisy breathing.
- Speaking problems
- The need to take frequent breaths while speaking.
- Loss of vocal pitch.
- Inability to talk loudly.
- Trouble Swallowing
- Choking or coughing when swallowing.
- Loss of gag reflex.
- Frequent coughing and throat clearing.
Causes
Neck or Chest Injury
- Trauma to the neck or chest can injure the voice box nerves.
Infections
- Infections like Lyme disease, Epstein-Barr virus, and herpes can cause inflammation and nerve damage.
Tumors
- Tumors, cancerous and noncancerous, can grow inside or around the muscles, cartilage, and nerves.
Neurological
- Neurological conditions like multiple sclerosis or Parkinson’s disease can lead to vocal cord paralysis.
Surgical Injury
- Surgical procedure mistakes or complications on or near the neck or upper chest can result in damage to the voice box nerves.
- Surgeries to the thyroid or parathyroid glands, esophagus, neck, and chest have an increased risk.
Stroke
- A stroke chokes blood flow to the brain and can damage the region of the brain that transmits messages to the voice box.
Treatment
Treatment is determined by a doctor based on the individual medical condition and diagnostic tests. Treatment can involve:
Speech Therapy
Speech therapy is recommended as the laryngeal muscles are strengthened through various exercises, improving breathing function. A speech therapist will begin working with the individual on exercises targeting the weakened vocal folds by enhancing airflow and blood circulation.
Physical Therapy and Chiropractic
Treatment involves performing gentle exercises that work on the vocal cords gradually and progressively but does not stress them. Chiropractors work with the physical therapist performing high-velocity, low-amplitude manipulation targeted at the lower neck and upper thoracic area, the C3/T1 vertebrae. A treatment plan will also use massage, non-surgical decompression, instrument/tool-assisted soft-tissue mobilization, low laser or ultrasound, and at-home stretches and exercises.
Surgery
Surgery could be necessary for individuals experiencing no improvement despite doing the prescribed speech and physical therapy exercises. Different types of procedures are based on the degree and extent of the paralysis:
- Injections – Collagen and fillers are injected into the vocal cords to reposition the affected muscles closer to the larynx.
- Phonosurgery – The vocal cords are repositioned through restructuring.
- Tracheotomy – If the vocal folds are closing, a surgeon may make an incision in the neck at the opening of the windpipe and insert a breathing tube. This bypasses the air blockage caused by the vocal folds and promotes proper air circulation.
Cervical Spine Instability
References
Chen, Ching-Chang, et al. “Long-term result of vocal cord paralysis after anterior cervical discectomy.” The European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society vol. 23,3 (2014): 622-6. doi:10.1007/s00586-013-3084-y
Dankbaar JW, et al. Vocal cord paralysis: Anatomy, imaging, and pathology. Insights in Imaging. 2014; doi:10.1007/s13244-014-0364-y.
Fitzpatrick, P C, and R H Miller. “Vocal cord paralysis.” The Journal of the Louisiana State Medical Society: official organ of the Louisiana State Medical Society vol. 150,8 (1998): 340-3.
Kriskovich, M D et al. “Vocal fold paralysis after anterior cervical spine surgery: incidence, mechanism, and prevention of injury.” The Laryngoscope vol. 110,9 (2000): 1467-73. doi:10.1097/00005537-200009000-00011
Vocal fold paralysis. National Institute on Deafness and Other Communication Disorders. https://www.nidcd.nih.gov/health/vocal-fold-paralysis. Accessed May 18, 2022.
Vocal fold paralysis. American Speech-Language-Hearing Association. https://www.asha.org/public/speech/disorders/Vocal-Fold-Paralysis. Accessed May 18, 2022.
Waddell, Roger K. “Chiropractic care for a patient with spasmodic dysphonia associated with cervical spine trauma.” Journal of chiropractic medicine vol. 4,1 (2005): 19-24. doi:10.1016/S0899-3467(07)60108-6
Post Disclaimer
Professional Scope of Practice *
The information herein on "Vocal Cord Injury: EP Chiropractic Scientists" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.