Most of us will experience it at some point — but how does it influence on athletic performance? Chiropractic injury specialist, Dr. Alexander Jimenez investigates.
Research postulates that 80 percent of the populace will undergo an acute onset of back pain at least once in their lifetimes. This adds a considerable financial burden not just on the medical system (physician consultations, prescribed drugs, physiotherapy) but also the financing of the workforce in lost employee hours and loss in productivity.
The types of lower back pain that an individual may experience include (but are not limited to):
1. Lumbar spine disc herniation with/ without sciatica
2. Lumbar spine disc bulges
3. Lumbar spine disc degeneration
4. Lumbar spine disc annular tears
5. Ligament sprains
6. Muscle strains, particularly quadrutus lumborum
7. Osteoarthritis
8. Inflammatory arthritis such as rheumatoid and anklyosing spondylitis
9. Facet joint sprains
10. Bone injuries such as stress fractures, pars defects and spondylolisthesis.
The focus for this paper will be on the previous group — that the bone injuries. This may be simply postural (slow onset repetitive trauma) or related to sports; for instance, gymnastics.
The two demographic groups that tend to endure the most extension-related low back pain are:
- People who endure all day, for instance, retailers, army, security guards etc.. Prolonged position will obviously force the pelvis to start to migrate to an anterior tilt management. This may begin to place compressive pressure on the facet joints of the spinal column as they also change towards an expansion position since they accompany the pelvic tilt.
2. Extension sports such as gymnastics, tennis, swimming, diving, football codes, volleyball, basketball, track and field, cricket fast bowlers. This is more pronounced in sports that involve extension/rotation.
Table of Contents
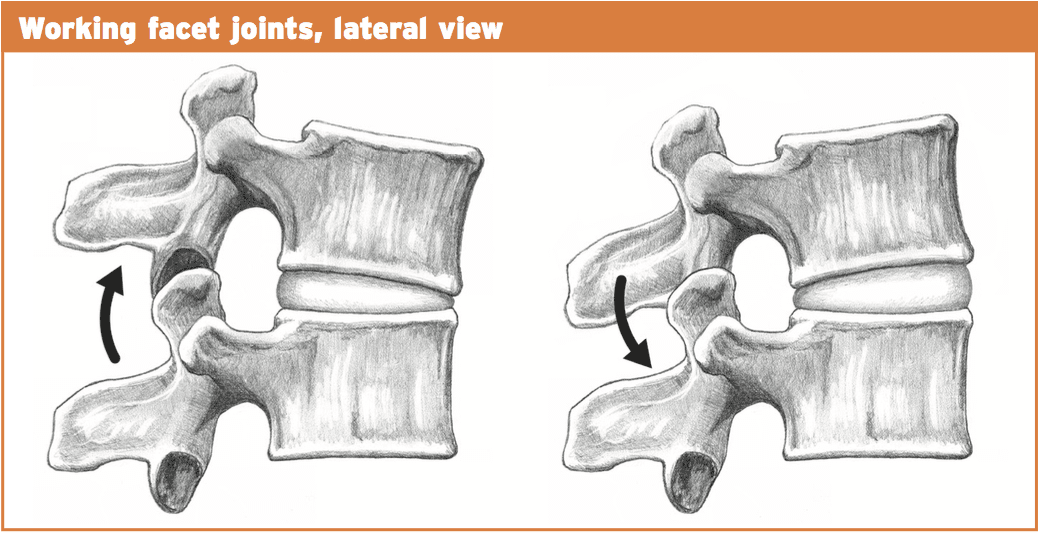
Pathomechanics
With normal extension of the lumbar spine (or backward bending), the facet joints begin to approximate each other and compress. The articular processes of this facet above will abut the articular process of the facet below. This is a normal biomechanical movement. However, if the extension ranges are excessive, the procedures will impinge quite aggressively and damage to the cartilage surfaces within the facet joint can result. Sports such as gymnastics, functioning in tennis, and handling in American Soccer may all involve uncontrolled and excessive extension.
 It would be unlikely that a bone stress response or even a stress fracture could be brought on by an isolated expansion injury. It would be more likely that a sudden forced extension injury may damage an already pre-existing bone strain reaction.
It would be unlikely that a bone stress response or even a stress fracture could be brought on by an isolated expansion injury. It would be more likely that a sudden forced extension injury may damage an already pre-existing bone strain reaction.
Similarly, if an individual stands daily and the pelvis migrates into lateral tilt, then the aspects will be placed under low load compression but for extensive intervals.
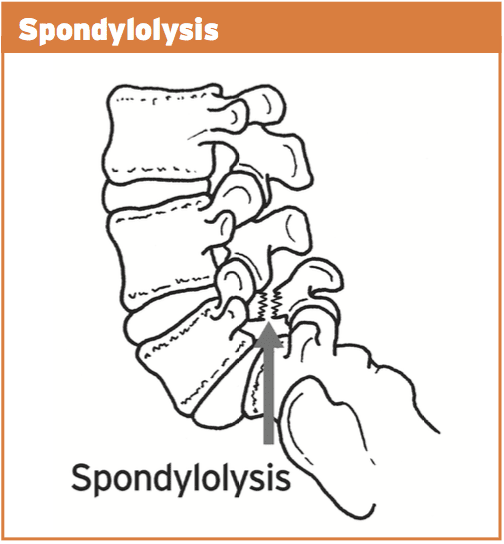
With ongoing uncontrolled loading, stress is then transferred from the facet joint to the bone below (pars interarticularis). This originally will manifest as a pressure reaction on the bone. This bone strain may advance to a stress fracture throughout the pars if uncorrected. This fracture is also referred to as a “pars flaw”, or spondylolysis.
It was initially considered that stress fractures of the pars was a congenital defect that introduced itself at the teenage years. However, it is now agreed that it is probably obtained through years of overuse into extension positions, especially in young sportspeople involved with expansion sports. What’s more, one-sided pars defects often occur more commonly in sport which also included a rotational component such as tennis serving or fast bowling in cricket.
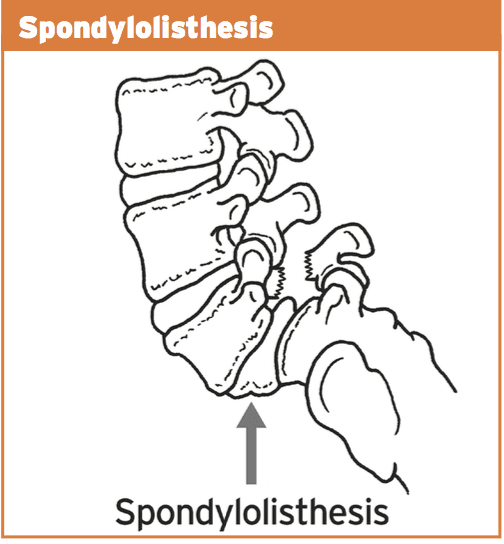
The stress fracture can then advance to impact the opposite side, causing a bilateral strain fracture, with anxiety subsequently being transferred to the disk in between both levels.
Spondylolisthesis features bilateral pars defects which could possibly be a result of repetitive stress into the bilateral pars in extension athletics, but more likely it is an independent pathology that manifests in the early growing stages (9-14) as this pathology is often viewed in this age category. If they become symptomatic in later years because of involvement in expansion sports, it is exceedingly likely that the defects were there by a young age but presented asymptomatically. As a result of rapid growth spurts in teenage years and the high-volume training experienced by teenaged athletes, it is possible that these dormant spondylolisthesis then pose as ‘acute onset’ back pain in teenage years.
In summary, the progression of this bone stress reactions tends to follow the following continuum:
1. Facet joint irritation
2. Pars interarticularis stress response
3. Stress fracture to the pars
4. Pars defect (or spondylolysis)
5. Spondylolisthesis due to activity or more likely congenital and found later in teenage years due to participation in extension sports.
The landmark publication related to spondylolysis and spondylolisthesis was presented by Wiltse et al (1976) and they classified these injuries as follows:
1. Type I: dysplastic – congenital abnormalities of L5 or the upper sacrum allow anterior displacement of L5 on the sacrum.
2. Type II: isthmic – a lesion in the pars interarticularis occurs. This is subclassified as
a. lytic, representing a fatigue fracture of the pars,
b. elongated but intact pars, and c. acute fracture.
3. Type III: degenerative – secondary to long-standing intersegmental instability with associated remodeling of the articular processes.
4. Type IV: traumatic – acute fractures in vertebral arch other than the pars.
5. Type V: pathological – due to generalized or focal bone disease affecting the vertebral arch.
The vast majority of spondylolysis and sponylolisthesis accidents are Type II — the isthmic variety.
For the purposes of this paper, we will refer to the above stages as the posterior arch bone stress injuries (PABSI).
 Epidemiology
Epidemiology
It is a lot more widespread at the L5 level (85-90 percent). It’s a high asymptomatic prevalence in the general population and is often found unintentionally on x ray imaging. Nonetheless, in athletes, particularly young athletes, it is a common reason for persistent low back pain. From the young athlete, the problem is often referred to as ‘active spondylolysis’.
Active spondylolysis is normal in virtually every gamenevertheless, sports such as gymnastics and diving and cricket pose a much greater danger due to the extension and turning character of the sport. The progression from an active spondylolysis into a non-union type spondylolisthesis has been associated with a greater prevalence of spinal disk degeneration.
Early detection through screening and imaging, therefore, will highlight those early at the bone stress phase and if caught early enough and managed, the progression to the larger and more complicated pathologies are avoided as a result of therapeutic capacity of the pars interarticularis in the early stages.
It is more common to find teens and young adults afflicted by PABSI. This will highlight the rapid growth of the spine through growth spurts that is also characterized by a delay in the motor control of the muscle system during this period. Furthermore, it’s thought that the neural arch actually gets stronger in the fourth decade hence possibly explaining the low incidence of bone stress reactions in mid ages.
The incidence of spondylolysis has been reported to be around 4-6% in the Caucasian population (Friedrikson et al 1984). The rates seem to be lower in females and also in African-American males. It has also been suggested that a link exists between pars defects and spina bifida occulta.
The incidence of spondylolysis seems to be higher in the young athletic population than in the general population. Studies in gymnasts, tennis, weightlifting, divers and wrestlers all show disproportionately high incidence of spondylolysis compared with the general population of age-matched subjects.
Tennis
The tennis serve generates excessive extension and rotation force. In addition, the forehand shot may also produce elevated levels of spinning/ extension. The more traditional forehand shot demanded a great deal of weight shift through the legs to the torso and arms. However, a more favorite forehand shot is to currently face the ball and also generate the force of this shot utilizing hip rotation and lumbar spine extension. This action does increase ball speed but also puts more extension and compressive loads on the spine potentially resulting in a greater degree of stress on the bone components.
Golf
The most likely skill component involved in golf that may cause a PABSI are the tee shot with a 1 wood when forcing for distance. The follow-through of this shot entails a significant quantity of spine rotation with maybe a level of spine expansion.
Cricket
Fast bowlers in cricket are the most susceptible to PABSI. This will occur on the opposite side to the bowling arm. As the front foot engages on plant stage, the pelvis abruptly stops moving but the spine and chest continue to proceed. With the wind-up of this bowling action (rotation), when coupled with expansion this can place large forces on the anterior arch of the thoracic. More than 50% of fast bowlers will create a pars stress fracture. Young players (up to 25) are most vulnerable. Cricket governments have implemented training and competition guidelines to avoid such injuries by restricting the number of meals in training/games.
Field Events
The more common field events to cause a PABSI would be high leap followed by javelin. Both these sports create enormous ranges of backbone extension and under significant load.
Contact Sports
Sports like NFL, rugby and AFL all require skill components that need backbone expansion under load.
Gymnastics/Dancers
It goes without saying that gymnastics and dancing involves a substantial amount of repetitive spine expansion, particularly backflips and arabesques. It has been suggested that nearly all Olympic degree gymnasts could have suffered from a pars defect. Many organizing bodies now put limits on the number of hours young gymnasts can instruct to prevent the repetitive loading on the spine.
Diving
Spine extension injuries occur mostly off the spring board and on water entrance.
Diagnosis Of PABSI In Athletes
Clinical investigation
These can pose as preventable injuries. Research shows that the incidence was emphasized from the general population that have nil indicators of back pain. But, individuals will typically complain of back ache that is deep and generally unilateral (one side). This may radiate into the buttock area. The most offending movements tend to be described as expansion moves or backward bending movements. This may be a slow progression of pain or might be initiated by one acute episode of back pain in a competitive extension motion.
On clinical examination:
1. Pain may be elicited with a one-leg extension/rotation test (standing on the leg on the affected side) – stork test.
2. Tenderness over the site of the fracture.
3. Postural faults such as excessive anterior tilt and/or pelvic asymmetry.
The one-legged hyperextension test (stork test) was suggested to be pathognomonic for busy spondylolysis. A negative evaluation was stated to effectively exclude the diagnosis of a bone stress-type injury, thus creating radiological investigations unnecessary.
But, Masci et al (2006) examined the connection between the one-legged hyperextension test and gold standard bone scintigraphy and MRI. They discovered that the one-legged hyperextension test was neither sensitive nor specific for active spondylolysis. Moreover, its negative predictive value was so poor. Thus, a negative test can’t exclude energetic spondylolysis as a possible cause.
Masci et al (2006) go on to indicate that the bad relationship between imaging and the one-legged test may be because of a number of factors. The extension test would be expected to move a significant extension force on to the lower back spine. In addition to putting substantial strain on the pars interarticularis, it might also stress different regions of the spinal column like facet joints as well as posterior lumbar disks, and this may subsequently induce pain in the existence of other pathology such as facet joint arthropathy and spinal disc disease. This will explain the poor specificity of the test. Conversely, the inadequate sensitivity of the test may be related to the subjective reporting of pain by issues performing the maneuvre, which may vary based on individual pain tolerance. Additionally, this evaluation can preferentially load the fifth cervical vertebra, and so bone stress located in the upper lumbar spine may not test positive.
Grade 1 spondylolisthesis are normally asymptomatic; nonetheless, grade 2+ lesions often present with leg pain, either with or without leg pain. On examination, a palpable slip could be evident.
Imaging
Clinical assessment of active spondylolysis and the more severe pars defects and spondylolisthesis can be notoriously non-specific; this is, not all patients suffering PABSI will present with favorable abstract features or positive signs on analyzing. Thus, radiological visualization is important for diagnosis. The imaging methods available in the diagnosis of bone stress injury are:
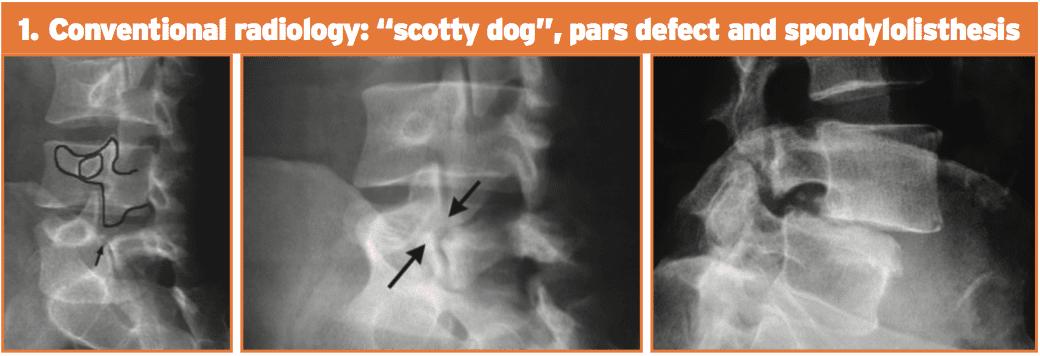
1. Conventional radiology. This test is not very sensitive but is highly unique. Its limits are partially because of the cognitive orientation of the pars defect. The oblique 45-degree films may show the timeless ‘Scotty Dog’ appearance. Spondylolisthesis can be looked at simply on a lateral movie x-ray.
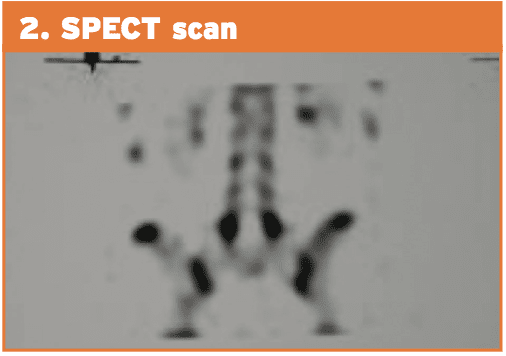
 2. Planar bone scintigraphy (PBS) and single photon emission computed tomography (SPECT). SPECT enhances sensitivity in addition to specificity of PBS than straightforward radiographic study. Comparative research between PBS and conventional radiology have shown that scintigraphy is more sensitive. Patients with positive SPECT scan must then undergo a reverse gantry CT scan to assess whether the lesion is active or old.
2. Planar bone scintigraphy (PBS) and single photon emission computed tomography (SPECT). SPECT enhances sensitivity in addition to specificity of PBS than straightforward radiographic study. Comparative research between PBS and conventional radiology have shown that scintigraphy is more sensitive. Patients with positive SPECT scan must then undergo a reverse gantry CT scan to assess whether the lesion is active or old.
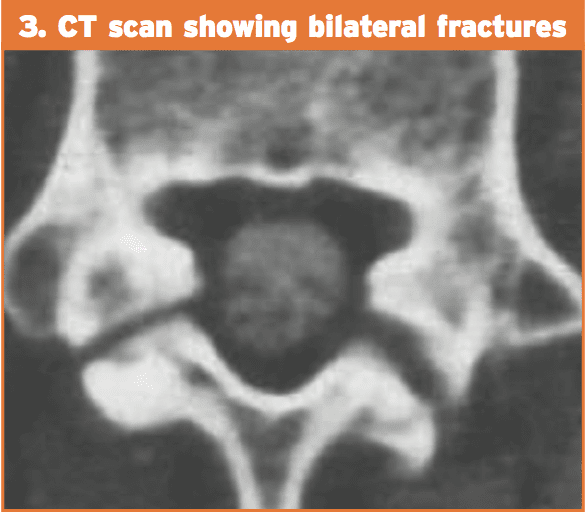
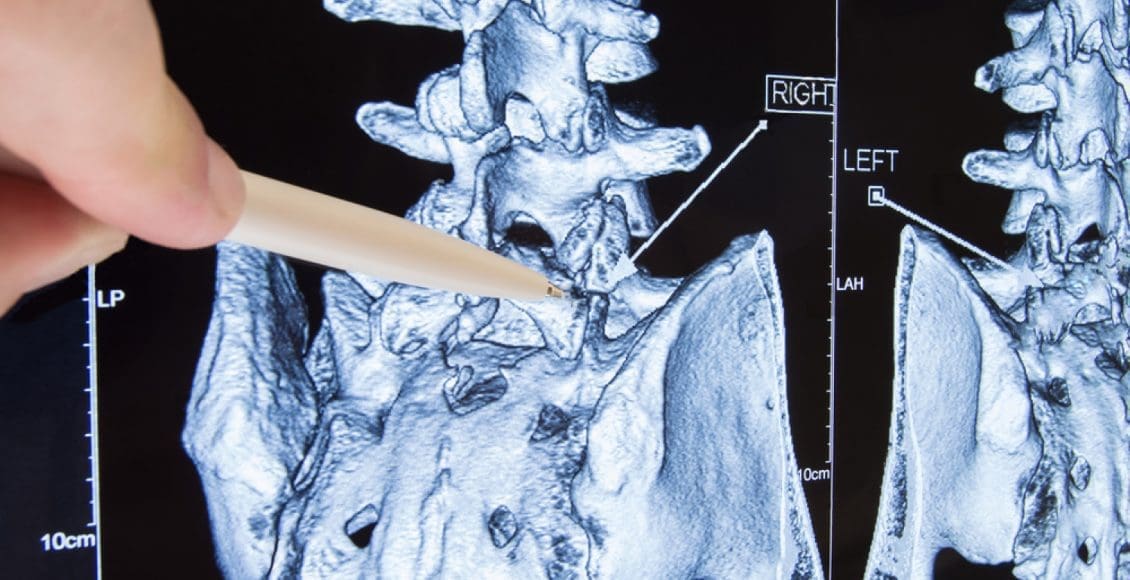
 3. Computed tomography (CT). The CT scan is considered to be more sensitive than conventional radiology and with higher specificity than SPECT. Regardless of the type of cross-sectional image utilized, the CT scan provides information on the state of the flaw (intense fracture, unconsolidated flaw with geodes and sclerosis, pars in procedure for consolidation or repair). The “inverse gantry” perspective can evaluate this condition better. Repeat CT scan can be used to track progress and recovery of the pars defect.
3. Computed tomography (CT). The CT scan is considered to be more sensitive than conventional radiology and with higher specificity than SPECT. Regardless of the type of cross-sectional image utilized, the CT scan provides information on the state of the flaw (intense fracture, unconsolidated flaw with geodes and sclerosis, pars in procedure for consolidation or repair). The “inverse gantry” perspective can evaluate this condition better. Repeat CT scan can be used to track progress and recovery of the pars defect.
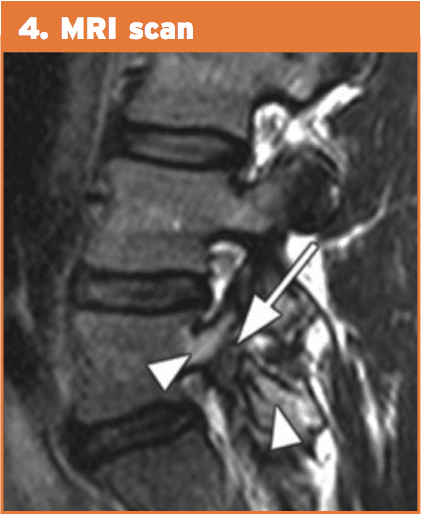
 4. Magnetic resonance imaging (MRI). This technique shows pronounced changes in the signal in the amount of the pars. This is recognized as “stress response” and can be classified into five different degrees of action. MRI can be helpful for evaluating elements that stabilize isthmic lesions, for example intervertebral disc, common anterior ligament, and related lesions. The MRI isn’t as specific or sensitive as SPECT and CT combination.
4. Magnetic resonance imaging (MRI). This technique shows pronounced changes in the signal in the amount of the pars. This is recognized as “stress response” and can be classified into five different degrees of action. MRI can be helpful for evaluating elements that stabilize isthmic lesions, for example intervertebral disc, common anterior ligament, and related lesions. The MRI isn’t as specific or sensitive as SPECT and CT combination.
 Therefore, the current gold standards of investigation for athletes with low back pain are:
Therefore, the current gold standards of investigation for athletes with low back pain are:
1. bone scintigraphy with single photon emission computed tomography (SPECT); if positive then
2. limited reverse-gantry axial computed tomography .
MRI has many advantages over bone scintigraphy, for instance, noninvasive nature of the imaging along with the absence of ionizing radiation. MRI changes in active spondylolysis include bone marrow edema, visualized as increased signal in the pars interarticularis on edema-sensitive sequences, and fracture, visualized as reduced signal in the pars interarticularis on T1 and T2 weighted sequences.
However, there is greater difficulty in detecting the changes of busy spondylolysis from MRI. Detecting pathology from MRI relies on the interpretation of distinct contrasts of signals compared with normal tissue. Unlike stress fractures in different parts of the body, the little region of the pars interarticularis may make detection of those changes harder.
However, unlike MRI, computed tomography has the capability to differentiate between acute and chronic fractures, and this differentiation might be an important determinant of fracture healing. Accordingly, in areas using pars interarticularis fractures discovered by MRI, it might nonetheless be necessary to execute thin computed tomography slices to determine whether or not a fracture is severe or chronic — an important factor in fracture resolution.
Post Disclaimer
Professional Scope of Practice *
The information herein on "Extension-Related Low Back Pain: Sports & Science" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


 Epidemiology
Epidemiology

 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.