Acetabular labral tears of the hip are just one of the more challenging accidents for clinicians to diagnose and manage. Chiropractor, Dr. Alexander Jimenez looks at what the recent signs indicate…
Physical disturbance of the hip joint is often related to a acetabular labral tear (ALT) and may be associated with intra- articular snapping hip syndrome around 80% of instances(1). Labral tears affecting the hip joint are prevalent in 22-55% of patients having hip or groin pain(two) and evidence indicates that an untreated ALT may predispose an individual to premature degenerative arthritis(3), which has created a widespread interest within clinical practice and the literature.)
The examination and imaging techniques with guessed ALT’s have improved greatly in the last decade, but an appraisal of a labral tear still remains complex. The purpose of this article therefore is to review the anatomy and biomechanics of the acetabular labrum, the evaluation techniques and the treatment and treatment options available.
Table of Contents
Anatomy & Biomechanics
The labrum increases the surface area of this acetabulum by 22\% and the volume by 33\% and it works by forming a seal for the mind of femur to rotate (see Figure 1). From a cross-sectional view, the labrum is triangular in its appearance with the extra articular zone being dense connective tissue which has a rich blood supply and the intra thoracic zone chiefly having no blood source (3).
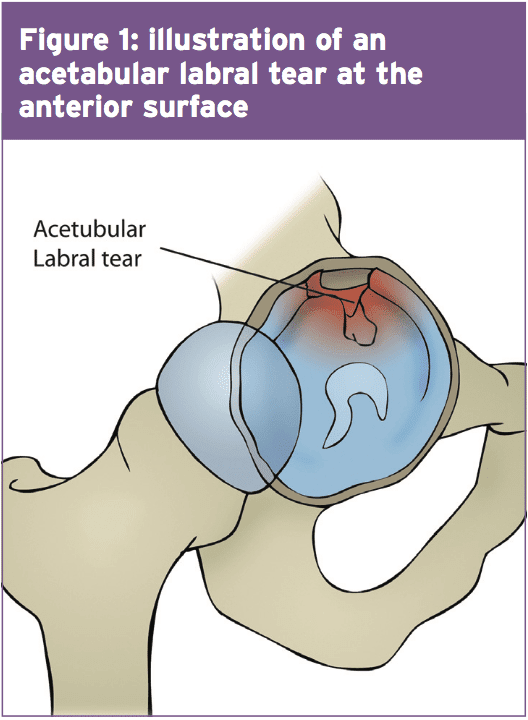 At the extreme end ranges of hip motion, The labrum is worried by compressive forces -a rip at this point can affect joint stability and load distribution(2). What’s more, pain receptors have been located in the superior and anterior areas, and the labrum is therefore regarded as a pain generating structure(4). It is in the anterior surface (Figure 1) where an ALT is most at risk due to the compressive forces at the end stage of hip flexion (5). Also of note is that structural abnormalities like retroverted acetabulum and coxa valga happen to be observed concurrently in patients (87 percent) with labral tears (6).
At the extreme end ranges of hip motion, The labrum is worried by compressive forces -a rip at this point can affect joint stability and load distribution(2). What’s more, pain receptors have been located in the superior and anterior areas, and the labrum is therefore regarded as a pain generating structure(4). It is in the anterior surface (Figure 1) where an ALT is most at risk due to the compressive forces at the end stage of hip flexion (5). Also of note is that structural abnormalities like retroverted acetabulum and coxa valga happen to be observed concurrently in patients (87 percent) with labral tears (6).
Examination & Assessment
An ALT is complicated to diagnose and even though recent improvements in medical imaging and evaluation methods, one report identified that generally, patients seen three healthcare providers and also waited for 21 months before an ALT was correctly diagnosed(3). When examining a patient with a suspected ALT, clinicians should also consider femoro-acetabular impingement (FAI) and acetabular cartilage damage, and MRI imaging ought to be used to encourage the clinical findings(3).
Acetabular labral tears are often the consequence of cutting, pivoting, twisting as well as repetitive movements into end range hip flexion usually found in tennis players, footballers and runners. This might help explain why researchers in the New England Baptist hospital in Boston, USA found that from 436 arthroscopies of labral tears in athletes, 273 (62 percent) also had articular cartilage damage(6). However the specific mechanism of an ALT injury may not always be apparent to the individual, as it may be degenerative, congenital or traumatic in its incidence(two).
During a physical assessment of a hip related injury it is essential to be vigilant for a non-musculoskeletal associated pathology. Hip associated pain may be associated to an ALT but might also be the result of spinal spine or pelvic girdle dysfunction, abdominal viscera and the peripheral nervous system(two). Pain at rest, night pain, fever, night sweats, and generally feeling unwell and unexplained weight loss are indicators of a non musculoskeletal pathology and require referral for further evaluation by a healthcare provider(2). Reiman and colleagues also indicated that hip pain may be associated with the abdominal and pelvic organs and a musculoskeletal injury must not be assumed(two).
A patient with an undiagnosed ALT may also pose with synovitis and joint inflammation and might adopt places of hip flexion, external rotation and minor abduction, which place the capsule at its largest potential volume to reduce the strain on the labrum. Positions including flexion and adduction are found to raise the total load on the labrum and this are purposely avoided.
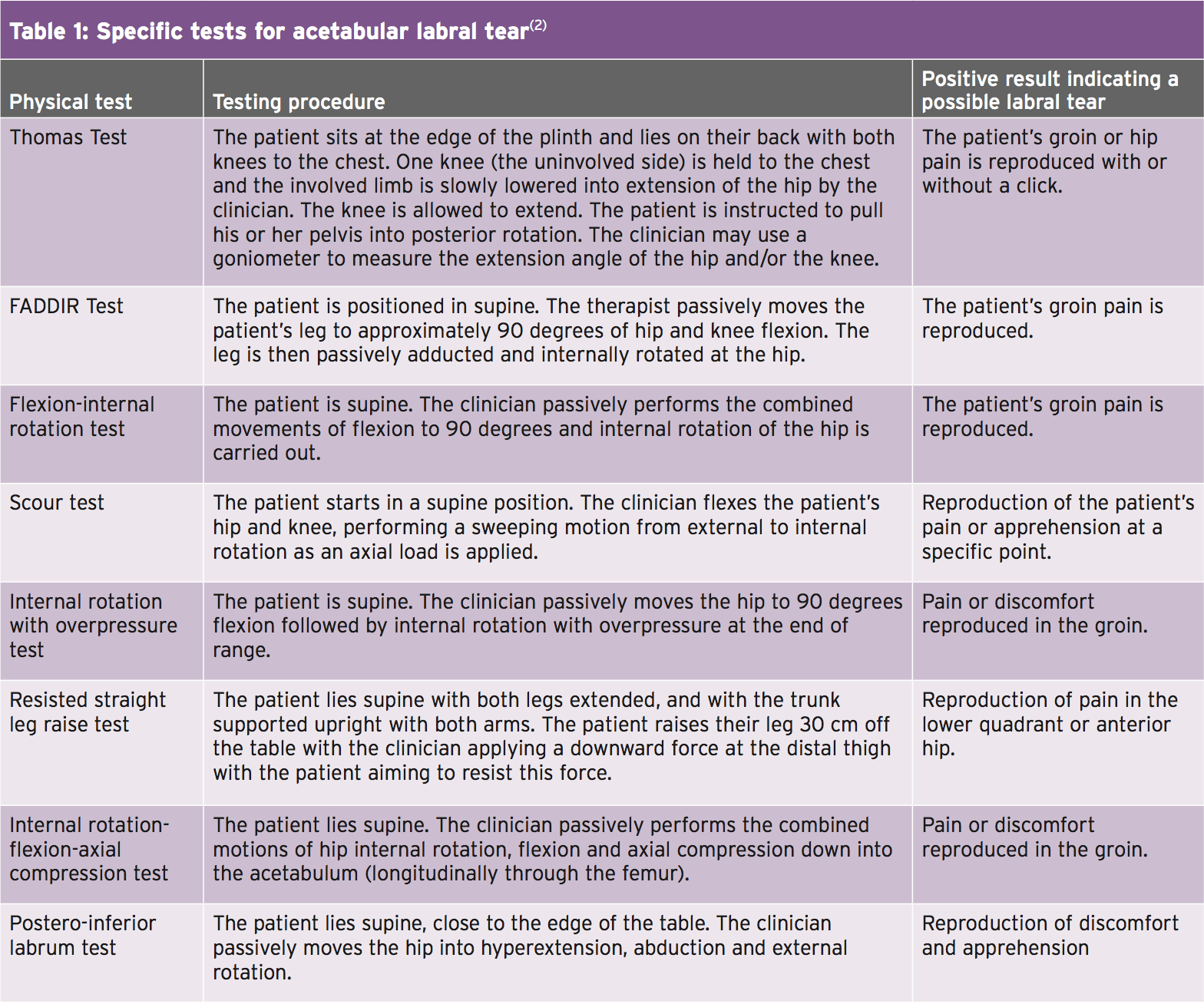
The combined impingement position of flexion, adduction and internal rotation, known as ‘FADDIRs test’ increases stress into the labrum, but can also be a contributor to intra-articular hip pathology(7). Patients using an ALT may also complain of pain on squatting, stepping up together with the joints that are involved, or sitting in a seat with the buttocks positioned lower than the knees. In addition a patient with an ALT is not likely to extend fully in the hip during gait because this places the greatest load to the anterior joint capsule and consequently stress to the anterior labrum. Table 1 outlines the many positions and specific tests for determining an ALT.
 Surgical Vs Non-Surgical Treatment
Surgical Vs Non-Surgical Treatment
Hip arthroscopy is a widely used treatment adjunct in patients presenting with an ALT symptomatic of more than four months and confirmed by MRI (magnetic resonance imaging) or MRA (magnetic resonance arthrogram)(4). Hip athroscopy for an ALT may comprise either labral debridement or labral repair. In contrast to surgical repair there’s limited support for conservative treatments for an ALT. Nevertheless researchers from Sao Paulo, Brazil have provided a case number of four patients that underwent a rehabilitation program for an ALT without operation(8). The four patients have been diagnosed with an MRI scan and failed a 3-phase program together with the first being pain management, hip and trunk stabilization, re-education and correction of abnormal joint movement. Phase two focused on restoring normal range of motion, muscular strength and beginning sensory motor training. The last phase of the rehabilitation program focused on preparing the athlete for a return to sport.
The four patients involved in the case series were in their mid twenties and were from both sedentary and athletic wallpapers(8). The outcomes of the conservative rehabilitation program yielded a decrease in pain levels, functional improvement and correction of muscle imbalances. Increased muscle strength was noted using the hip flexors increasing from 1% to 39 percent, hip abductors increasing from 18 percent to 56% and the hip extensors rising from 68% to 139%. The potency of the research is limited, with the case series being just four sufferers but nevertheless could offer an excellent proactive strategy whilst a patient is anticipating an arthroscopy.
Rehabilitation
Rehabilitation following surgical repair of an ALT is limited regarding its signs, both inside the surgeons own rehab protocol and the therapist’s experience(4). Researchers from Tampa, USA, devised a rehab protocol for the patients to follow the following protocol is mostly predicated upon(4):
Stage 1 (weeks 1–4)
- After labral debridement, weight bearing ought to be limited to 50% partial weight bearing for 7-10 days, using flexion restricted to 90° for 14 days. A labral debridement also has no limits post- operatively to abduction, external or internal rotation or extension. In contrast a labral repair should keep non-weight posture or toe-touch weight bearing for three to six weeks post operatively.
- The ranges of motion should be much more conservative in labral repair, while external and internal rotation must be invisibly transferred into for 3 weeks. Do note that if other procedures are carried out such as microfracture fix afterward the post-op protocol might well differ.
- Throughout the immediate post-operative period, it is crucial to handle pain, decrease swelling and initiate premature motion in the affected limb, however it’s also vital to concentrate on additional factors such as core activation and abductor control (see Table 2). A strong association exists between decreased action of the hip abductor muscles and lower kinetic chain injuries, including anterior knee pain(9). As a result, once the fashionable ranges are available, it is essential to encourage a patient to trigger the profound hip and backward stability muscles to prevent secondary injuries from happening.
 Stage 2 (weeks 5–7)
Stage 2 (weeks 5–7)
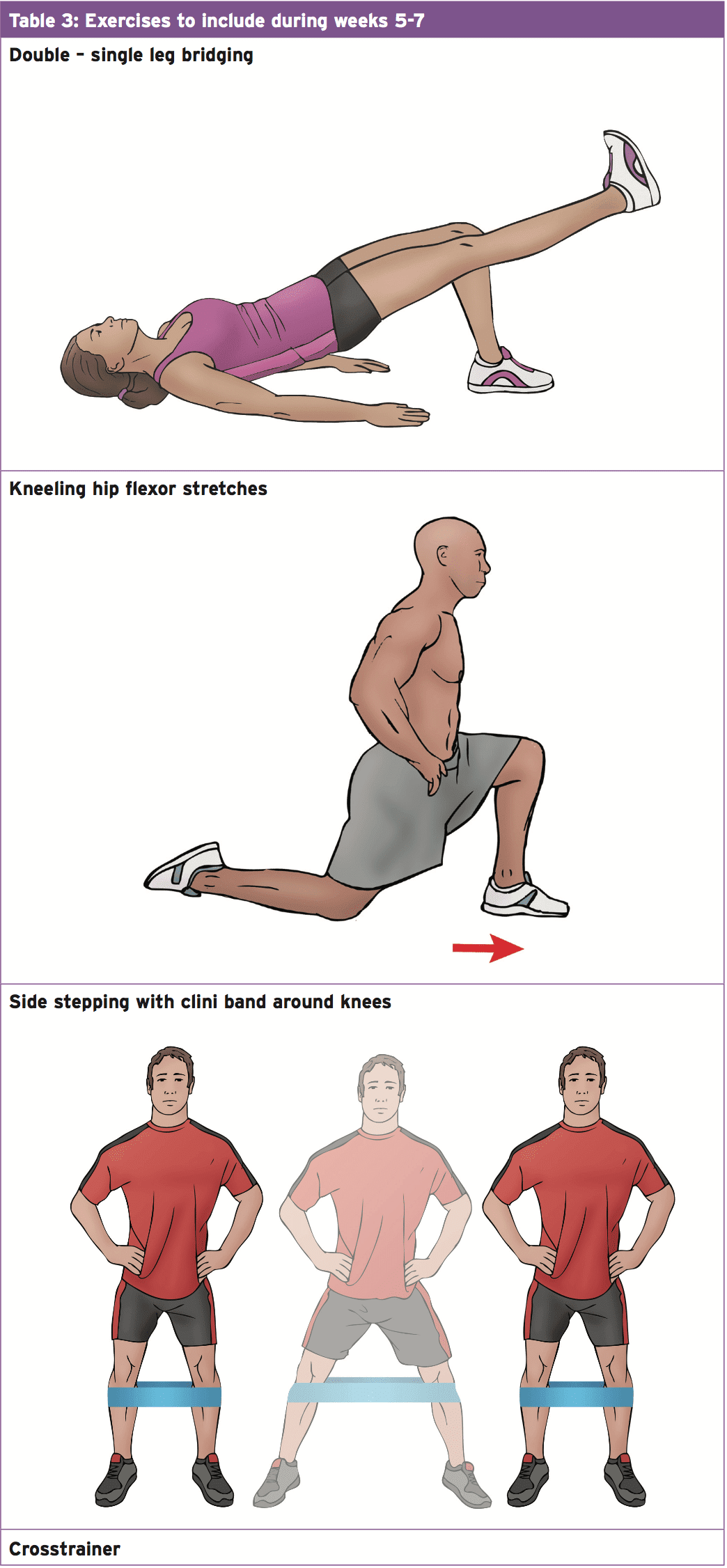
- Throughout this stage of rehabilitation it is essential to restore normal range of movement with a focus on increasing strength and growing flexibility of the muscles crossing the fashionable join (see Table 3).
 Stage 3 (weeks 8-12)
Stage 3 (weeks 8-12)
- This stage is a great opportunity to develop cardiovascular fitness and operational control of the hip. Functional stability exercises should be carried out at a standing position with an emphasis on maintaining and enhancing equilibrium ready for athletic participation. Exercises to include within this phase are walking lunges, lunges with back rotation on the front leg and a Swiss ball system suitable for challenging the core muscles. Garrison and colleagues(4)) have provided criteria (Table 4) to follow ready for development to stage four which is planning for return to sport.
 Stage 4 (months 12+)
Stage 4 (months 12+)
- This phase of the rehabilitation program is the opportunity to be preparing the athlete for their return to sport, and especially their position it’s particular tasks. If the athlete is a defender in football, they ought to be replicating tasks unique to their own position. Before the individual resuming full instruction, they have to have the ability to demonstrate the same neuromuscular controller as the uninvolved side.
Summary
A guessed ALT with the background and clinical texts should be verified using an MRI or MRA to affirm the presence Of a ALT but also to exclude any referred Pain masquerading as a Psychological injury. An appropriate rehabilitation Program ought to be started Immediately to improve hip and back control and to handle pain. This will enable the individual to proceed through the Surgery with increased simplicity having already Commenced a rehabilitation program.
References
1. Arthroscopy. 2005, 21:1120-1125
2. Br J Sports Med, 2014: 46 (4), 311-319
3. J Bone & Joint Surg Am, 2009, 91, 701–710
4. J Arthroplasty, 2001 Dec; 16 (1), 81-7
5. North American J of Sports Phys Thera Nov 2007, 2, 4, 241-250
6. Arch Orthop Trauma Surg. July 2003,123 (6), 283-8
7. Am J Sports Med 2011; 39
8. J or Ortho and Sports Phys Thera, May 2011, 41, 5, 346 – 353
9. J Athl Train. 2011 Mar-Apr; 46(2): 142–149
Post Disclaimer
Professional Scope of Practice *
The information herein on "Assessing & Managing Acetabular Labral Tears" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card



 Surgical Vs Non-Surgical Treatment
Surgical Vs Non-Surgical Treatment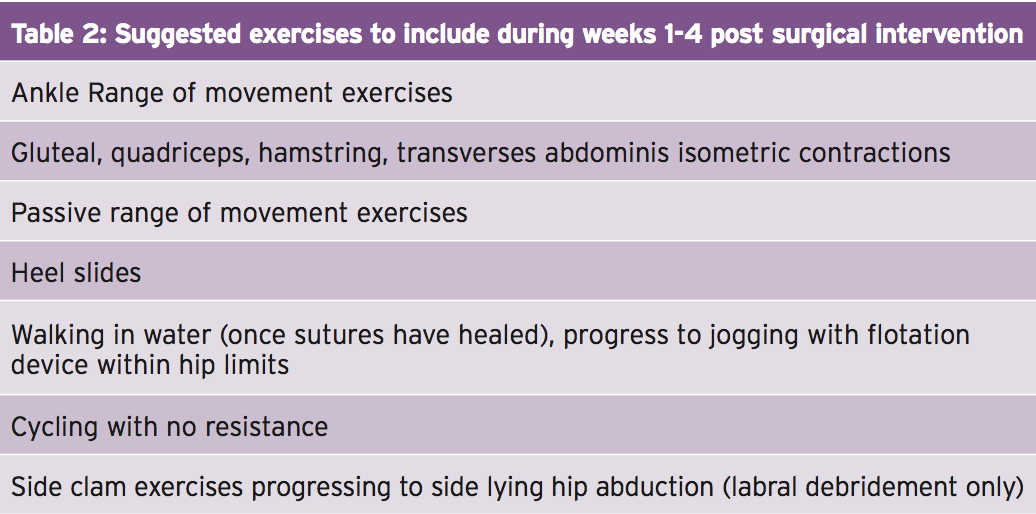 Stage 2 (weeks 5–7)
Stage 2 (weeks 5–7)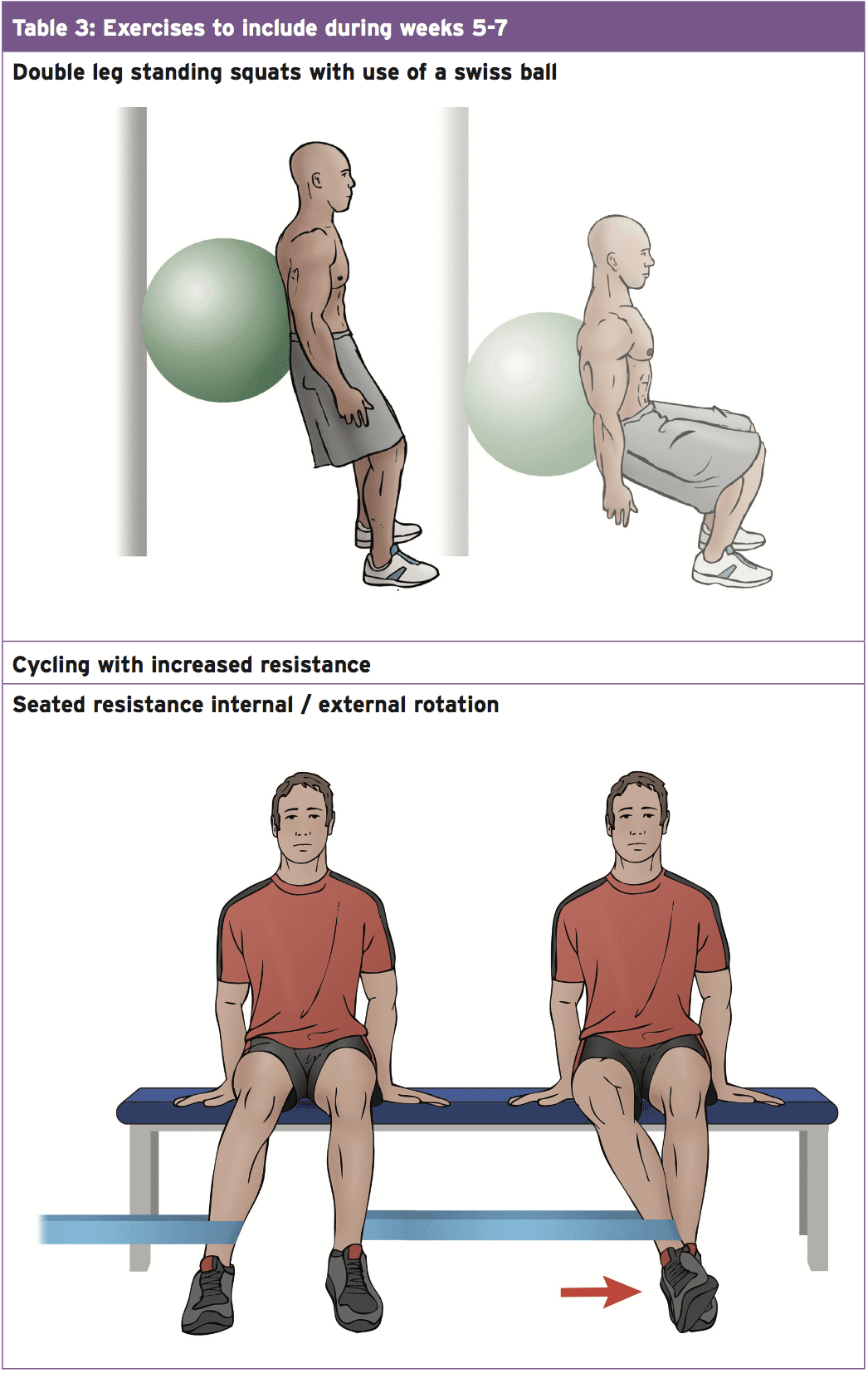
 Stage 3 (weeks 8-12)
Stage 3 (weeks 8-12)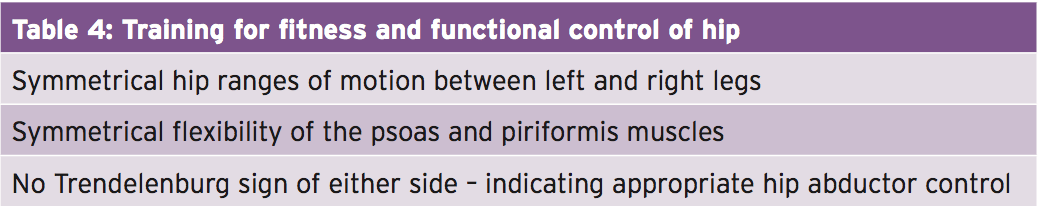 Stage 4 (months 12+)
Stage 4 (months 12+)

 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.