Individuals feeling tingling or pins and needles sensations that overtake the arms or legs could be experiencing paresthesia, which occurs when a nerve has been compressed or damaged. Can knowing the symptoms and causes help in diagnosis and treatment?
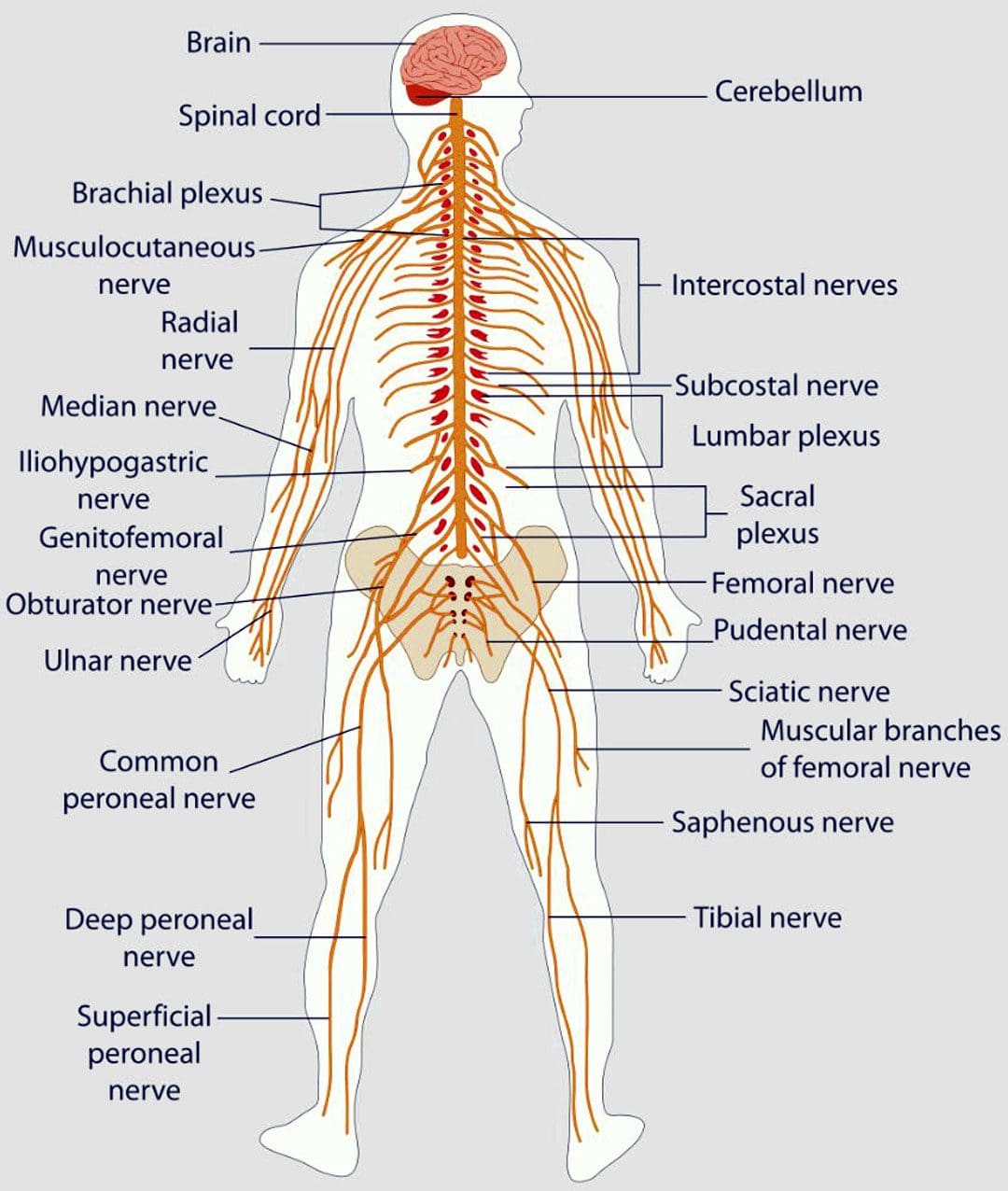
Table of Contents
Paresthesia Body Sensations
The numbness or tingling feeling when an arm, leg, or foot has fallen asleep is not so much about blood circulation but nerve function.
- Paresthesia is an abnormal sensation felt in the body due to the compression or irritation of nerves.
- It can be a mechanical cause like a compressed/pinched nerve.
- Or it may be due to a medical condition, injury, or illness.
Symptoms
Paresthesia can cause various symptoms. These symptoms can range from mild to severe and can be brief or long-lasting. Signs can include: (National Institute of Neurological Disorders and Stroke. 2023)
- Tingling
- Pins and needles sensations
- Feeling like the arm or leg has fallen asleep.
- Numbness
- Itching.
- Burning sensations.
- Difficulty contracting the muscles.
- Difficulty using the affected arm or leg.
- The symptoms typically last for 30 minutes or less.
- Shaking the affected limb often relieves the sensations.
- Paresthesia usually affects only one arm or leg at a time.
- However, both arms and legs can be affected, depending on the cause.
Consult a healthcare provider if the symptoms last for more than 30 minutes. Treatment may be required if paresthesia body sensations are brought on by a serious underlying cause.
Causes
Sitting with incorrect and unhealthy postures can compress a nerve and generate symptoms. However, some causes are more concerning and can include:
- Central nervous system conditions – stroke or multiple sclerosis/MS. (National Institute of Neurological Disorders and Stroke. 2023)
- Altered nerve function brought on by a condition, like diabetes.
- Compression or irritation of spinal nerve/s. (American Association of Neurological Surgeons. 2023)
- Tension and traction or pulling on a nerve.
Seeking Medical Assistance
If the symptoms don’t go away after 30 minutes or keep returning for unknown reasons, call a healthcare provider to find out what is causing the abnormal sensations. A worsening case should be monitored by a healthcare provider.
- Peripheral neuropathy caused by diabetes usually begins with a feeling of paresthesia in the foot/feet and can worsen and lead to other complications.
- This is a symptom that diabetes is poorly controlled and needs to be managed appropriately. (National Institute of Diabetes and Digestive and Kidney Diseases. 2018)
Diagnosis
A healthcare provider will work with the individual to understand the symptoms and perform the appropriate diagnostic tests to determine the cause. A healthcare provider will choose the tests based on a physical examination. Common diagnostic procedures include: (Merck Manual Professional Version. 2022)
- Magnetic resonance imaging – MRI of the spine, brain, or extremities.
- X-ray to rule out bone abnormalities, like a fracture.
- Blood tests.
- Electromyography – EMG studies.
- Nerve conduction velocity – NCV test.
- If paresthesia is accompanied by back or neck pain, a healthcare provider may suspect a compressed/pinched spinal nerve.
- If the individual has a history of diabetes that is poorly controlled, they may suspect peripheral neuropathy.
Treatment
Treatment for paresthesia depends on the diagnosis. A healthcare provider can help determine the best course of action for the specific condition.
Nervous System
- If symptoms are triggered by a central nervous condition like MS, individuals will work closely with their healthcare provider to get the appropriate treatment.
- Physical therapy could be recommended to help improve overall functional mobility. (Nazanin Razazian, et al., 2016)
Spinal Nerve
- If paresthesia is caused by compression of a spinal nerve, like sciatica, individuals may be referred to a chiropractor and physical therapy team to release the nerve and pressure. (Julie M. Fritz, et al., 2021)
- A physical therapist may prescribe spinal exercises to relieve compression of the nerve and restore normal sensations and motion.
- Strengthening exercises to restore flexibility and mobility may be prescribed if weakness presents along with paresthesia body sensations.
Herniated Disc
- If a herniated disc is causing the abnormal sensations, and there has been no improvement with conservative measures, a healthcare provider may suggest surgery to relieve pressure on the nerve/s. (American Association of Neurological Surgeons. 2023)
- In surgical procedures like a laminectomy or discectomy, the objective is to restore nerve function.
- Post-surgery, individuals may be recommended to a physical therapist to help regain mobility.
Peripheral Neuropathy
- If peripheral neuropathy from diabetes is the cause, the symptoms can become permanent and may change slightly with medication. (National Institute of Diabetes and Digestive and Kidney Diseases. 2018)
What Is Plantar Fasciitis?
References
National Institute of Neurological Disorders and Stroke. (2023) Paresthesia.
American Association of Neurological Surgeons. (2023) Herniated disc.
National Institute of Diabetes and Digestive and Kidney Diseases. (2018) Peripheral neuropathy.
Merck Manual Professional Version. (2022) Numbness.
Razazian, N., Yavari, Z., Farnia, V., Azizi, A., Kordavani, L., Bahmani, D. S., Holsboer-Trachsler, E., & Brand, S. (2016). Exercising Impacts on Fatigue, Depression, and Paresthesia in Female Patients with Multiple Sclerosis. Medicine and science in sports and exercise, 48(5), 796–803. https://doi.org/10.1249/MSS.0000000000000834
Fritz, J. M., Lane, E., McFadden, M., Brennan, G., Magel, J. S., Thackeray, A., Minick, K., Meier, W., & Greene, T. (2021). Physical Therapy Referral From Primary Care for Acute Back Pain With Sciatica : A Randomized Controlled Trial. Annals of internal medicine, 174(1), 8–17. https://doi.org/10.7326/M20-4187
Post Disclaimer
Professional Scope of Practice *
The information herein on "Tingling, Pins & Needles: Causes of Paresthesia in the Body" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.