Table of Contents
The Hidden Link Between Head Injuries and Sciatica: Causes, Effects, and Chiropractic Relief

Head injuries happen more often than you might think, from car crashes to sports accidents. They can shake up your brain and lead to problems far from your head, like pain in your lower back and legs. This pain is often called sciatica. Sciatica is when the sciatic nerve, the longest nerve in your body, gets irritated or pressed on. It starts in your lower spine and runs down through your hips, buttocks, and legs. When it’s bothered, you might feel sharp pain, numbness, or tingling that makes walking or sitting hard.
But how does a bump on the head connect to pain in your back? It turns out that head injuries, especially traumatic brain injuries (TBI), can mess with how your brain talks to the muscles in your spine. This can throw things out of balance and irritate the sciatic nerve. Head injuries can also make you more likely to hurt your spine later on. In some cases, they cause weird bone growth that squeezes the nerve. Severe injuries can even shift the bones in your upper neck, starting a chain of problems that ends up pressing on the sciatic nerve way down in your lower back.
The good news is that integrative chiropractic care can help. This type of care focuses on correcting spinal alignment, reducing inflammation, and optimizing the nervous system’s function. It might even help with the flow of a special fluid around your brain and spine. In this article, we’ll break it all down step by step. We’ll use simple words to explain the science, backed by real studies and expert views, including observations from Dr. Alexander Jimenez, a chiropractor and nurse practitioner with years of experience in treating injuries.
How Head Injuries Disrupt Brain Control of Spinal Muscles
Your brain is like the boss of your body. It sends signals through nerves to tell muscles what to do. The muscles in your spine help keep everything straight and supported. When you get a head injury, like a concussion or a more serious TBI, it can scramble those signals.
A concussion is a mild form of TBI where your brain gets jostled inside your skull. This can cause swelling and bruising of brain cells. The swelling increases pressure inside your head, which affects how nerves function (Physio Pretoria, n.d.). Your brain might not send the right messages to the muscles in your back. Those muscles could get too tight or too weak. When that happens, your spine may not stay properly aligned. Misaligned spine bones, called vertebrae, can pinch or irritate the sciatic nerve.
For example, if the muscles around your lower back spasm because of bad signals from the brain, they pull on the spine unevenly. This can lead to conditions like herniated disks, where the soft cushions between vertebrae bulge out and press on nerves (Arrowhead Clinic, n.d.). Sciatica pain shoots down your leg because the sciatic nerve is squeezed.
Studies show this connection. In one case, a person with TBI developed sciatica because their brain injury caused an “upper-motor nerve injury,” which affected how lower nerves worked (Lee et al., 2008). Upper-motor nerves are in the brain and spinal cord, and when they’re hurt, they can make muscles below them act funny. This includes the muscles that support your spine.
Dr. Alexander Jimenez, DC, APRN, FNP-BC, has seen this in his clinic. He notes that after head injuries, patients often have tight muscles and poor posture because the brain isn’t coordinating things right. He uses gentle adjustments to help fix this (Jimenez, n.d.).
Head injuries don’t just stop at one problem. They can make your whole body less stable. If your balance is affected by a concussion, you may move awkwardly and strain your back muscles more. Over time, this wear and tear adds up, irritating the sciatic nerve even further.
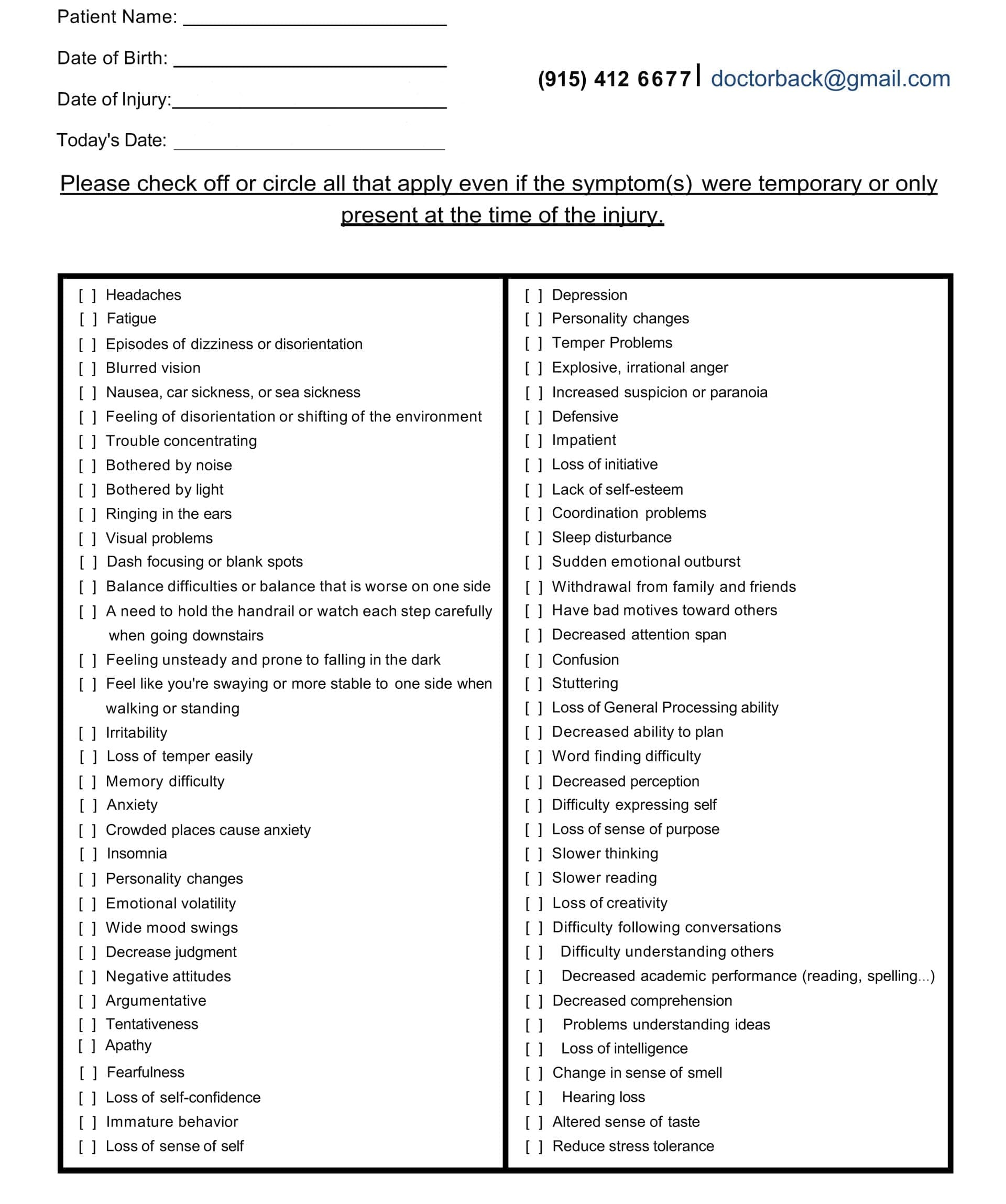
Head Injury/TBI Symptom Questionnaire:
Head Injuries and the Risk of More Spinal Problems
Once you’ve had a head injury, your chances of hurting your spine go up. Why? TBIs weaken your body’s defenses and change how you move.
Research on 236 people with TBI found that about 13% also had neck or spine injuries at the same time. Conditions such as brain bruises or bleeding increased the likelihood of spine problems (Sultan et al., 2022). Another study looked at people with moderate to severe TBIs. Those with low consciousness scores or other body injuries were at higher risk for spine damage (Soffler et al., 2011).
Head injuries make you clumsy or dizzy, so you’re more prone to falls or twists that hurt your back. The inflammation from a concussion spreads through your body, making tissues more sensitive (Nature, 2019). This can turn a minor spine issue into a major problem.
Severe head injuries can cause a “metabolic mismatch” where your brain doesn’t get enough energy. This affects how it controls posture and balance (Physio Pretoria, n.d.). Poor posture puts extra stress on your lower spine, where the sciatic nerve starts. Over weeks or months, this can lead to sciatica.
Dr. Jimenez observes that many patients with head injuries develop chronic back pain because their bodies compensate in unhealthy ways. He stresses checking the whole spine after any head trauma (Jimenez, n.d.).
Traumatic Brain Injury and Abnormal Bone Growth
One scary way TBIs cause sciatica is through something called heterotopic ossification (HO). This is when bone grows in places it shouldn’t, like soft tissues around your hips or nerves.
After a TBI, your body goes through swelling and tissue damage. This can trigger cells to turn into bone where they shouldn’t. In one reported case, a 22-year-old with TBI got HO around both hips, trapping the sciatic nerves on both sides (Lee et al., 2008). The new bone squeezed the nerves, causing pain and weakness.
HO occurs because the injury damages tissue and triggers inflammation. Factors like long surgeries or hip fractures worsen it, especially with TBI (Letournel et al., 2009). The bone grows slowly, so sciatica may not appear immediately. But over time, it narrows the space around the nerve, making it smaller and more irritated.
Studies show TBI boosts HO risk. The brain injury alters how your body heals, resulting in the formation of ectopic bone (extra bone outside the skeleton). This can encase the sciatic nerve, leading to “neuropathy” or nerve damage (Letournel et al., 2009).
Preventing HO with treatments like radiation or meds can help, but if it happens, surgery might be needed to free the nerve. However, sensory problems improve more than muscle strength after surgery.
Dr. Jimenez has treated patients with post-injury bone issues. He uses non-invasive methods to reduce inflammation early, which might lower HO risks (Jimenez, n.d.).
How Severe Head Injuries Worsen Sciatica Through Neck Misalignment
Severe head and brain injuries often jolt your whole body, especially the neck. The upper part of your neck, known as the cervical spine, can become misaligned. This starts a domino effect that reaches your lower back and sciatic nerve.
The top two bones in your neck, the atlas and axis, hold your head steady. A severe hit can misalign them. This misalignment, or subluxation, messes with nerve signals and blood flow (OK Precision Chiro, n.d.). It also alters the curvature of your spine, placing additional pressure on the lower back.
This chain reaction is similar to a wave: neck issues lead to shoulder tension, then mid-back strain, and ultimately, lower back compression. The lower spine bears extra weight, squeezing the sciatic nerve roots (Broadview Health Centre, n.d.).
Inflammation from the brain injury adds to this. Swollen brain tissues increase pressure, affecting the spinal cord connected to the neck (Physio Pretoria, n.d.). This can exacerbate sciatica, causing pain to radiate down the leg.
Research links TBI to pain sensitization. After TBI, your spine’s pain pathways get hyped up due to chemicals like chemokines (Sahbaie et al., 2019). This makes even small pressures on the sciatic nerve feel intense.
A study found that individuals with TBI experience more back and leg pain due to brain changes in areas that process pain (Govindarajan et al., 2016). Neck misalignment plays a big role in starting this.
Dr. Jimenez emphasizes upper cervical care. In his practice, he observes that correcting the neck can alleviate lower back pressure and sciatica symptoms (Jimenez, n.d.).
Integrative Chiropractic Care: A Path to Relief and Recovery
If you’re dealing with sciatica after a head injury, integrative chiropractic care might be a great option. This approach combines spinal adjustments with other therapies to address the root causes of the problem.
Chiropractors realign the spine to take pressure off nerves. For sciatica, this means adjusting the lower back to free the sciatic nerve (Dr. Kal, n.d.). It reduces inflammation and enhances the functioning of your nervous system.
For head injuries, chiropractic helps speed recovery. Adjustments restore cerebrospinal fluid (CSF) flow, which can get blocked by neck misalignments (Apex Chiro, n.d.). CSF is like a cushion and nutrient delivery system for your brain and spine. Better flow means less swelling and faster healing.
Techniques include gentle manipulations, massage, and exercises. These improve mobility, reduce pain, and boost brain-body communication (Calibration Mansfield, n.d.). One study has shown that chiropractic adjustments can change brain chemistry, reducing pain in the thalamus (YouTube, n.d.).
Chiropractic also tackles inflammation. By fixing alignments, it calms the body’s response, which is key after TBI (Zaker Chiro, n.d.).
Dr. Jimenez integrates chiropractic with functional medicine. He observes that combining adjustments with nutrition helps patients recover from TBI and sciatica faster. His plans address root causes, such as muscle imbalances (Jimenez, n.d.).
Other benefits include balancing the nervous system, addressing musculoskeletal issues, and enhancing circulation (Pinnacle Health Chiro, n.d.). For post-concussion syndrome, it eases headaches and dizziness (Team Allied PW, n.d.).
Compared to medication or surgery, chiropractic care is a non-invasive approach. It works well with other treatments (Addison Sports Clinic, n.d.).
In El Paso, clinics like Dr. Jimenez’s use advanced tools for personalized care (El Paso Chiro, n.d.).
Conclusion
Head injuries and sciatica are connected in ways that might surprise you. From disrupted muscle control to abnormal bone growth and neck misalignments, TBIs can lead to lasting nerve pain. But understanding this link is the first step to relief. Integrative chiropractic care offers hope by realigning your body, reducing inflammation, and restoring function. Experts like Dr. Jimenez show how personalized treatments can make a difference. If you’ve had a head injury and feel back pain, talk to a professional. Early care can help prevent more severe problems and help you get back to feeling good.
References
- Addison Sports Clinic. (n.d.). Chiropractic care for concussion recovery after car accidents
- Apex Chiro. (n.d.). How chiropractic care can treat a traumatic brain injury
- Arrowhead Clinic. (n.d.). Chiropractic treatment for sciatica relief: What you need to know
- Broadview Health Centre. (n.d.). Back pain connected to concussions
- Calibration Mansfield. (n.d.). How can integrative chiropractic care help with traumatic brain injuries
- Dr. Kal. (n.d.). Chiropractic care for sciatica after an accident
- El Paso Chiro. (n.d.). Chiropractic care in El Paso: Unlocking the secrets to recovery
- Govindarajan, K. A., Narayanan, M. D., & Widerström-Noga, E. G. (2016). Subacute pain after traumatic brain injury is associated with lower insular N-acetylaspartate concentrations
- Jimenez, A. (n.d.). Injury specialists
- Lee, J. H., Jun, H. S., Choi, S. H., Lim, M. K., Moon, M. S., & Kim, H. S. (2008). Bilateral sciatic nerve entrapment due to heterotopic ossification in a traumatic brain-injured patient
- Letournel, E., Judet, R., & Fassina, F. (2009). Sciatic nerve injury associated with acetabular fractures
- Nature. (2019). Mild traumatic brain injury causes nociceptive sensitization through spinal chemokine upregulation
- NW Health. (n.d.). Chiropractic economics: Chiropractic and traumatic brain injuries
- OK Precision Chiro. (n.d.). Upper cervical chiropractor OKC – Concussions & back pain link
- Physio Pretoria. (n.d.). Concussion
- Pinnacle Health Chiro. (n.d.). Six ways chiropractic care supports healing after TBI
- Sahbaie, P., Jang, Y., Irvine, K. A., & Clark, J. D. (2019). Mild traumatic brain injury causes nociceptive sensitization through spinal chemokine upregulation
- Soffler, C., Shaikh, Z., Wang, L., & Ahuja, C. S. (2011). Spinal cord injury and its association with blunt head trauma
- Sultan, M. J., Alqahtani, A. M., Alqahtani, M. M., & Alghamdi, A. M. (2022). Concurrent cranial and cervical spine injuries by associated injury mechanisms in traumatic brain injury patients
- Team Allied PW. (n.d.). The benefits of chiropractic care for post-concussion syndrome
- YouTube. (n.d.). Video on spinal manipulation and brain metabolites
- Zaker Chiro. (n.d.). Chiropractic care for head injury rehabilitation: Recovery after auto accidents
Post Disclaimer
Professional Scope of Practice *
The information herein on "The Hidden Link Between Head Injuries and Sciatica Symptoms" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.