When compared to other central nervous system (CNS) health issues, chronic neurodegenerative diseases can be far more complicated. Foremostly, because the compromised mitochondrial function has been demonstrated in many neurodegenerative diseases, the resulting problems in energy sources are not as severe as the energy collapse in ischemic stroke. Therefore, if excitotoxicity contributes to neurodegeneration, a different time of chronic excitotoxicity needs to be assumed. In the following article, we will outline what is known about the pathways that may cause excitotoxicity in neurodegenerative diseases. We will specifically discuss that in amyotrophic lateral sclerosis (ALS), Alzheimer’s disease (AD) and Huntington’s disease (HD) as fundamental examples with sufficiently validated animal models in research studies. Â
Table of Contents
Alzheimer’s Disease
Alzheimer’s disease (AD) is one of the main causes of dementia among older adults in the United States. Neuropathologically, AD is characterized as neurodegeneration with extracellular senile plaques made up of β amyloid (Aβ) and intraneuronal neurofibrillary tangles of aggregated tau, which initially appear in the hippocampus than then spread as the health issue progresses. Prominent microglial cell activation can also be associated with AD. Hereditary types of AD occur due to mutations in the Aβ precursor protein, AβPP, or in the presenilins, which are part of the multi-protein complex involved in Aβ generation. The pathophysiology of AD is complicated and a variety of pathways are included in the synaptic and the cellular degeneration in AD, such as abnormalities in signaling pathways through glycogen synthase kinase-3 beta or mitogen-activated protein kinases, cell cycle re-entry, oxidative stress, or decreased transport of trophic factors and adrenal dysregulation. However, evidence suggests that L-glutamate dysregulation plays a critical role in Alzheimer’s disease. Â
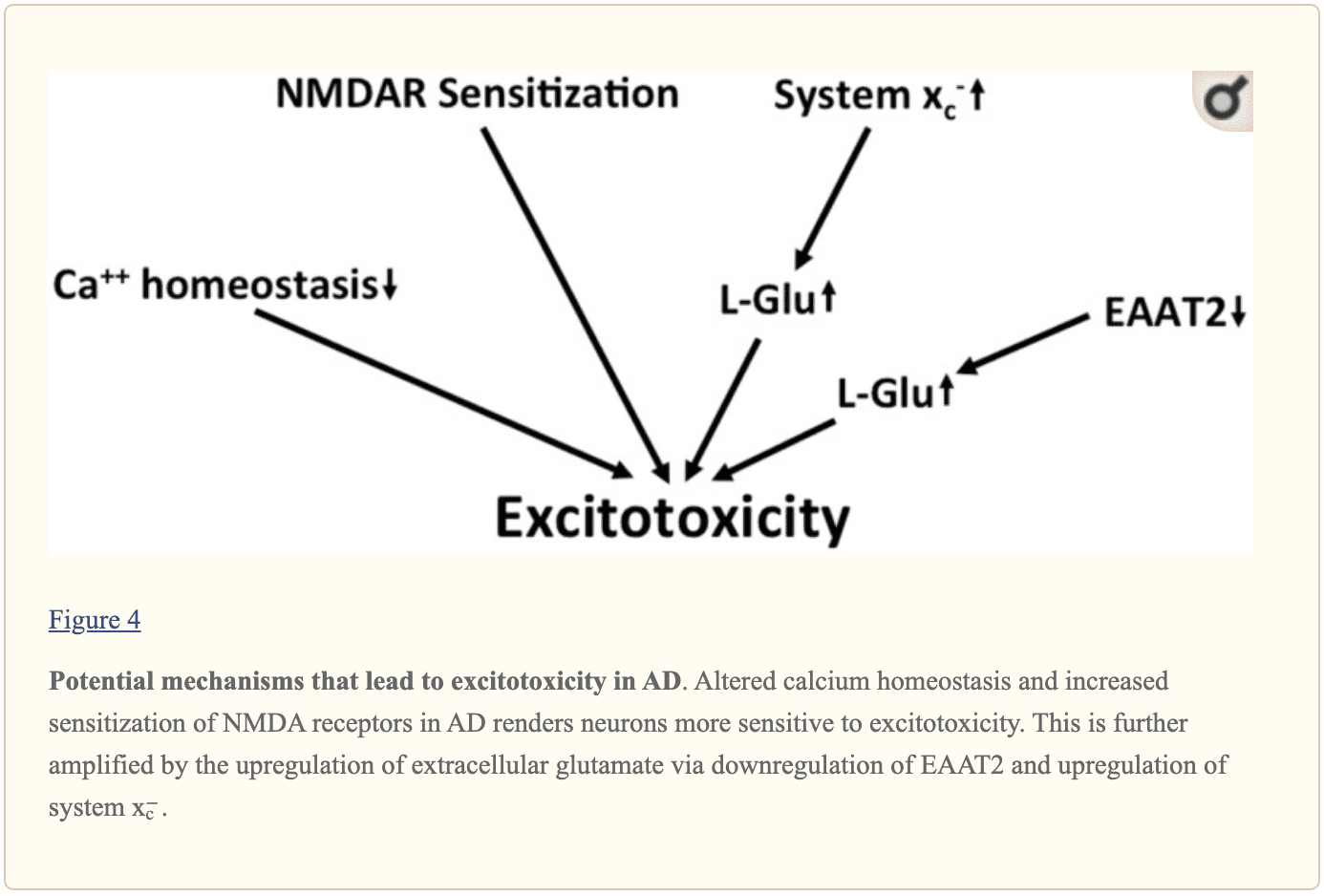
Research studies demonstrated that primary neurons from transgenic mice overexpressing mutant presenilin are far more sensitive to excitotoxic stimulation in vitro. In vitro, aggregated Aβ increases both NMDA and kainate receptor-mediated L-glutamate toxicity, perhaps by interrupting neuronal calcium homeostasis. Others have demonstrated that Aβ can increase neuronal excitability by changing the capacity of glycogen synthase kinase 3β inhibition to decrease NMDA receptor-mediated pathways. Soluble Aβ oligomers were demonstrated to cause L-glutamate release from astrocytes resulting in dendritic spine loss through over-activation of extrasynaptic NMDA receptors. Moreover, extracellular L-glutamate concentrations were demonstrated to increase in a triple transgenic mouse model of AD, in which a 3-month treatment with the NMDA receptor inhibitor ultimately affected synapse loss. However, further research studies are still required. Â
Numerous mouse research studies have demonstrated the consequences of AD-like pathology on EAAT expression and/or function. In acute hippocampal slice preparations, Aβ was shown to interrupt the clearance of synaptically released L-glutamate by diminishing membrane insertion of EAAT2, a result perhaps mediated by oxidative stress. In aged AβPP23 mice, research studies revealed the downregulation of EAAT2 expression in the frontal cortex and hippocampus, which in the frontal cortex was associated with an increase in xCT expression. These changes were associated with a strong tendency toward improved extracellular L-glutamate amounts as measured by microdialysis. In triple transgenic AD mice expressing the amyloid precursor protein mutations K670N and M671L, the presenilin 1 mutation M146V and the tau P301L mutation, a strong and age-dependent decrease of EAAT2 expression was demonstrated. Restoration of EAAT2 activity in the AD mice following treatment with all the β-lactam antibiotic Cef was associated with a decrease in cognitive impairment and reduced tau pathology. In human AD brains, decreased expression of EAAT2 protein and a decrease in EAAT action was determined. However, this outcome measure could not be replicated by other researchers. On the transcriptome level, research studies discovered exon-skipping splice variations of EAAT2 which reduce glutamate transport activity to be upregulated in human AD brains. From the CSF, several groups demonstrated an increase in glutamate concentrations in AD patients where other groups demonstrated absolutely no change or even diminished levels of L-glutamate associated with Alzheimer’s disease. Â
In vitro, Aβ causes L-glutamate discharge from primary microglia through the upregulation of program x−c. Others discovered that it also triggered L-glutamate release from astrocytes through the activation of the α7 nicotinic acetylcholine receptor. Additionally, xCT, the specific subunit of system x−c is upregulated at the region of senile plaques, possibly in microglial cells, in Thy1-APP751 mice (TgAPP) expressing human APP bearing the Swedish (S: KM595/596NL) and London (L: V6421) mutations after Aβ injection in the hippocampus. Semiquantitative immunoblot evaluations revealed an upregulation of xCT protein expression in the frontal cortex in elderly AβPP23 mice compared to wild-type controls. Â
Postmortem research studies show that KYN metabolism affects AD elevated concentrations of KYNA while also discovered in the basal ganglia of both AD sufferers. Utilizing immunohistochemistry, research studies demonstrated immunoreactivity for both IDO and QUIN upregulated in AD brains, particularly in the vicinity of plaques. Aβ causes IDO expression in human primary macrophages and microglia. Systemic inhibition of KMO ultimately increases brain KYNA levels and ameliorated the phenotype of a mouse model of AD, indicating an upregulation of KYNA may be an endogenous protective reaction, including the IDO inhibitor, coptisine, decreased microglial, astrocytic activation and cognitive impairment in AD mice. Â
Taken together, along with many other harmful changes, there is evidence for chronic excitotoxicity in AD which can be driven by numerous variables, including the central sensitization of both NMDA receptors, a decrease in L-glutamate and L-aspartate reuptake capacity and an increase in glutamate release through system x−c, as shown in Figure 4. Although the KYN pathway seems to be upregulated in AD, no specific conclusions can be drawn regarding glutamatergic neurotransmission from the upregulation of the two QUIN which was neurotoxic and neuroprotective KYNA. Â
 Â
 
In many research studies, evidence and outcome measures have demonstrated that glutamate dysregulation and excitotoxicity in many neurological diseases, including AD, HD, and ALS, ultimately lead to neurodegeneration and a variery of symptoms associated with the health issues. The purpose of the following article is to discuss and demonstrate the role that glutamate dysregulation and excitotoxicity plays on neurodegenerative diseases. The mechanisms for excitotoxicity are different for every health issue. – Dr. Alex Jimenez D.C., C.C.S.T. Insight – Dr. Alex Jimenez D.C., C.C.S.T. Insight
Metabolic Assessment Form
The following Metabolic Assessment Form can be filled out and presented to Dr. Alex Jimenez. Symptom groups listed on this form are not intended to be utilized as a diagnosis of any type of disease, condition, or any other type of health issue. Â
In the article above, we outlined what is known about the pathways which may cause excitotoxicity in neurodegenerative diseases. We also discussed that in amyotrophic lateral sclerosis (ALS), Alzheimer’s disease (AD) and Huntington’s disease (HD) as fundamental examples with sufficiently validated animal models in research studies. The scope of our information is limited to chiropractic, musculoskeletal and nervous health issues as well as functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or chronic disorders of the musculoskeletal system. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 . Â
Curated by Dr. Alex Jimenez Â
References Â
- Lewerenz, Jan, and Pamela Maher. “Chronic Glutamate Toxicity in Neurodegenerative Diseases-What Is the Evidence?†Frontiers in Neuroscience, Frontiers Media S.A., 16 Dec. 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4679930/.
Additional Topic Discussion: Chronic Pain
Sudden pain is a natural response of the nervous system which helps to demonstrate possible injury. By way of instance, pain signals travel from an injured region through the nerves and spinal cord to the brain. Pain is generally less severe as the injury heals, however, chronic pain is different than the average type of pain. With chronic pain, the human body will continue sending pain signals to the brain, regardless if the injury has healed. Chronic pain can last for several weeks to even several years. Chronic pain can tremendously affect a patient’s mobility and it can reduce flexibility, strength, and endurance.
Neural Zoomer Plus for Neurological Disease
Dr. Alex Jimenez utilizes a series of tests to help evaluate neurological diseases. The Neural ZoomerTM Plus is an array of neurological autoantibodies which offers specific antibody-to-antigen recognition. The Vibrant Neural ZoomerTM Plus is designed to assess an individual’s reactivity to 48 neurological antigens with connections to a variety of neurologically related diseases. The Vibrant Neural ZoomerTM Plus aims to reduce neurological conditions by empowering patients and physicians with a vital resource for early risk detection and an enhanced focus on personalized primary prevention. Â
Formulas for Methylation Support
XYMOGEN’s Exclusive Professional Formulas are available through select licensed health care professionals. The internet sale and discounting of XYMOGEN formulas are strictly prohibited.
Proudly, Dr. Alexander Jimenez makes XYMOGEN formulas available only to patients under our care.
Please call our office in order for us to assign a doctor consultation for immediate access.
If you are a patient of Injury Medical & Chiropractic Clinic, you may inquire about XYMOGEN by calling 915-850-0900.
For your convenience and review of the XYMOGEN products please review the following link.*XYMOGEN-Catalog-Download Â
* All of the above XYMOGEN policies remain strictly in force.
Â
Post Disclaimer
Professional Scope of Practice *
The information herein on "Functional Neurology: Chronic Excitotoxicity in Neurodegenerative Diseases Part 2" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.