Cauda equina syndrome/CES is a rare condition in which the nerves in the lower back are compressed. It can include sciatica as one of its symptoms. Individuals presenting with symptoms that could be CES are advised to see a healthcare provider as soon as possible, as delaying treatment can lead to permanent damage.
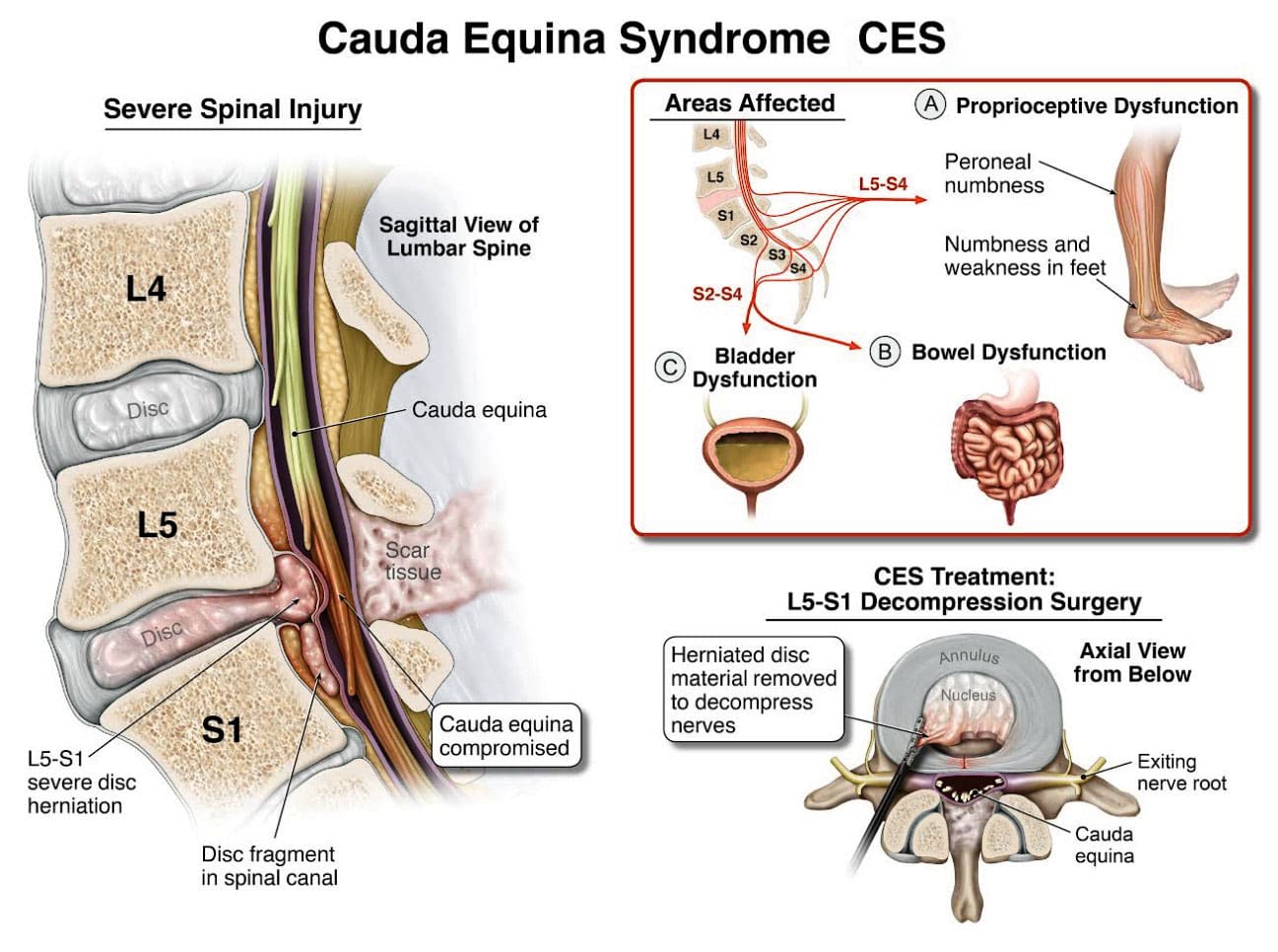
Table of Contents
Cauda Equina Syndrome
A cluster of nerve roots called the cauda equina, Latin for horse’s tail, sends and receives messages to the legs, bladder, and other body parts. Cauda equina syndrome is a rare condition in which nerve roots in the lower spinal cord are compressed. This compresses the nerves and disrupts motor and sensory function in the bladder and lower extremities. The most common cause is a ruptured or herniated disc in the lumbar area. This usually occurs when a severe disc herniation compresses the nerve bundle at the base of the spinal cord, causing significant neurological dysfunction like bladder/bowel issues and numbness in the saddle area. If found early, it is treated with surgery within 24 to 48 hours of symptom onset.
Initial Signs
Symptoms can occur acutely, in hours, or gradually over weeks or months. One of the first signs and most common symptoms is urinary retention, where the bladder fills, but there is no normal sensation or urge to urinate. (American Association of Neurological Surgeons, 2024) Other symptoms include: (Gardner A., Gardner E., & Morley T. 2011)
- Severe low back pain
- Sciatica
- Pain, numbness, or weakness in one or both legs
- Saddle anesthesia, which is numbness or other nerve sensations around the anus and the area that sits.
- A loss of reflexes in the extremities
- Sexual dysfunction that comes suddenly
- Loss of bowel control
- Overflow urination
There are two stages based on urinary symptoms (Fairbank J., & Mallen C. 2014)
CES-Incomplete CES-I
- This is characterized by symptoms that include unusual urinary sensation, loss of desire to urinate, poor urinary stream, and having to strain to urinate. (Gardner A., Gardner E., & Morley T. 2011)
CES-Retention CES-R
- Bladder control is completely lost.
Causes
The most common cause is a ruptured or herniated disc in the lumbar area. Other possible causes may include: (American Association of Neurological Surgeons, 2024)
Trauma or injury to the spine
- that leads to fractures or dislocations (gunshots, falls, auto accidents)
Tumors or Infections
- It can compress the cauda equina nerve bundle.
Spinal Stenosis
- Narrowing of the spinal column can be either congenital or acquired.
Bone Spurs
- Spurs in the spinal canal can compress the nerves. (American Association of Neurological Surgeons, 2024)
Tuberculosis or Pott’s Paralysis
- Pott’s paralysis is a neurological complication of tuberculosis (TB) of the spine.
- TB is a bacterial infection that usually affects the lungs but can spread to the spine.
Iatrogenic Side Effects
- Injuries or illnesses that result from medical or surgical treatment
Spinal Lesions or Malignant Tumors
- A spinal lesion refers to any abnormal growth or damage within the spine.
- It can include benign (noncancerous) and malignant (cancerous) tumors.
- A malignant tumor is a cancerous growth within the spine; essentially, a malignant tumor is a type of spinal lesion with the potential to spread to other parts of the body.
Spinal Infection, Inflammation, Hemorrhage, or Fracture
- A spinal infection refers to a bacterial, fungal, or viral infection that occurs within the bones of the spine (vertebrae) or the surrounding tissues, potentially causing pain, inflammation, and, in severe cases, neurological complications like weakness or paralysis;
- Spinal inflammation is a general term for swelling or irritation within the spinal column.
- Spinal hemorrhage” indicates bleeding within the spinal canal.
- A spinal fracture refers to a break in one or more of the vertebrae in the spine.
Spinal Arteriovenous Malformations (AVMs)
- A spinal arteriovenous malformation (AVM) is a rare condition in which the arteries and veins in the spinal cord tangle abnormally.
- This can damage the spinal cord over time.
Complications from Lumbar Surgery
- Lumbar surgery can have several complications, including infections, blood clots, nerve damage, and spinal fluid leaks.
Spinal Anesthesia
- Spinal anesthesia is a regional anesthesia that blocks pain and sensation in the lower body.
- It involves injecting a local anesthetic medication into the subarachnoid space surrounding the spinal cord.
- The exact cause is not fully understood, but it can involve direct nerve root injury from the needle, inflammation caused by the anesthetic, or a spinal hematoma compressing the nerve roots.
Spinal Birth Defects
- Birth defects of the spinal cord, such as spina bifida. (American Association of Neurological Surgeons, 2024)
- Infection of the tissues (meninges) that cover the cauda equina and spinal cord.
- An abscess pressing on the cauda equina.
Diagnosis
Diagnosis requires a medical history of symptoms, general health, activity level, and a physical exam to assess strength, reflexes, sensation, stability, alignment, and motion. (?American Association of Neurological Surgeons, 2024) Testing includes:
Blood Tests
- These test for infections.
MRI
- These yield three-dimensional images of the spinal cord, nerve roots, and surrounding areas.
Myelography
- X-ray or computerized tomography (CT) imaging is enhanced by the injection of contrast material into the cerebrospinal fluid spaces, which can show displacement of the spinal cord or spinal nerves.
Specialized Nerve Testing
- This could be nerve conduction velocity tests and testing electrical activity in muscles or electromyography.
Treatment
The extent of urinary problems can determine treatment protocols. A CES diagnosis is usually followed by emergency surgery within 24 to 48 hours to relieve compression of the nerves. Moving quickly is essential to prevent permanent complications such as nerve damage, incontinence, or leg paralysis. (American Association of Neurological Surgeons, 2024)
- Depending on the cause, corticosteroids also may be prescribed to reduce swelling.
- Antibiotics may be needed if an infection is responsible for CES.
- For situations in which a tumor is the cause, surgery to remove it may be necessary, followed by chemotherapy and/or radiation.
- The outcome with CES-I during surgery is generally favorable.
- Those whose CES has deteriorated to CES-R tend to have a less favorable prognosis.
Post Surgery Therapy
After surgery, CES can be challenging to deal with. If bladder function has been impaired, recovery of control can take time.
- It may be necessary to use a catheter or to wear disposable underwear. (American Association of Neurological Surgeons, 2024)
- Frequent urinary infections are also a potential complication.
- Loss of bladder or bowel control can be psychologically distressing, impacting social life, work, and relationships.
- Sexual dysfunction can also occur, contributing to relationship difficulties or depression.
Therapy with a mental health professional may be recommended. When damage is permanent, it will be important to include family and friends in the adjustment to living with a chronic condition. Psychological counseling and/or a support group can be helpful. Other specialists who can help include: (American Academy of Orthopaedic Surgeons, 2024)
- Occupational therapist
- Physical therapist
- Physiotherapist
- Sex therapist
- Social worker
Injury Medical Chiropractic and Functional Medicine Clinic
Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to build optimal health and wellness solutions. We focus on what works for you to relieve pain, restore function, prevent injury, and mitigate issues through adjustments that help the body realign itself. The clinic can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal problems.
Disc Herniation
References
American Association of Neurological Surgeons. (2024). Cauda Equina Syndrome. https://www.aans.org/patients/conditions-treatments/cauda-equina-syndrome/
Gardner, A., Gardner, E., & Morley, T. (2011). Cauda equina syndrome: a review of the current clinical and medico-legal position. European Spine Journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society, 20(5), 690–697. https://doi.org/10.1007/s00586-010-1668-3
Fairbank, J., & Mallen, C. (2014). Cauda equina syndrome: implications for primary care. The British journal of general practice: the journal of the Royal College of General Practitioners, 64(619), 67–68. https://doi.org/10.3399/bjgp14X676988
American Academy of Orthopaedic Surgeons. (2024). Cauda equina syndrome. https://orthoinfo.aaos.org/en/diseases–conditions/cauda-equina-syndrome
Post Disclaimer
Professional Scope of Practice *
The information herein on "Cauda Equina Syndrome: Early Diagnosis Benefits" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.