Metabolic Syndrome:
Key indexing terms:
- Metabolic syndrome X
- Insulin resistance
- Hyperglycemia
- Inflammation
- Weight loss
Abstract
Objective: This article presents an overview of metabolic syndrome (MetS), which is a collection of risk factors that can lead to diabetes, stroke, and heart disease. The purposes of this article are to describe the current literature on the etiology and pathophysiology of insulin resistance as it relates to MetS and to suggest strategies for dietary and supplemental management in chiropractic practice.
Methods: The literature was searched in PubMed, Google Scholar, and the Web site of the American Heart Association, from the earliest date possible to May 2014. Review articles were identified that outlined pathophysiology of MetS and type 2 diabetes mellitus (T2DM) and relationships among diet, supplements, and glycemic regulation, MetS, T2DM, and musculoskeletal pain.
Results: Metabolic syndrome has been linked to increased risk of developing T2DM and cardiovascular disease and increased risk of stroke and myocardial infarction. Insulin resistance is linked to musculoskeletal complaints both through chronic inflammation and the effects of advanced glycosylation end products. Although diabetes and cardiovascular disease are the most well-known diseases that can result from MetS, an emerging body of evidence demonstrates that common musculoskeletal pain syndromes can be caused by MetS.
Conclusions: This article provides an overview of lifestyle management of MetS that can be undertaken by doctors of chiropractic by means of dietary modification and nutritional support to promote blood sugar regulation.
Table of Contents
Introduction: Metabolic Syndrome
Metabolic syndrome (MetS) has been described as a cluster of physical examination and laboratory findings that directly increases the risk of degenerative metabolic disease expression. Excess visceral adipose tissue, insulin resistance, dyslipidemia, and hypertension are conditions that significantly contribute to the syndrome. These conditions are united by a pathophysiological basis in low-grade chronic inflammation and increase an individual’s risk of cardiovascular disease, type 2 diabetes mellitus (T2DM), and all-cause mortality.1
The National Health and Nutrition Examination Survey (NHANES) 2003-2006 estimated that approximately 34% of United States adults aged 20 years and more had MetS.2 The same NHANES data found that 53% had abdominal adiposity, a condition that is closely linked to visceral adipose stores. Excess visceral adiposity generates increased systemic levels of pro-inflammatory mediator molecules. Chronic, low- grade inflammation has been well documented as an associated and potentially inciting factor for the development of insulin resistance and T2DM.1
NHANES 2003-2006 data showed that 39% of subjects met criteria for insulin resistance. Insulin resistance is a component of MetS that significantly contributes to the expression of chronic, low-grade inflammation and predicts T2DM expression. T2DM costs the United States in excess of $174 billion in 2007. 3 It is estimated that 1 in 4 adults will have T2DM by the year 2050.3 Currently, more than one third of US adults (34.9%) are obese, 4 and, in 2008, the annual medical cost of obesity was $147 billion.4,5 This clearly represents a health care concern.
The pervasiveness of MetS dictates that doctors of chiropractic will see a growing proportion of patients who fit the syndrome criteria.6 Chiropractic is most commonly used for musculoskeletal complaints believed to be mechanical in nature;6 however, an emerging body of evidence identifies MetS as a biochemical promoter of musculoskeletal complaints such as neck pain, shoulder pain, patella tendinopathy, and widespread musculoskeletal pain. 7–13 As an example, the cross-linking of collagen fibers can be caused by increased advanced glycation end-product (AGE) formation as seen in insulin resistance.14 Increased collagen cross-linking is observed in both osteoarthritis and degenerative disc disease, 15 and reduced mobility in elderly patients with T2DM has also been attributed to AGE-induced collagen cross-linking. 16,17
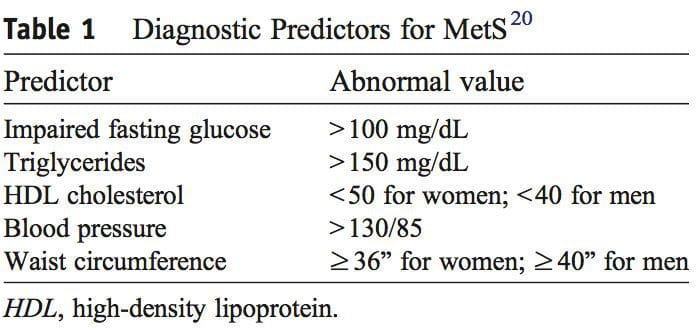
A diagnosis of MetS is made from a patient having 3 of the 5 findings presented in Table 1. Fasting hyperglycemia is termed impaired fasting glucose and indicates insulin resistance. 18,19 An elevated hemoglobin A1c (HbA1c) level measures long-term blood glucose regulation and is diagnostic for T2DM when elevated in the presence of impaired fasting glucose. 3,18
The emerging evidence demonstrates that we cannot view musculoskeletal pain as only coming from conditions that are purely mechanical in nature. Doctors of chiropractic must demonstrate prowess in identification and management of MetS and an understanding of insulin resistance as its main pathophysiological feature. The purposes of this article are to describe the current literature on the etiology and pathophysiology of insulin resistance as it relates to MetS and to suggest strategies for dietary and supplemental management in chiropractic practice.
Methods
 PubMed was searched from the earliest possible date to May 2014 to identify review articles that outlined the pathophysiology of MetS and T2DM. This led to further search refinements to identify inflammatory mechanisms that occur in the pancreas, adipose tissue, skeletal muscle, and hypothalamus. Searches were also refined to identify relationships among diet, supplements, and glycemic regulation. Both animal and human studies were reviewed. The selection of specific supplements was based on those that were most commonly used in the clinical setting, namely, gymnema sylvestre, vanadium, chromium and α-lipoic acid.
PubMed was searched from the earliest possible date to May 2014 to identify review articles that outlined the pathophysiology of MetS and T2DM. This led to further search refinements to identify inflammatory mechanisms that occur in the pancreas, adipose tissue, skeletal muscle, and hypothalamus. Searches were also refined to identify relationships among diet, supplements, and glycemic regulation. Both animal and human studies were reviewed. The selection of specific supplements was based on those that were most commonly used in the clinical setting, namely, gymnema sylvestre, vanadium, chromium and α-lipoic acid.
Discussion
Insulin Resistance Overview
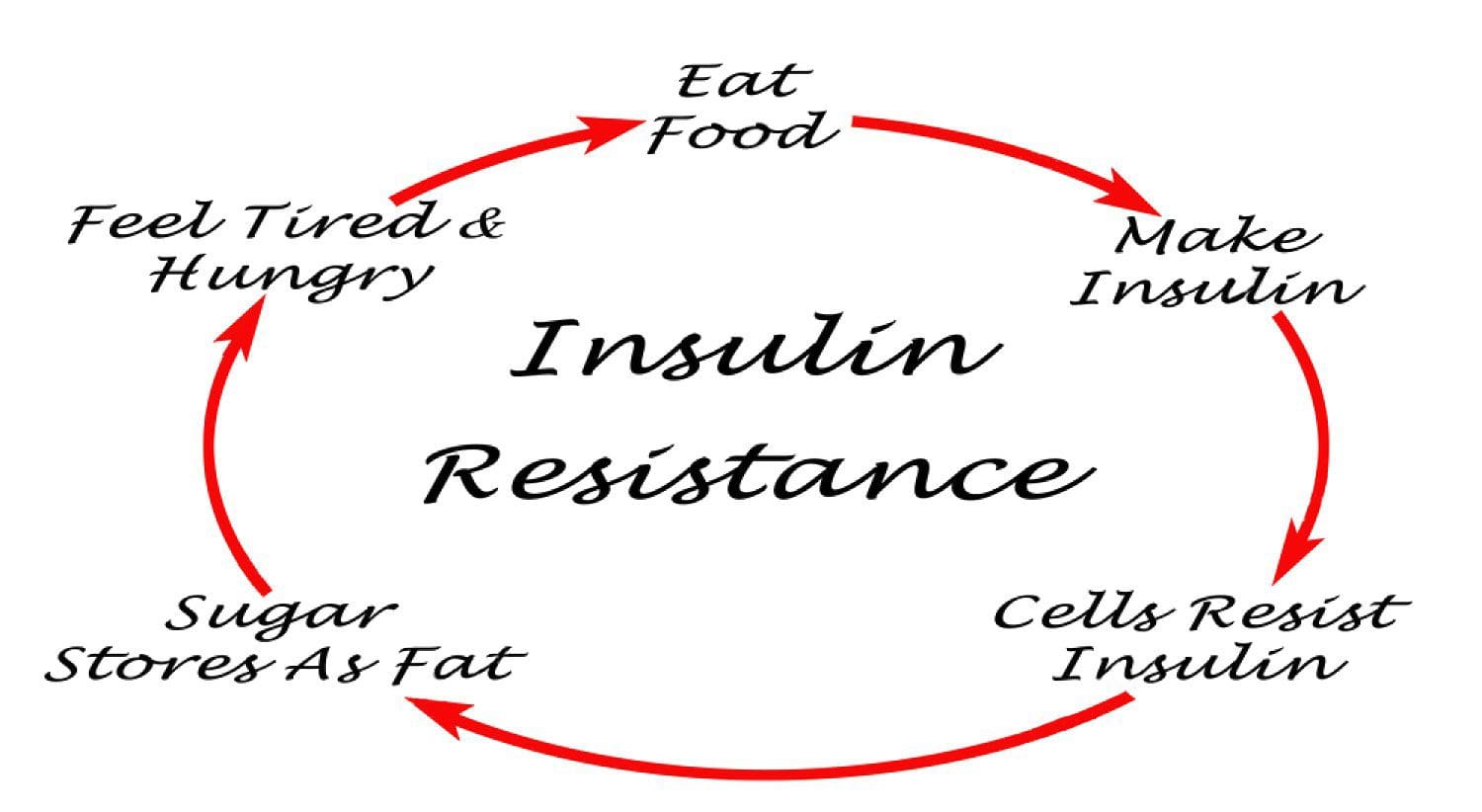 Under normal conditions, skeletal muscle, hepatic, and adipose tissues require the action of insulin for cellular glucose entry. Insulin resistance represents an inability of insulin to signal glucose passage into insulin-dependent cells. Although a genetic predisposition can exist, the etiology of insulin resistance has been linked to chronic low-grade inflammation.1 Combined with insulin resistance-induced hyperglycemia, chronic low-grade inflammation also sustains MetS pathophysiology.1
Under normal conditions, skeletal muscle, hepatic, and adipose tissues require the action of insulin for cellular glucose entry. Insulin resistance represents an inability of insulin to signal glucose passage into insulin-dependent cells. Although a genetic predisposition can exist, the etiology of insulin resistance has been linked to chronic low-grade inflammation.1 Combined with insulin resistance-induced hyperglycemia, chronic low-grade inflammation also sustains MetS pathophysiology.1
Two thirds of postprandial blood glucose metabolism occurs within skeletal muscle via an insulin-dependent mechanism.18,19 Insulin binding to its receptor triggers glucose entry and subsequently inhibits lipolysis within the target tissue.21,22 Glucose enters skeletal muscles cells by way of a glucose transporter designated Glut4. 18 Owing to genetic variability, insulin-mediated glucose uptake can vary more than 6-fold among non-diabetic individuals. 23
Prolonged insulin resistance leads to structural changes within skeletal muscle such as decreased Glut4 transporter number, intramyocellular fat accu- mulation, and a reduction in mitochondrial con- tent.19,24 These events are thought to impact energy generation and functioning of affected skeletal mus- cle.24 Insulin-resistant skeletal muscle is less able to suppress lipolysis in response to insulin binding.25 Subsequently, saturated free fatty acids accumulate and generate oxidative stress. 22 The same phenomenon within adipose tissue generates a rapid adipose cell expansion and tissue hypoxia.26 Both these processes increase inflammatory pathway activation and the generation of proinflammatory cytokines (PICs).27
Multiple inflammatory mediators are associated with the promotion of skeletal muscle insulin resistance. The PICs tumor necrosis factor α (TNF-α), interleukin 1 (IL- 1), and IL-6 have received much attention because of their direct inhibition of insulin signaling.28–30 Since cytokine testing is not performed clinically, elevated levels of high- sensitivity C-reactive protein (hsCRP) best represent the low-grade systemic inflammation that characterizes insulin resistance.31,32
Insulin resistance–induced hyperglycemia can lead to irreversible changes in protein structure, termed glycation, and the formation of AGEs. Cells such as those of the vascular endothelium are most vulnerable to hyperglycemia due to utilization of an insulin-independent Glut1 transporter. 33 This makes AGE generation responsible for most diabetic complications, 15,33,34 including collagen cross-linking.15
If unchanged, prolonged insulin resistance can lead to T2DM expression. The relationship between chronic low-grade inflammation and T2DM has been well characterized. 35 Research has demonstrated that patients with T2DM also have chronic inflammation within the pancreas, termed insulitis, and it worsens hyperglycemia due to the progressive loss of insulin- producing β cells.36–39
Visceral Adiposity And Insulin Resistance
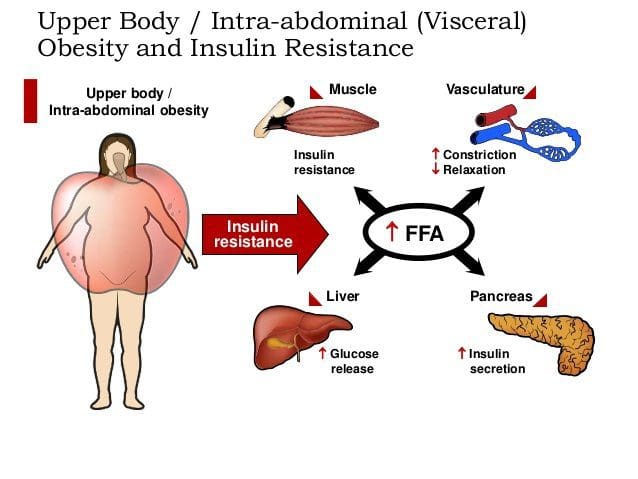 Caloric excess and a sedentary lifestyle contribute to the accumulation of subcutaneous and visceral adipose tissue. Adipose tissue was once thought of as a metabolically inert passive energy depot. A large body of evidence now demonstrates that excess visceral adipose tissue acts as a driver of chronic low-grade inflammation and insulin resistance.27,34
Caloric excess and a sedentary lifestyle contribute to the accumulation of subcutaneous and visceral adipose tissue. Adipose tissue was once thought of as a metabolically inert passive energy depot. A large body of evidence now demonstrates that excess visceral adipose tissue acts as a driver of chronic low-grade inflammation and insulin resistance.27,34
It has been documented that immune cells infiltrate rapidly expanding visceral adipose tissue. 26,40 Infil- trated macrophages become activated and release PICs that ultimately cause a phenotypic shift in resident macrophage phenotype to a classic inflammatory M1 profile.27 This vicious cycle creates a chronic inflam- matory response within adipose tissue and decreases the production of adipose-derived anti-inflammatory cytokines.43 As an example, adiponectin is an adipose- derived anti-inflammatory cytokine. Macrophage- invaded adipose tissue produces less adiponectin, and this has been correlated with increasing insulin resistance. 26
Hypothalamic Inflammation And Insulin Resistance
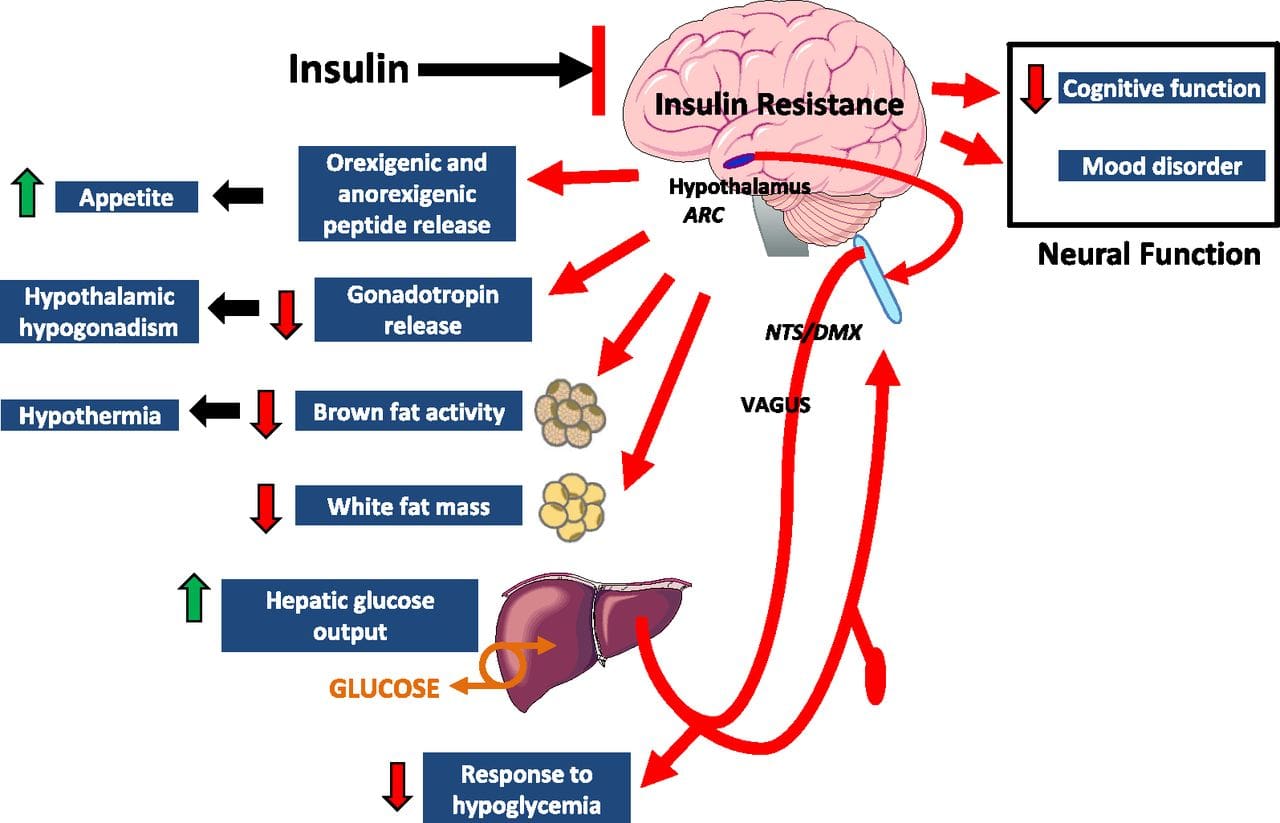 Eating behavior in the obese and overweight has been popularly attributed to a lack of will power or genetics. However, recent research has demonstrated a link between hypothalamic inflammation and increased body weight.41,41
Eating behavior in the obese and overweight has been popularly attributed to a lack of will power or genetics. However, recent research has demonstrated a link between hypothalamic inflammation and increased body weight.41,41
Centers that govern energy balance and glucose homeostasis are located within the hypothalamus. Recent studies demonstrate that inflammation in the hypothalamus coincides with metabolic inflammation and an increase in appetite.43 These hypothalamic centers simultaneously become resistant to anorexigenic stimuli, leading to altered energy intake. It has been suggested that this provides a neuropathological basis for MetS and drives a progressive increase in body weight. 41
Central metabolic inflammation pathologically activates hypothalamic immune cells and disrupts central insulin and leptin signaling.41 Peripherally, this has been associated with dysregulated glucose homeostasis that also impairs pancreatic β cell functioning.41,44 Hypothalamic inflammation contributes to hypertension through similar mechanisms, and it is thought that central inflammation parallels chronic low-grade systemic inflammation and insulin resistance.41–44
Clinical Correlates Diet-Induced Inflammation & Insulin Resistance
 Feeding generally leads to a short-term increase in both oxidative stress and inflammation. 41 Total calories consumed, glycemic index, and fatty acid profile of a meal all influence the degree of postprandial inflammation. It is estimated that the average American consumes approximately 20% of calories from refined sugar, 20% from refined grains and flour, 15% to 20% from excessively fatty meat products, and 20% from refined seed/legume oils.45 This pattern of eating contains a macronutrient composition and glycemic index that promote hyperglycemia, hyperlipemia, and an acute postprandial inflammatory response. 46 Collectively referred to as postprandial dysmetabolism, this pro-inflammatory response can sustain levels of chronic low-grade inflammation that leads to excess body fat, coronary heart disease (CHD), insulin resistance, and T2DM.28,29,47
Feeding generally leads to a short-term increase in both oxidative stress and inflammation. 41 Total calories consumed, glycemic index, and fatty acid profile of a meal all influence the degree of postprandial inflammation. It is estimated that the average American consumes approximately 20% of calories from refined sugar, 20% from refined grains and flour, 15% to 20% from excessively fatty meat products, and 20% from refined seed/legume oils.45 This pattern of eating contains a macronutrient composition and glycemic index that promote hyperglycemia, hyperlipemia, and an acute postprandial inflammatory response. 46 Collectively referred to as postprandial dysmetabolism, this pro-inflammatory response can sustain levels of chronic low-grade inflammation that leads to excess body fat, coronary heart disease (CHD), insulin resistance, and T2DM.28,29,47
Recent evidence suggests that several MetS criteria may not sufficiently identify all individuals with postprandial dysmetabolism. 48,49 A 2-hour oral glucose tolerance test (2-h OGTT) result greater than 200 mg/dL can be used clinically to diagnose T2DM. Although MetS includes a fasting blood glucose level less than 100 mg/dL, population studies have shown that a fasting glucose as low as 90 mg/dL can be associated with an 2-h OGTT level greater than 200 mg/dL.49 Further, a recent large cohort study indicated that an increased 2-h OGTT was independently predictive of cardiovascular and all-cause mortality in a nondiabetic population. 48 Mounting evidence indicates that post- prandial glucose levels are better correlated with MetS and predicting future cardiovascular events than fasting blood glucose alone.41,48
Fasting triglyceride levels generally correlate with postprandial levels, and a fasting triglyceride level greater than 150 mg/dL reflects MetS and insulin resistance. Contrastingly, epidemiologic data indicate that a fasting triglyceride level greater than 100 mg/dL influences CHD risk via postprandial dysmetabolism. 48 The acute postprandial inflammatory response that contributes to CHD risk includes an increase in PICs, free radicals, and hsCRP.48,49 These levels are not measured clinically but, monitoring fasting glucose, 2-hour postprandial glucose and fasting triglycerides can be used as correlates of postprandial dysmetabolic and low-grade systemic inflammation.
MetS And Disease Expression
 Diagnosis of MetS has been linked to an increased risk of developing T2DM and cardiovascular disease over the following 5 to 10 years. 1 It further increases a patient’s risk of stroke, myocardial infarction, and death from any of the aforementioned conditions.1
Diagnosis of MetS has been linked to an increased risk of developing T2DM and cardiovascular disease over the following 5 to 10 years. 1 It further increases a patient’s risk of stroke, myocardial infarction, and death from any of the aforementioned conditions.1
Facchini et al47 followed 208 apparently healthy, non-obese subjects for 4 to 11 years while monitoring the incidence of clinical events such as hypertension, stroke, CHD, cancer, and T2DM. Approximately one fifth of participants experienced clinical events, and all of these subjects were either classified as intermediately or severely insulin resistant. It is important to note that all of these clinical events have a pathological basis in chronic low-grade inflammation,50 and no events were experienced in the insulin-sensitive groupings. 47
Insulin resistance is linked to musculoskeletal com- plaints both through chronic inflammation and the effects of AGEs. Advanced glycation end-products have been shown to extensively accumulate in osteoarthritic cartilage and treatment of human chondrocytes with AGEs increased their catabolic activity. 51 Advanced glycation end-products increase collagen stiffness via cross-linking and likely contribute to reduced joint mobility seen in elderly patients with T2DM.52 Com- pared to non-diabetics, type II diabetic patients are known to have altered proteoglycan metabolism in their intervertebral discs. This altered metabolism may pro- mote weakening of the annular fibers and subsequently, disc herniation.53 The presence of T2DM increases a person’s risk of expressing disc herniation in both the cervical and lumbar spines.17,54 Patients with T2DM are also more likely to develop lumbar stenosis compared with non-diabetics, and this has been documented as a plausible relationship between MetS risk factors and physician-diagnosed lumbar disc herniation. 55–57
There are no specific symptoms that denote early skeletal muscle structural changes. Fatty infiltration and decreased muscle mitochondria content are observed within age-related sarcopenia 58 ; however, it is still being argued whether fatty infiltration is a risk factor for low back pain. 59,60
Clinical management of MetS should be geared toward improving insulin sensitivity and reducing chronic low-grade inflammation. 1 Regular exercise without weight loss is associated with reduced insulin resistance, and at least 30 minutes of aerobic activity and resistance training is recommended daily. 61,62 Although frequently considered preventative, exercise, dietary, and weight loss interventions should be considered alongside pharmacological management in those with MetS. 1
Data regarding the exact amount of weight loss needed to improve chronic inflammation are inconclusive. In overweight individuals without diagnosed MetS, a very-low-carbohydrate diet (b 10% calories from carbohydrate) has significantly reduced plasma inflammatory markers (TNF-α, hsCRP, and IL-6) with as little as 6% reduction in body weight.63,64 Individuals who meet MetS criteria may require 10% to 20% body weight loss to reduce inflammatory markers. 65 Interestingly, the Mediterranean Diet has been shown to reduce markers of systemic inflammation independent of weight loss65 and was recommended in the American College of Cardiology and American Heart Association Adult Treatment Panel 4 guidelines.66
A growing body of research has examined the effects of the Spanish ketogenic Mediterranean diet, including olive oil, green vegetables and salads, fish as the primary protein, and moderate red wine consumption. In a sample of 22 patients, adoption of the Spanish ketogenic Mediterranean diet with 9 g of supplemental salmon oil on days when fish was not consumed has led to complete resolution of MetS.67 Significant reductions in markers of chronic systemic inflammation were seen in 31 patients following this diet for 12 weeks.68
A Paleolithic diet based on lean meat, fish, fruits, vegetables, root vegetables, eggs, and nuts has been described as more satiating per calorie than a diabetes diet in patients with T2DM.69 In a randomized crossover study, a Paleolithic diet resulted in lower mean HbA1c values, triglycerides, diastolic blood pressure, waist circumference, improved glucose tolerance, and higher high-density lipoprotein (HDL) values compared to a diabetes diet.70 Within the context of these changes, a referral for medication management may be advisable.
Irrespective of name, a low-glycemic diet that focuses on vegetables, fruits, lean meats, omega-3 fish, nuts, and tubers can be considered anti-inflammatory and has been shown to ameliorate insulin resistance. 49,71–73 Inflammatory markers and insulin resistance further improve when weight loss coincides with adherence to an anti-inflammatory diet.70 A growing body of evidence suggests that specific supplemental nutrients also reduce insulin resistance and improve chronic low-grade inflammation.
Key Nutrients That Promote Insulin Sensitivity
 Research has identified nutrients that play key roles in promoting proper insulin sensitivity, including vitamin D, magnesium, omega-3 (n-3) fatty acids, curcumin, gymnema, vanadium, chromium, and α-lipoic acid. It is possible to get adequate vitamin D from sun exposure and adequate amounts of magnesium and omega-3 fatty acids from food. Contrastingly, the therapeutic levels of chromium and α-lipoic acid that affect insulin sensitivity and reduce insulin resistance cannot be obtained in food and must be supplemented.
Research has identified nutrients that play key roles in promoting proper insulin sensitivity, including vitamin D, magnesium, omega-3 (n-3) fatty acids, curcumin, gymnema, vanadium, chromium, and α-lipoic acid. It is possible to get adequate vitamin D from sun exposure and adequate amounts of magnesium and omega-3 fatty acids from food. Contrastingly, the therapeutic levels of chromium and α-lipoic acid that affect insulin sensitivity and reduce insulin resistance cannot be obtained in food and must be supplemented.
Vitamin D, Magnesium, Omega-3 Fatty Acids, & Curcumin
 Vitamin D, magnesium, and n-3 fatty acids have multiple functions, and generalized inflammation reduction is a common mechanism of action.74–80 Their supplemental use should be considered in the context of low-grade inflammation reduction and health promotion, rather than as a specific treatment for MetS or T2DM.
Vitamin D, magnesium, and n-3 fatty acids have multiple functions, and generalized inflammation reduction is a common mechanism of action.74–80 Their supplemental use should be considered in the context of low-grade inflammation reduction and health promotion, rather than as a specific treatment for MetS or T2DM.
Evidence pertaining to the precise role of vitamin D in MetS and insulin resistance is inconclusive. Increas- ing dietary and supplemental vitamin D intake in young men and women may lower the risk of MetS and T2DM development,81 and a low serum vitamin D level has been associated with insulin resistance and T2DM expression. 82 Supplementation to improve low serum vitamin D (reference range, 32-100 ng/mL) is effective, but its impact on improving central glycemia and insulin sensitivity is conflicting. 83 Treating insulin resistance and MetS with vitamin D as a monotherapy appears to be unsuccessful. 82,83 Achieving normal vitamin D blood levels through adequate sun exposure and/or supplementation is advised for general health. 84–86
The average American diet commonly contains a low magnesium intake.80 Recent studies suggest that supple- mental magnesium can improve insulin sensitivity. 81,82 Taking 365 mg/d may be effective in reducing fasting glucose and raising HDL cholesterol in T2DM,83 as well as normomagnesemic, overweight, nondiabetics. 84
Diets high in the omega-6 fat linoleic acid have been associated with insulin resistance85 and higher levels of serum pro-inflammatory mediator markers including IL-6, IL-1β, TNF-α, and hsCRP.87 Supplementation to increase dietary omega-3 fatty acids at the expense of omega-6 fatty acids has been shown to improve insulin sensitivity. 88–90 Six months of omega-3 supplementation at 3 g/d with meals has been shown to reduce MetS markers including fasting triglycerides, HDL cholesterol, and an increase in anti-inflammatory adiponectin. 91
Curcumin is responsible for the yellow pigmentation of the spice turmeric. Its biological effects can be characterized as antidiabetic and antiobesity via down- regulating TNF-α, suppressing nuclear factor κB activation, adipocytokine expression, and leptin level modulation,. 92–95 Curcumin has been reported to activate peroxisome proliferator-activated receptor-γ, the nuclear target of the thiazolidinedione class of antidiabetic drugs,93 and it also protects hepatic and pancreatic cells. 92,93 Numerous studies have reported weight loss, hsCRP reduction, and improved insulin sensitivity after curcumin supplementation.92–95
There is no established upper limit for curcumin, and doses of up to 12 g/d are safe and tolerable in humans. 96 A randomized, double-blinded, placebo- controlled trial (N = 240) showed a reduced progression of prediabetes to T2DM after 9 months of 1500 mg/d curcumin supplementation.97
Curcumin, 98 vitamin D, 84 magnesium, 91 and omega-3 fatty acids80 are advocated as daily supplements to promote general health. A growing body of evidence supports the views of Gymnema sylvestre, vanadium, chromium, and α-lipoic acid should as therapeutic supplements to assist in glucose homeostasis.
G Sylvestre
 Gymnemic acids are the active component of the G sylvestre plant leaves. Gymnemic acids are the active component of the G sylvestre plant leaves. Studies evaluating G sylvestre’s effects on diabetes in humans have generally been of poor methodological quality. Experimental animal studies have found that gymnemic acids may decrease glucose uptake in the small intestine, inhibit gluconeogenesis, and reduce hepatic and skeletal muscle insulin resistance.99 Other animal studies suggest that gymnemic acids may have comparable efficacy in reducing blood sugar levels to the first-generation sulfonylurea, tolbutamide.100
Gymnemic acids are the active component of the G sylvestre plant leaves. Gymnemic acids are the active component of the G sylvestre plant leaves. Studies evaluating G sylvestre’s effects on diabetes in humans have generally been of poor methodological quality. Experimental animal studies have found that gymnemic acids may decrease glucose uptake in the small intestine, inhibit gluconeogenesis, and reduce hepatic and skeletal muscle insulin resistance.99 Other animal studies suggest that gymnemic acids may have comparable efficacy in reducing blood sugar levels to the first-generation sulfonylurea, tolbutamide.100
Evidence from open-label trials suggests its use as a supplement to oral antidiabetic hypoglycemic agents. 96 One quarter of patients were able to discontinue their drug and maintain normal glucose levels on an ethanolic gymnema extract alone. Although the evidence to date suggests its use in humans and animals is safe and well tolerated, higher quality human studies are warranted.
Vanadyl Sulfate
 Vanadyl sulfate has been reported to prolong the events of insulin signaling and may actually improve insulin sensitivity.101 Limited data suggest that it inhibits gluconeogenesis, possibly ameliorating hepatic insulin resistance. 100,101 Uncontrolled clinical trials have reported improvements in insulin sensitivity using 50 to 300 mg daily for periods ranging from 3 to 6 weeks. 101–103 Contrastingly, a recent randomized, double-blind, placebo-controlled trial found that 50 mg of vanadyl sulfate twice daily for 4 weeks had no effect in individuals with impaired glucose tolerance. 104 Limited clinical and experimental data exist supporting the use of vanadyl sulfate to improve insulin resistance, and further research is warranted regarding its safety and efficacy.
Vanadyl sulfate has been reported to prolong the events of insulin signaling and may actually improve insulin sensitivity.101 Limited data suggest that it inhibits gluconeogenesis, possibly ameliorating hepatic insulin resistance. 100,101 Uncontrolled clinical trials have reported improvements in insulin sensitivity using 50 to 300 mg daily for periods ranging from 3 to 6 weeks. 101–103 Contrastingly, a recent randomized, double-blind, placebo-controlled trial found that 50 mg of vanadyl sulfate twice daily for 4 weeks had no effect in individuals with impaired glucose tolerance. 104 Limited clinical and experimental data exist supporting the use of vanadyl sulfate to improve insulin resistance, and further research is warranted regarding its safety and efficacy.
Chromium
 Diets high in refined sugar and flour are deficient in chromium (Cr) and lead to an increased urinary excretion of chromium. 105,106 The progression of MetS is not likely caused by a chromium deficiency, 107 and dosages that benefit glycemic regulation are not achievable through food. 106,108,109
Diets high in refined sugar and flour are deficient in chromium (Cr) and lead to an increased urinary excretion of chromium. 105,106 The progression of MetS is not likely caused by a chromium deficiency, 107 and dosages that benefit glycemic regulation are not achievable through food. 106,108,109
A recent randomize, double-blind trial demonstrated that 1000 μg Cr per day for 8 months improved insulin sensitivity by 10% in subjects with T2DM.110 Cefalu et al110 further suggested that these improvements might be more applicable to patients with a greater degree of insulin resistance, impaired fasting plasma glucose, and higher HbA1c values. Chromium’s mechanism of action for improving insulin sensitivity is through increased Glut4 translocation via prolonging insulin receptor signaling.109 Chromium has been well tolerated at 1000 μg/d,105 and animal models using significantly more than 1000 μ Cr per day were not associated with toxicological consequences.109
α-Lipoic Acid
 Humans derive α-lipoic acid through dietary means and from endogenous synthesis. 111 The foods richest in α-lipoic acid are animal tissues with extensive metabolic activity such as animal heart, liver, and kidney, which are not consumed in large amounts in the typical American diet. 111 Supplemental amounts of α-lipoic acid used in the treatment of T2DM (300-600 mg) are likely to be as much as 1000 times greater than the amounts that could be obtained from the diet.112
Humans derive α-lipoic acid through dietary means and from endogenous synthesis. 111 The foods richest in α-lipoic acid are animal tissues with extensive metabolic activity such as animal heart, liver, and kidney, which are not consumed in large amounts in the typical American diet. 111 Supplemental amounts of α-lipoic acid used in the treatment of T2DM (300-600 mg) are likely to be as much as 1000 times greater than the amounts that could be obtained from the diet.112
Lipoic acid synthase (LASY) appears to be the key enzyme involved in the generation of endogenous lipoic acid, and obese mice with diabetes have reduced LASY expression when compared with age-and sex- matched controls.111 In vitro studies to identify potential inhibitors of lipoic acid synthesis suggest a role for diet-induced hyperglycemia and the PIC TNF- α in the down-regulation of LASY.113 The inflammatory basis of insulin resistance may therefore drive lowered levels of endogenous lipoic acid via reducing the activity of LASY.
α-Lipoic acid has been found to act as insulin mimetic via stimulating Glut4-mediated glucose trans- port in muscle cells. 110,114α-Lipoic acid is a lipophilic free radical scavenger and may affect glucose homeostasis through protecting the insulin receptor from damage114 and indirectly via decreasing nuclear factor κB–mediated TNF-α and IL-1 production. 110 In postmenopausal women with MetS (presence of at least 3 ATPIII clinical criteria) 4 g/d of a combined inositol and α-lipoic acid supplement for 6 months significantly improved OGTT scores by 20% in two thirds of the subjects. 114 A recent randomized double-blinded placebo-controlled study showed that 300 mg/d α- lipoic acid for 90 days significantly decreased HbA1c values in subjects with T2DM.115
Side effects to α-lipoic acid supplementation as high as 1800 mg/d have largely been limited to nausea. 116 It may be best to take supplemental α-lipoic acid on an empty stomach (1 hour before or 2 hours after eating) because food intake reportedly reduces its bioavailability.117 Clinicians should be aware that α-lipoic acid supplementation might increase the risk of hypoglycemia in diabetic patients using insulin or oral antidiabetic agents.117
Limitations
 This is a narrative overview of the topic of MetS. A systematic review was not performed; therefore, there may be relevant information missing from this review. The contents of this overview focuses on the opinions of the authors, and therefore, others may disagree with our opinions or approaches to management. This overview is limited by the studies that have been published. To date, no studies have been published that identify the effectiveness of a combination of a dietary intervention, such as the Spanish ketogenic diet, and nutritional supplementation on the expression of the MetS. Similarly, this approach has not been studied in patients with musculoskeletal pain who also have the MetS. Consequently, the information presented in this article is speculative. Longitudinal studies are needed before any specific recommendations can be made for patients with musculoskeletal that may be influenced by the MetS.
This is a narrative overview of the topic of MetS. A systematic review was not performed; therefore, there may be relevant information missing from this review. The contents of this overview focuses on the opinions of the authors, and therefore, others may disagree with our opinions or approaches to management. This overview is limited by the studies that have been published. To date, no studies have been published that identify the effectiveness of a combination of a dietary intervention, such as the Spanish ketogenic diet, and nutritional supplementation on the expression of the MetS. Similarly, this approach has not been studied in patients with musculoskeletal pain who also have the MetS. Consequently, the information presented in this article is speculative. Longitudinal studies are needed before any specific recommendations can be made for patients with musculoskeletal that may be influenced by the MetS.
Conclusion: Metabolic Syndrome
This overview suggests that MetS and type 2 diabetes are complex conditions, and their prevalence is expected to increase substantially in the coming years. Thus, it is important to identify if the MetS may be present in patients who are nonresponsive to manual care and to help predict who may not respond adequately.
We suggest that diet and exercise are essential to managing these conditions, which can be supported with key nutrients, such as vitamin D, magnesium, and omega-3 fatty acids. We also suggest that curcumin, G sylvestre, vanadyl sulfate chromium, and α-lipoic acid could be viewed as specific nutrients that may be taken during the process of restoring appropriate insulin sensitivity and signaling.
Chiropractic Care
David R. Seaman DC, MS,âŽ, Adam D. Palombo DC
Professor, Department of Clinical Sciences, National University of Health Sciences, Pinellas Park, FL Private Chiropractic Practice, Newburyport, MA
Funding Sources and Conflicts of Interest
No funding sources were reported for this study. David Seaman is a paid consultant for Anabolic Laboratories, a manufacturer of nutritional products for health care professionals. Adam Palombo was sponsored and remunerated by Anabolic laboratories to speak at chiropractic conventions/meetings.
1. Kaur J. A comprehensive review on metabolic syndrome.
Cardiol Res Pract 2014:943162, http://dx.doi.org/10.1155/
2014/943162.
2. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic
syndrome among US adults. Findings from the Third National
Health and Nutrition Examination Survey. J Am Med Assoc
2006;287:356–9.
3. Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson
DF. Projection of the year 2050 burden of diabetes in the US
adult population: dynamic modeling of incidence, mortality,
and prediabetes prevalence. Popul Health Metr 2010;8:29,
http://dx.doi.org/10.1186/1478-7954-8-29.
4. [Internet]Centers for Disease Control and Prevention.
Adult Obesity Facts. Atlanta: CDC; 2014. [Available from
http://www.cdc.gov/obesity/data/adult.html].
5. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of
childhood and adult obesity in the United States, 2011–2012.
JAMA 2014;311(8):806–14.
6. Riksman JS, Williamson OD, Walker BF. Delineating
inflammatory and mechanical sub-types of low back pain: a
pilot survey of fifty low back pain patients in a chiropractic
setting. Chiropr Man Therap 2011;19(1):5, http://dx.doi.org/
10.1186/2045-709X-19-5.
7. Dobretsov M, Ghaleb AH, Romanovsky D, Pablo CS, Stimers
JR. Impaired insulin signaling as a potential trigger of
pain in diabetes and prediabetes. Int Anesthesiol Clin
2007;45(2):95–105.
8. Mantyselka P, Miettola J, Niskanen L, Kumpusalo E. Glucose
regulation and chronic pain at multiple sites. Rheumatology
2008;47(8):1235–8.
9. Mäntyselkä P, Miettola J, Niskanen L, Kumpusalo E.
Persistent pain at multiple sites—connection to glucose
derangement. Diabetes Res Clin Pract 2009;84(2):e30–2.
10. Mantyselka P, Kautianen H, Vanhala M. Prevalence of neck
pain in subjects with metabolic syndrome—a cross-sectional
population-based study. BMC Musculoskelet Disord 2010;11:
171, http://dx.doi.org/10.1186/1471-2474-11-171.
11. Rechardt M, Shiri R, Karppinen J, Jula A, Heliövaara M,
Viikari-Juntura E. Lifestyle and metabolic factors in relation
to shoulder pain and rotator cuff tendinitis: a population-based
study. BMC Musculoskelet Disord 2010;11:165.
12. Gaida JE, Alfredson L, Kiss ZS, Wilson AM, Alfredson H,
Cook JL. Dyslipidemia in Achilles tendinopathy is
characteristic of insulin resistance. Med Sci Sports Exerc
2009;41:1194–7.
13. Malliaras P, Cook JL, Kent PM. Anthropometric risk factors
for patellar tendon injury among volleyball players. Br J
Sports Med 2007;41:259–63.
14. Skrzynski S. DSC study of collagen in disc disease. J Biophys
2009;2009:819635, http://dx.doi.org/10.1155/2009/819635.
15. Luevano-Contreras C, Chapman-Novakofski K. Dietary
advanced glycation end products and aging. Nutrients
2010;2(12):1247–65 [2009;2009:819635].
16. Abate M, Schiavone C, Pelotti P, Salini V. Limited joint
mobility (LJM) in elderly subjects with type II diabetes
mellitus. Arch Gerontol Geriatrics 2011;53:135–40.
17. Sakellaridis N. The influence of diabetes mellitus on lumbar
intervertebral disk herniation. Surg Neurol 2006;66:152–4.
18. Shepherd PR, Kahn BB. Glucose transporters and insulin
action: implications for insulin resistance and diabetes
mellitus. New Eng J Med 1999;341(4):248–57.
19. Abdul-Ghani MA, DeFronzo RA. Pathogenesis of insulin
resistance in skeletal muscle. J Biomed Biotechnol 2010:19,
http://dx.doi.org/10.1155/2010/476279 [Article ID 476279].
20. [Internet]American Heart Association. About metabolic
syndrome. Dallas: The Association; 2014. [Available from
http://www.heart.org/HEARTORG/Conditions/More/
MetabolicSyndrome/About-Metabolic-Syndrome_UCM_
301920_Article.jsp].
21. Hotamisligil GS. Inflammation and metabolic disorders.
Nature 2006;444:860–7.
22. Glass CK, Olefsky JM. Inflammation and lipid signaling in the
etiology of insulin resistance. Cell Metab 2012;15(5):635–45.
23. Reaven GM. All obese individuals are not created equal:
insulin resistance is the major determinant of cardiovascular
disease in overweight/obese individuals. Diabetes Vasc Dis
Res 2005;2:105–12.
24. Ritov VB, Menshikova EV, He J, Ferrell RE, Goodpaster
BH, Kelley DE. Deficiency of subsarcolemmal mitochondria
in obesity and type 2 diabetes. Diabetes 2005;54:8–14.
25. Corcoran MP, Lamon-Fava S, Fielding RA. Trans fats and
insulin resistance: skeletal muscle lipid deposition and insulin
resistance: effect of dietary fatty acids and exercise. Am J Clin
Nutr 2007;85:662–77.
26. Schipper HS, Prakken B, Kalkhoven E, Boes M. Adipose
tissue-resident immune cells: key players in immunometabolism.
Trends Endocrinol Metab 2012;23:407–15.
27. Antuna-Puente B, Feve B, Fellahi S, Bastard JP. Adipokines:
the missing link between insulin resistance and obesity.
Diabetes Metab 2008;34:2–11.
28. Grimble RF. Inflammatory status and insulin resistance. Curr
Opin Clin Nutr Metab Care 2003;5:551–9.
29. Tilg H, Moschen AR. Inflammatory mechanisms in
the regulation of insulin resistance. Mol Med 2008;3–4:222–31.
30. Johnson DR, O’Conner JC, Satpathy A, Freund GG.
Cytokines in type 2 diabetes. Vitam Horm 2006;74:405–41.
31. Ridker PM, Wilson PW, Grundy SM. Should C-reactive
protein be added to the metabolic syndrome and to
assessment of global cardiovascular risk? Circulation 2004;
109:2818–25.
32. Gelaye B, Revilla L, Lopez T, et al. Association between
insulin resistance and c-reactive protein among Peruvian
adults. Diabetol Metab Syn 2010;2:30.
33. Singh VP, Bali A, Singh N, et al. Advanced glycation end
products and diabetic complications. Korean J Physiol
Pharmacol 2014;18(1):1–14.
34. Baker RG, Hayden MS. NF-kB, inflammation and metabolic
disease. Cell Metab 2011;13(1):11–22.
35. Purkayastha S, Cair D. Neuroinflammatory basis of metabolic
syndrome. Mol Metab Nov 2013;2(4):356–63.
36. Ehse JA, Boni-Schnetzler M, Faulenbach M, Donath MY.
Macrophages, cytokines and beta-cell death in type 2 diabetes.
Biochem Soc Trans 2008;36(3):340–2.
37. Boni-Schnetzler M, Ehses JA, Faulenbach M, Donath MY.
Insulitis in type 2 diabetes. Diabetes Obes Metab 2008;10
(Suppl 4):201–4.
38. Donath MY, Schumann DM, Faulenbach M, Ellingsgaard H,
Perren A, Ehses JA. Islet inflammation in type 2
diabetes: from metabolic stress to therapy. Diabetes Care
2008;31(Suppl 2):S161–4.
39. Donath MY, Boni-Schnetzler M, Ellingsgaard H, Ehses JA.
Islet inflammation impairs the pancreatic beta-cell in type 2
diabetes. Physiology 2009;24:325–31.
40. Harford KA, Reynolds CM, McGillicuddy FC, Roche HM.
Fats, inflammation and insulin resistance: insights to the role
of macrophage and T-cell accumulation in adipose tissue.
Proc Nutr Soc 2011;70:408–17.
41. Munoz A, Costa M. Nutritionally mediated oxidative stress and
inflammation. Oxid Med Cell Longev 2013;2013:610950, http://
dx.doi.org/10.1155/2013/610950.
42. Wisse BE, Schwartz MW. Does hypothalamic inflammation
cause obesity? Cell Metab 2009;10(4):241–2.
43. Purkayastha S, Cair D. Neuroinflammatory basis of metabolic
syndrome. Mol Metab Nov 2013;2(4):356–63.
44. Calegari VC, Torsoni AS, Vanzela EC, Araújo EP, Morari
J, Zoppi CC, et al. Inflammation of the hypothalamus leads
to defective pancreatic islet function. J Biol Chem 2011;
286(15):12870–80.
45. Cordain L, Eaton SB, Sebastian A, et al. Origins and evolution
of the Western diet: health implications for the 21st century.
Am J Clin Nutr 2005;81:341–54.
46. Barclay AW, Petocz P, McMillan-Price J, et al. Glycemic
index, glycemic load, and chronic disease risk—a metaanalysis
of observational studies. Am J Clin Nutr
2008;87:627–37.
47. Facchini FS, Hua N, Abbasi F, Reaven GM. Insulin resistance
as a predictor of age-related disease. J Clin Endocrinol Metab
2001;86:3574–8.
48. Lin H, Lee B, Ho Y, et al. Postprandial glucose improves the
risk prediction of cardiovascular death beyond the metabolic
syndrome in the nondiabetic population. Diabetes Care Sep
2009;32(9):1721–6.
49. O’Keefe JH, Bell DS. Postprandial hyperglycemia/
hyperlipidemia (postprandial dysmetabolism) is a cardiovascular
risk factor. Am J Cardiol 2007;100:899–904.
50. Cao H. Adipocytokines in obesity and metabolic disease.
J Endocrinol 2014;220(2):T47–59.
51. Nah SS, Choi IY, Lee CK, et al. Effects of advanced glycation
end products on the expression of COX2, PGE2 and NO in human osteoarthritic chondrocytes. Rheumatology (Oxford)
2008;47(4):425–31.
52. Abate M, Schiavone C, Pelotti P, Salini V. Limited joint
mobility (LJM) in elderly subjects with type II diabetes
mellitus. Arch Gerontol Geriatr 2011;53:135–40.
53. Robinson D, Mirovsky Y, Halperin N, Evron Z, Nevo Z.
Changes in proteoglycans of intervertebral disc in diabetic
patients: a possible cause of increased back pain. Spine
1998;23:849–56.
54. Sakellaridis N, Androulis A. Influence of diabetes mellitus on
cervical intervertebral disc herniation. Clin Neurol Neurosurg
2008;110:810–2.
55. Jhawar BS, Fuchs CS, Colditz GA, Stampfer MJ. Cardiovascular
risk factors for physician-diagnosed lumbar disc
herniation. Spine J 2006;6:684–91.
56. Lotan R, Oron A, Anekstein Y, Shalmon E, Mirovsky Y.
Lumbar stenosis and systemic diseases: is there any relevance.
J Spinal Disord Tech 2008;21:247–51.
57. Anekstein Y, Smorgick Y, Lotan R, et al. Diabetes mellitus as
a risk factor for the development of lumbar spinal stenosis. Isr
Med Assoc J 2010;12:16–20.
58. Choi KM. Sarcopenia and sarcopenic obesity. Endocrinol
Metab (Seoul) 2013;28(2):86–9.
59. D’hooge R, Cagnie B, Crombez G, et al. Increased
intramuscular fatty infiltration without differences in lumbar
muscle cross-sectional area during remission of unilateral
recurrent low back pain. Man Ther 2012 Dec;17(6):5584–8.
60. Chen YY, Pao JL, Liaw CK, et al. Image changes of paraspinal
muscles and clinical correlations in patients with unilateral
lumbar spinal stenosis. Eur Spine J 2014;23(5):999–1006.
61. Kim Y, Park H. Does regular exercise without weight loss
reduce insulin resistance in children and adolescents? In J
Endocrinol 2013:402592, http://dx.doi.org/10.1155/2013/
402592 [Epub 2013 Dec 12].
62. Strasser B, Siebert U, Schobersberger W. Resistance training
in the treatment of the metabolic syndrome: a systematic
review and meta-analysis of the effect of resistance training on
metabolic clustering in patients with abnormal glucose
metabolism. Sports Med 2010;40:397–415.
63. Sharman MJ, Volek JS. Weight loss leads to reductions in
inflammatory biomarkers after a very-low-carbohydrate diet
and a low-fat diet in overweight men. Clin Sci (Lond)
2004;13:365–9.
64. Teng KT, Chang CY, Chang LF, et al. Modulation of obesityinduced
inflammation by dietary fats: mechanisms and
clinical evidence. Nutr J 2014;13:12, http://dx.doi.org/
10.1186/1475-2891-13-12.
65. Tzotzas T, Evangelou P, Kiortsis DN. Obesity, weight loss
and conditional cardiovascular risk factors. Obes Rev 2011;12
(5):e282–9.
66. Stone N, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA
Guideline on the Treatment of Blood Cholesterol to Reduce
Atherosclerotic Cardiovascular Risk in Adults: A report of
the American College of Cardiology/American Heart
Association Task Force on practice guidelines. Circulation
2014;129(25 Suppl 2):S1–S45.
67. Pérez-Guisado J, Muñoz-Serrano A. A pilot study of the
Spanish ketogenic Mediterranean diet: an effective therapy for
the metabolic syndrome. J Med Food 2011;14(7–8):681–7.
68. Pérez-Guisado J, Muñoz-Serrano A, Alonso-Moraga A.
Spanish ketogenic Mediterranean diet: a healthy cardiovascular
diet for weight loss. Nutr J 2008;7:30, http://dx.doi.org/
10.1186/1475-2891-7-30.
69. Jonsson T, Granfeldt Y, Lindeberg S, et al. Subjective satiety
and other experiences of a Paleolithic diet compared to a
diabetes diet in patients with T2DM. Nutr J 2013;12:105,
http://dx.doi.org/10.1186/1475-2891-12-105.
70. Jonsson T, Granfeldt Y, Ahren B, et al. Beneficial effects of a
Paleolithic diet on cardiovascular risk factors in T2DM: a
randomized cross-over pilot study. Cardiovasc Diabetol
2009;8:35, http://dx.doi.org/10.1186/1475-2840-8-35.
71. Nicklas BJ, You T, Pahor M. Behavioural treatments
for chronic system inflammation: effects of dietary
weight loss and exercise training. Can Med Assoc J
2005;172(9):1199–209.
72. O’Keefe JH, Gheewala NM, O’Keefe JO. Dietary
strategies for improving post-prandial glucose, lipids, inflammation,
and cardiovascular health. J Am Coll Cardiol
2008;51:249–55.
73. O’Keefe Jr JH, Cordain L. Cardiovascular disease resulting
from a diet and lifestyle at odds with our Paleolithic genome:
how to become a 21st-century hunter–gatherer. Mayo Clin
Proc 2004;79(1):101–8.
74. Ames BN. Low micronutrient intake may accelerate the
degenerative diseases of aging through allocation of scarce
micronutrients by triage. Proc Natl Acad Sci U S A 2006;103
(47):17589–94.
75. Holick MF, Chen TC. Vitamin D deficiency: a worldwide
problem with health consequences. Am J Clin Nutr
2008;87:1080S–6S [Suppl.].
76. Toubi E, Shoenfeld Y. The role of vitamin D in regulating
immune responses. Isr Med Assoc J 2010;12(3):174–5.
77. King DE, Mainous AG, Geesey ME, Egan BM, Rehman S.
Magnesium supplement intake and C-reactive protein levels
in adults. Nutr Res 2006;26:193–6.
78. Rosanoff A, Weaver CM, Rude RK. Suboptimal magnesium
status in the United States: are the health consequences
underestimated? Nutr Rev 2012;70(3):153–64.
79. Simopoulos AP. Omega-3 fatty acids in inflammation and
autoimmune diseases. J Am Coll Nutr 2002;21(6):495–505.
80. Simopoulos AP. The importance of the omega-6/omega-3
fatty acid ratio in cardiovascular disease and other chronic
diseases. Exp Biol Med 2008;233:674–88.
81. Fung GJ, Steffen LM, Zhou X, et al. Vitamin D intake is
inversely related to risk of developing metabolic syndrome
in African American and white men and women over 20 y:
the Coronary Artery Risk Development in Young Adults
study. Am J Clin Nutr 2012;96(1):24–9 [Published online
2012 May 30].
82. Palomer X, Gonzalez-Clemente JM, Blanco-Vaca F, Mauricio
D. Role of vitamin D in the pathogenesis of type 2 diabetes
mellitus. Diabetes Obes Metab 2008;10:185–97.
83. Guadarrama-Lopez AL, Valdes-Ramos R, Martinex-Carrillo
BE. T2DM, PUFAs, and vitamin D: their relation to
inflammation. J Immunol Res 2014;2014:860703, http://dx.
doi.org/10.1155/2014/860703.
84. Cannell JJ, Hollis BW. Use of vitamin D in clinical practice.
Altern Med Rev 2008;13(1):6–20.
85. Davidson MB, Duran P, Lee ML, Friedman TC. High-dose
vitamin D supplementation in people with prediabetes and
hypovitaminosis D. Diabetes Care 2013;36(2):260–6, http://
dx.doi.org/10.2337/dc12-1204.
86. Schwalfenberg G. Vitamin D, and diabetes: improvement of
glycemic control with vitamin D3 repletion. Can Fam
Physician 2008;54:864–6.
87. Kim DJ, Xun P, Liu K, et al. Magnesium intake in relation to
systemic inflammation, insulin resistance, and the incidence
of diabetes. Diabetes Care 2010;33(12):2604–10, http://dx.
doi.org/10.2337/dc10-0994.
88. Guerrero-Romero F, Tamez-Perez HE, González-González G,
et al. Oral magnesium supplementation improves insulin
sensitivity in non-diabetic subjects with insulin resistance. A
double-blind placebo-controlled randomized trial. Diabetes
Metab 2004;30(3):253–8.
89. RodrÃguez-Morán M, Guerrero-Romero F. Oral magnesium
supplementation improves insulin sensitivity and metabolic
control in type 2 diabetic subjects: a randomized double-blind
controlled trial. Diabetes Care 2003;26(4):1147–52.
90. Song Y, He K, Levitan EB, Manson JE, Liu S. Effects of oral
magnesium supplementation on glycaemic control in type 2
diabetes: a meta-analysis of randomized double-blind controlled
trials. Diabet Med 2006;23(10):1050–6.
91. Mooren FC, Krüger K, Völker K, Golf SW,Wadepuhl M, Kraus
A. Oral magnesium supplementation reduces insulin resistance
in non-diabetic subjects—a double-blind, placebo-controlled,
randomized trial. Diabetes Obes Metab 2011;13(3):281–4.
92. Aggarwal BB. Targeting inflammation induced obesity and
metabolic diseases by curcumin and other nutraceuticals.
Annu Rev Nutr 2010;30:173–9.
93. Alappat L, Awad AB. Curcumin and obesity: evidence and
mechanisms. Nutr Rev 2010;68(12):729–38.
94. Gonzales AM, Orlando RA. Curcumin and resveratrol inhibit
nuclear factor-kappaB-mediated cytokine expression in adipocytes.
Nutr Metab 2008;5:17, http://dx.doi.org/10.1186/
1743-7075-5-17.
95. Sahebkar A. Why it is necessary to translate curcumin into
clinical practice for the prevention and treatment of metabolic
syndrome? Biofactors 2012, http://dx.doi.org/10.1002/
biof.1062 [Epub ahead of print].
96. Hsu CH, Cheng AL. Clinical studies with curcumin. Adv Exp
Med Biol 2007;595:471–80.
97. Chuengsamarn S, Rattanamongkolgul S, Luechapudiporn R,
Phisalaphong C, Jirawatnotai S. Curcumin extract for prevention
of type 2 diabetes. Diabetes Care 2012;35(11):2121–7.
98. Jurenka JS. Anti-inflammatory properties of curcumin, a
major constituent of curcuma longa: a review of preclinical
and clinical research. Altern Med Rev 2009;14(2):141–53.
99. Leach M. Gymnema sylvestre for diabetes mellitus: a systematic
review. J Altern Complement Med 2007;13(9):977–83.
100. Chattopadhyay R. A comparative evaluation of some blood
sugar lowering agents of plant origin. J Ethnopharmacol
1999;67:367–72.
101. Nahas R, Moher M. Complementary and alternative medicine
for the treatment of type 2 diabetes. Can Fam Physician
2009;55:591–6.
102. Vanadium/Vanadyl sulfate: monograph. Altern Med Rev
2009;14:17–80.
103. Boden G, Chen X, Ruiz J, et al. Effects of vanadyl sulfate
on carbohydrate and lipid metabolism in patients with noninsulin-dependent
diabetes mellitus. Metabolism 1996;45:
1130–5.
104. Jacques-Camarena O, González-Ortiz M, MartÃnez-Abundis E,
et al. Effect of vanadium on insulin sensitivity in patients with
impaired glucose tolerance. Ann Nutr Metab 2008;53:195–8.
105. Vincent JB. The biochemisty of chromium. J Nutr
2000;130:715–8.
106. Anderson RA. Chromium and insulin resistance. Nutr Res
Rev 2003;16:267–75.
107. Vincent JB. Chromium: celebrating 50 years as an essential
element? Dalton Trans 2010;39:3787–94.
108. Office of Dietary Supplements. [Internet]. Dietary supplement
fact sheet: Chromium. Washington, DC: United States
Department of Health and Human Services. http://ods.od.nih.
gov/factsheets/chromium/. Reviewed November 4, 2013.
109. Anderson RA. Chromium, glucose intolerance and diabetes.
J Am Coll Nutr 1998;17(6):548–55.
110. Cefalu WT, Rood J, Patricia Pinsonat P, et al. Characterization
of the metabolic and physiologic response to chromium
supplementation in subjects with type 2 diabetes mellitus.
Metab Clin Exp 2010;59:755–62.
111. Heimbach JT, Anderson RA. Chromium: recent studies regarding
nutritional roles and safety. Nutr Today 2005;40(4):180–95.
112. Shay KP, Moreau RF, Smith EJ, Smith AR, Hagen TM.
Alpha-lipoic acid as a dietary supplement: molecular
mechanisms and therapeutic potential. Biochim Biophys
Acta 2009;1790:1149–60.
113. Morikawa T, Yasuno R, Wada H. Do mammalian cells
synthesize lipoic acid? Identification of a mouse cDNA
encoding a lipoic acid synthase located in mitochondria.
FEBS Lett 2001;498:16–21.
114. Singh U, Jialal I. Alpha-lipoic acid supplementation and
diabetes. Nutr Rev 2008;66(11):646–57.
115. Padmalayam I, Hasham S, Saxena U, Pillarisetti S. Lipoic acid
synthase (LASY): a novel role in inflammation, mitochondrial
function, and insulin resistance. Diabetes 2009;58:600–8.
116. Capasso I, Esposito E, Maurea N, et al. Combination of
inositol and alpha lipoic acid in metabolic syndrome-affected
women: a randomized placebo-controlled trial. Trial
2013;14:273, http://dx.doi.org/10.1186/1745-6215-14-273.
117. Udupa A, Nahar P, Shah S, et al. A comparative study of
effects of omega-3 fatty acids, alpha lipoic acid and vitamin E
in T2DM. Ann Med Health Sci Res 2013;3(3):442–6.
Post Disclaimer
Professional Scope of Practice *
The information herein on "Metabolic Syndrome And Chiropractic" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card




 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.