Spinal trauma consists of spine fractures, or spinal fractures, and spinal cord injuries. Approximately 12,000 spinal trauma cases are reported in the United States every year. While the most prevalent causes of spinal cord injuries and spine fractures are automobile accidents and falls, spinal trauma can also be attributed to assault, sports injuries, and work-related accidents. Diagnosis of spinal trauma includes imaging and assessment of nerve function, such as reflex, motor, and sensation. The following article discusses the role of emergency radiology in spinal trauma. Chiropractic care can help provide diagnostic evaluations for spinal trauma.
Table of Contents
Abstract
Spinal trauma is very frequent injury with different severity and prognosis varying from asymptomatic condition to temporary neurological dysfunction, focal deficit or fatal event. The major causes of spinal trauma are high- and low- energy fall, traffic accident, sport and blunt impact. The radiologist has a role of great responsibility to establish the presence or absence of lesions, to define the characteristics, to assess the prognostic influence and therefore treatment. Imaging has an important role in the management of spinal trauma. The aim of this paper was to describe: incidence and type of vertebral fracture; imaging indication and guidelines for cervical trauma; imaging indication and guidelines for thoracolumbar trauma; multidetector CT indication for trauma spine; MRI indication and protocol for trauma spine.
Introduction
The trauma of the spine weighs heavily on the budget of social and economic development of our society. In the USA, 15–40 cases per million populations with 12,000 cases of paraplegia every year, 4000 deaths before admission and 1000 deaths during hospitalization are estimated. The young adult population is the most frequently involved in road accidents, followed by those at home and at work, with a prevalence of falls from high and sports injuries.1
Imaging has an important role in the management of spinal trauma. Quick and proper management of the patients with trauma, from diagnosis to therapy, can mean reduction of the neurological damage of vital importance for the future of the patient. Radiologists have a role of great responsibility to establish the presence or absence of lesions, defining the characteristics, assessing the prognostic influence and therefore treatment.
The aim of this paper was to describe:
- incidence and type of vertebral fracture
- imaging indication and guidelines for cervical trauma
- imaging indication and guidelines for thoracolumbar trauma
- multidetector CT (MDCT) pattern for trauma spine
- MRI pattern for trauma spine.
Spinal trauma, including spine fractures and spinal cord injuries, represent about 3 percent to 6 percent of all skeletal injuries. Diagnostic assessments are fundamental towards the complex diagnosis of spinal trauma. While plain radiography is the initial diagnostic modality used for spine fractures and/or spinal cord injuries, CT scans and MRI can also help with diagnosis. As a chiropractic care office, we can offer diagnostic assessments, such as X-rays, to help determine the best treatment.
Vertebral Fracture Management and Imaging Indication and Evaluation
The rationale of imaging in spinal trauma is:
- To diagnose the traumatic abnormality and characterize the type of injury.
- To estimate the severity, potential spinal instability or damaged stability with or without neurological lesion associated, in order to avoid neurological worsening with medical legal issue.
- To evaluate the state of the spinal cord and surrounding structures (MR is the gold standard technique).
Clinical evaluation involving different specialities—emergency medicine, trauma surgery, orthopaedics, neurosurgery and radiology or neuroradiology—and trauma information is the most important key point in order to decide when and which type of imaging technique is indicated.2
A common question in patients with spine trauma is: is there still a role for plain-film X-ray compared with CT?
In order to clarify when and what is more appropriate for spinal trauma, different guidelines were published distinguishing cervical and thoracolumbar level.
Cervical Spinal Trauma: Standard X-Ray and Multidetector CT Indication
For cervical level, controversy persists regarding the most efficient and effective method between cervical standard X-ray with three film projections (anteroposterior and lateral view plus open-mouth odontoid view) and MDCT.
X-ray is generally reserved for evaluating patients suspected of cervical spine injury and those with injuries of the thoracic and lumbar areas where suspicion of injury is low. Despite the absence of a randomized controlled trial and thanks to the high quality and performance of MDCT and its post-processing (multiplanar reconstruction and three-dimensional volume rendering), the superiority of cervical CT (CCT) compared with cervical standard X-ray for the detection of clinically significant cervical spine injury is well demonstrated.
In order to reduce the patient radiation exposure, it is important to determine and to select patients who need imaging and those who do not, through the clinical evaluation and probability of cervical spine injury, using only MDCT for the appropriate patient as is more cost-effective screening.3
First of all, it is necessary to distinguish the type of trauma:
- minor trauma (stable patient, mentally alert, not under the influence of alcohol or other drugs and who has no history or physical findings suggesting a neck injury)
- major and severe trauma (multitrauma, unstable patient with a simple temporary neurological dysfunction, with focal neurological deficit or with a history or mechanism of injury sufficient to have exceeded the physiologic range of motion).
Second, it is important to establish if trauma risk factors are presents, such as:
- violence of trauma: high-energy fall (high risk) or low-energy fall (low risk)
- age of the patient: <5years old, >65 years oldÂ
- associated lesions: head, chest, abdomen (multitrauma) etc.
- clinical signs: Glasgow Coma Scale (GCS), neurological deficit, vertebral deformation.
Combining these elements, patients can be divided into “low
risk†and “high risk†for cervical injury.
The first group consists of patients who are awake (GCS 15), alert, cooperative and non-intoxicated without any distract- ing injury.
The second group consists of unconscious, sedated, intoxicated or non-cooperative patients or those with a distracting injury or an altered mental state (GCS ,15) with a 5% chance of cervical spine injuries.3,4
CCT has a wider indication than X-ray for patients at very high risk of cervical spine injury (major trauma or multitrauma). No evidence suggests CCT instead of X-ray for a patient who is at low risk for cervical spine injury.5

In 2000, the National Emergency X-Radiography Utilization (NEXUS) study, analysing 34,069 patients, established low-risk criteria to identify patients with a low probability of cervical spine injury, who consequently needed no cervical spine imaging. To meet the NEXUS criteria, a patient must have the following conditions:
- no tenderness at the posterior midline of the cervical spine
- no focal neurologic deficit
- normal level of alertness
- no evidence of intoxication
- no clinically apparent painful injury that might distract the patient from the pain of a cervical spine injury.6
If all of these roles are present, the patient does not need to undergo X-ray because he has a low possibility of having a cervical spine injury with a sensitivity of 99% and a specificity of 12.9%.7
In 2001, the Canadian C-spine rule (CCSR) study developed a second decision rule using the risk factor of the trauma: three high-risk criteria (age $ 65 years, dangerous mechanism and paraesthesias in extremities), five low-risk criteria (simple rear-end motor vehicle collision, sitting position in emergency department, ambulatory at any time, delayed onset of neck pain and absence of midline cervical spine tenderness) and the ability of the patient to actively rotate his or her neck to determine the need for cervical spine radiography. In practice, if one of these risk factors is present, the patient needs to undergo imaging evaluation. On the other hand, if the risk factors are not present, the use of the NEXUS criteria plus a functional evaluation of the cervical spine is needed (left and right cervical spine rotation .45°); if this functional evaluation is possible, imaging is unnecessary. If an incomplete cervical movement is present, then the patient needs to be checked with imaging. The results showed the criteria to have a sensitivity of up to 100% and a specificity of up to 42.5%.8
Applying these criteria, before cervical spine imaging, the authors report a decrease of about 23.9% in the number of negative CCT, and applying a more liberal NEXUS criteria including the presence or absence of pain, limited range of motion or posterolateral cervical spine tenderness, they report a decrease of up to 20.2% in the number of negative studies.2
If these clinical criteria cannot be applied, CCT must be performed.
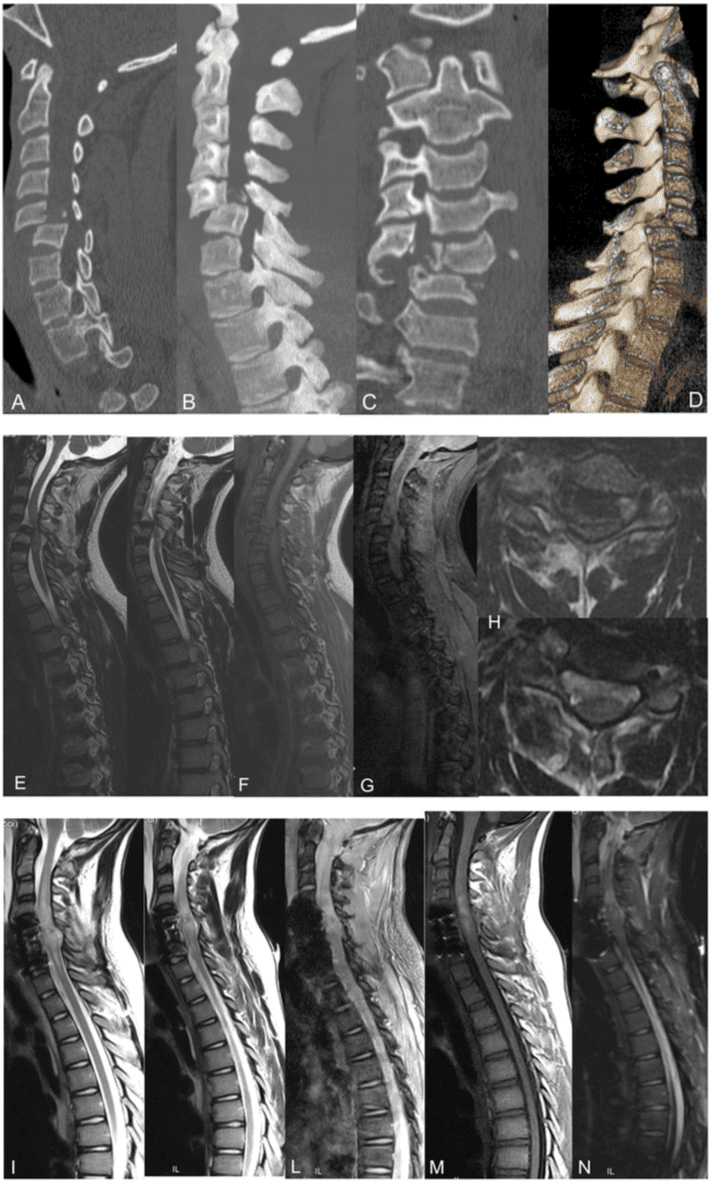
Major and severe traumas request a direct CCT screening, especially because there could be associated lesions, according to the high-risk criteria developed by Blackmore and Hanson to identify patients with trauma at high risk of c-spine injury who would benefit from CT scanning as the primary radiological investigation9 Figure 1.
Thoracolumbar Spinal Trauma: Standard X-Ray and Multidetector CT Indication
For thoracolumbar level, MDCT is a better examination for depicting spine fractures than conventional radiography. It has wider indication in the diagnosis of patients with thoracolumbar trauma for bone evaluation. It is faster than X-ray, more sensitive, thanks to multiplanar reformatted or volume-rendering reconstruction detecting small cortical fracture, and the sagittal alignment can be evaluated with a wide segment evaluation.10
It can replace conventional radiography and can be performed alone in patients who have sustained severe trauma.10
In fact, thoracolumbar spinal injuries can be detected during visceral organ-targeted CT protocol for blunt traumatic injury.
Thanks to multidetector technology, images reconstructed using a soft algorithm and wide-display field of view that covers the entire abdomen using a visceral organ-targeted protocol with 1.5-mm collimation are sufficient for the evaluation of spine fractures in patients with trauma, given that multiplanar reformatted images are provided without performing new CT study and without increasing radiation dose11 Figure 2.
With MDCT there is no information about spinal cord status or ligament lesion or acute epidural haematoma; it can only evaluate bone status. Spinal cord injury is suspected only by clinical data.
CCT is strictly recommended in patients affected by blunt cerebrovascular injuries. Both lesions can be strictly correlated and generally; contrast medium administration to exclude hemorrhagic brain lesion and cervical fracture is not needed.10
Magnetic resonance imaging, or MRI, is a medical diagnostic assessment technique utilized in radiology to create pictures of the anatomy and the physiological processes of the human body. Alongside radiography and CT scans, MRI can be helpful in the diagnosis of spinal trauma, including spine fractures and spinal cord injuries. Magnetic resonance imaging may not be necessary for all cases of spinal trauma. However, it could provide detailed information on the other soft tissues of the spine.Â
Spinal Trauma and MRI
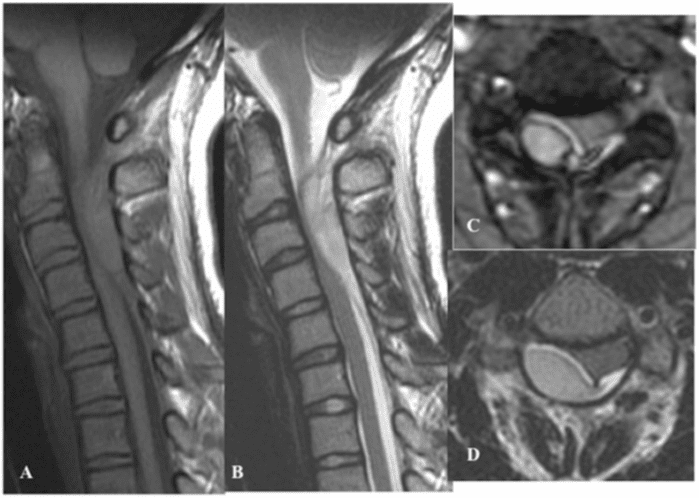
Even if MDCT is the first imaging modality in a patient with trauma, MRI is essential for the soft assessment of the ligament, muscle or spinal cord injury, spinal cord, disc, ligaments and neural elements, especially using T2 weighted sequences with fat suppression or T2 short tau inversion recovery (STIR) sequence.12 MRI is also used to classify burst fracture, obtaining information about the status of the posterior ligamentous complex, a critical determinant of surgical indication even if the diagnosis of ligament injuries remains complex, and its grade is also underestimated using high-field MRI.13
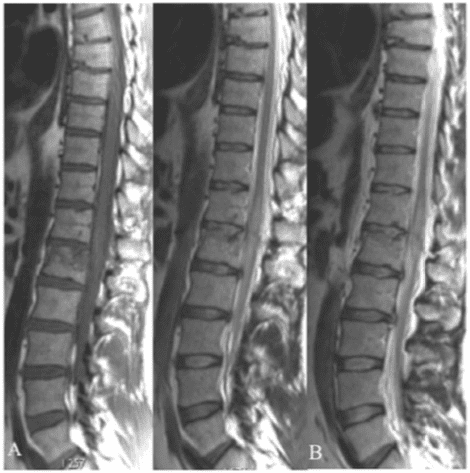
In the management of patients with polytrauma, MDCT total-body scan is necessary in an emergency condition, and MRI whole-spine indication is secondary to the clinical status of the patient: spinal cord compression syndrome Figure 3–5 MRI protocols recommended for patients affected by spinal injury and trauma are the following:13,14
- Sagittal T1 weighted, T2 weighted and STIR sequence for the bone marrow and spinal cord injury or spinal cord compression evaluation owing to epidural haematoma or traumatic herniated disc
- Sagittal gradient echo T2* sequence for haemorrhage evaluation of the spinal cord or into the epidural–subdural space
- Sagittal diffusion-weighted imaging helpful when evaluating spinal cord injury, differentiating cytotoxic from vasogenic oedema, assisting in detecting intramedullary haemorrhage. It can help to evaluate the degree of compressed spinal cord.
- Axial T1 weighted and T2 weighted sequence for the right localization of the injury. Recently, for patients affected by acute blunt trauma and cervical spinal cord injury, the axial T2 weighted sequence has been shown to be important for trauma-predicting outcomes. On axial T2 weighted imaging, five patterns of intramedullary spinal cord signal alteration can be distinguished at the injury’s epicentre. Ordinal values ranging from 0 to 4 can be assigned to these patterns as Brain and Spinal Injury Center scores, which encompassed the spectrum of spinal cord injury severity correlating with neurological symptoms and MRI axial T2 weighted imaging. This score improves on current MRI-based prognostic descriptions for spinal cord injury by reflecting functionally and anatomically significant patterns of intramedullary T2 signal abnormality in the axial plane.15
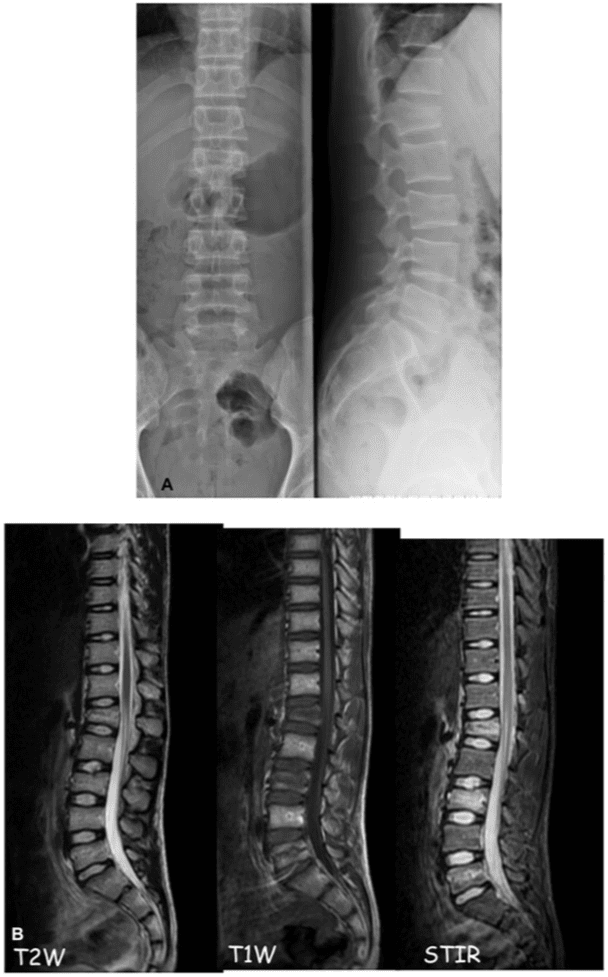
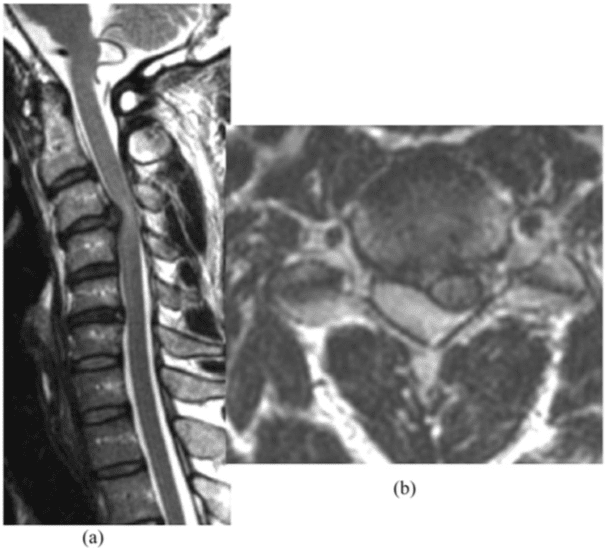
MRI has also an important role in case of discordance between clinical status and CT imaging. In the absence of vertebral fracture, patients can suffer from back pain resistant to medical therapy owing to bone marrow traumatic oedema that can be detected only using STIR sequence on MRI Figure 6.
In spinal cord injury without radiologic abnormalities (SCI- WORA), MRI is the only imaging modality that can detect intramedullary or extramedullary pathologies or show the absence of neuroimaging abnormalities.16 SCIWORA refers to spinal injuries, typically located in the cervical region, in the absence of identifiable bony or ligamentous injury on complete, technically adequate, plain radiographs or CT. SCIWORA should be suspected in patients subjected to blunt trauma who report early or transient symptoms of neurologic deficit or who have existing findings upon initial assessment.17
Vertebral Fracture Type and Classification
The rationale of imaging is to distinguish the vertebral fracture type into two groups:
• vertebral compression fracture as vertebral body fracture
compressing the anterior cortex, sparing the middle posterior
columns associated or not with kyphosis
• burst fracture as comminuted fracture of the vertebral body
extending through both superior and inferior endplates with kyphosis or posterior displacement of the bone into the canal. and to distinguish which type of treatment the patient needs; by imaging, it is possible to classify fractures into stable or unstable fracture, giving indication to conservative or surgical therapy.

Using MDCT and MRI, thanks to morphology and injury distribution, various classification systems have been used for identifying those injuries that require surgical intervention, distinguishing among stable and unstable fractures and surgical and non-surgical fractures.1
Denis proposed the “three-column conceptâ€, dividing the spinal segment into three parts: anterior, middle and posterior columns. The anterior column comprises the anterior longitudinal ligament and anterior half of the vertebral body; the middle column comprises the posterior half of the vertebral body and posterior longitudinal ligament; and the posterior column comprises the pedicles, facet joints and supraspinous ligaments. Each column has different contributions to stability, and their damages may affect stability differently. Generally, if two or more of these columns are damaged, the spine becomes unstable.18
Magerl divided the vertebral compression fracture (VCF) into three main categories according to trauma force: (a) compression injury, (b) distraction injury and (c) rotation injury. Type A has conservative or non-surgical mini-invasive treatment indication.19
The thoracolumbar injury classification and severity score (TLICS) system assigns numerical values to each injury based on the categories of morphology of injury, integrity of the posterior ligament and neurological involvement. Stable injury patterns (TLICS,4) may be treated non-operatively with brace immobilization. Unstable injury patterns (TLICS.4) may be treated operatively with the principles of deformity correction, neurological decompression if necessary and spinal stabilization.20
The Aebi classification is based on three major groups: A = isolated anterior column injuries by axial compression, B = disruption of the posterior ligament complex by distraction posteriorly and C = corresponding to group B but with rotation. There is an increasing severity from A to C, and within each group, the severity usually increases within the subgroups from 1 to 3. All these pathomorphologies are supported by the mechanism of injury, which is responsible for the extent of the injury. The type of injury with its groups and subgroups is able to suggest the treatment modality.21
Thoracolumbar Fracture and Mini-Invasive Vertebral Augmentation Procedure: Imaging Target
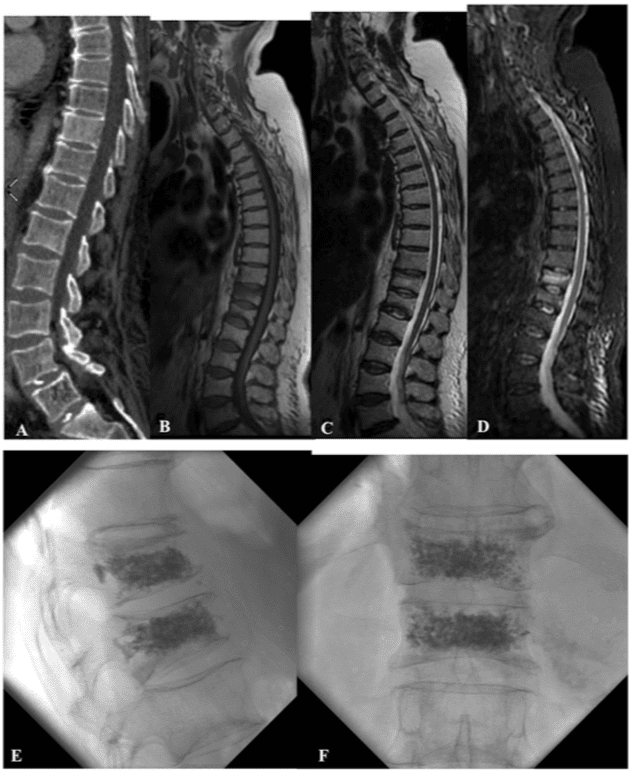
Recently, different mini-invasive procedures called assisted- technique vertebroplasty (balloon kyphoplasty KP or kyphoplasty-like techniques) have been developed in order to obtain pain relief and kyphosis correction as alternative treatment for non-surgical but symptomatic vertebral fracture.
The rationale of these techniques is to combine the analgesic and vertebral consolidation effect of vertebroplasty with the restoration of the physiological height of the collapsed vertebral body, reducing the kyphotic deformity of the vertebral body, delivering cement into the fractured vertebral body with a vertebral stabilization effect compared with conservative therapy (bed rest and medical therapy).22
From interventional point of view, imaging has an important role for treatment indication together with clinical evaluation. Both MDCT and MRI are recommended Figure 7 and 8.
In fact, MDCT has the advantage of diagnosing VCF with kyphosis deformity easily, while MRI with STIR sequence is useful to evaluate bone marrow oedema, an important sign of back pain.
Patients affected by vertebral fracture without bone marrow oedema on STIR sequence are not indicated for interventional procedure.
According to imaging, Magerl A1 classification fractures are the main indication of treatment.
However, the treatment must be performed within 2–3 weeks from trauma in order to avoid sclerotic bone response: the younger the fractures, the better the results and easier the treatment and vertebral augmentation effect. To exclude sclerotic bone reaction, CT is recommended.
Conclusion
The management of spinal trauma remains complex. MDCT has a wide indication for bone evaluation in patients affected by severe trauma or patients with high risk of spine injury. MRI has a major indication in the case of spinal cord injury and the absence of bone lesion. Diagnostic assessment of spinal trauma, including radiography, CT scans, and MRI are fundamental towards the diagnosis of spine fractures and spinal cord injury for treatment. The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
1. Pneumaticos SG, Triantafyllopoulos GK, Gian- noudis PV. Advances made in the treatment of thoracolumbar fractures: current trends and future directions. Injury 2013; 44: 703–12. doi: 10.1016/j.injury.2012.12.005
2. Griffith B, Bolton C, Goyal N, Brown ML, Jain R. Screening cervical spine CT in a level I trauma center: overutilization? AJR Am J Roentgenol 2011; 197: 463–7.doi: 10.2214/ AJR.10.5731
3. Hanson JA, Blackmore CC, Mann FA, Wilson AJ. Cervical spine injury: a clinical decision rule to identify high-risk patients for helical CTscreening. AJR Am J Roentgenol 2000; 174: 713–17.
4. Saltzherr TP, Fung Kon Jin PH, Beenen LF, Vandertop WP, Goslings JC. Diagnostic imaging of cervical spine injuries following blunt trauma: a review of the literature and practical guideline. Injury 2009; 40: 795–800. doi: 10.1016/j.injury.2009.01.015
5. Holmes JF, Akkinepalli R. Computed to- mography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma 2005; 58: 902–5. doi: 10.1097/01. TA.0000162138.36519.2A
6. Hoffman JR, Wolfson AB, Todd K, Mower WR. Selective cervical spine radiography in blunt trauma: methodology of the National Emergency X-Radiography Utilization Study (NEXUS). Ann Emerg Med 1998; 32: 461–9. doi: 10.1016/S0196-0644(98)70176-3
7. Dickinson G, Stiell IG, Schull M, Brison R, Clement CM, Vandemheen KL, et al. Retro- spective application of the NEXUS low-risk criteria for cervical spine radiography in Canadian emergency departments. Ann Emerg Med 2004; 43: 507–14. doi: 10.1016/j. annemergmed.2003.10.036
8. Stiell IG, Wells GA, Vandemheen KL, Clem- ent CM, Lesiuk H, De Maio VJ, et al. The Canadian C-spine rule for radiography in
alert and stable trauma patients. JAMA 2001;
286: 1841–8. doi: 10.1001/jama.286.15.1841 9. Berne JD, Velmahos GC, El-Tawil Q, Deme- triades D, Asensio JA, Murray JA, et al. Value
of complete cervical helical computed to- mographic scanning in identifying cervical spine injury in the unevaluable blunt trauma patient with multiple injuries: a prospective study. J Trauma 1999; 47: 896–902. doi: 10.1097/00005373-199911000-00014
10. Wintermark M, Mouhsine E, Theumann N, Mordasini P, van Melle G, Leyvraz PF, et al. Thoracolumbar spine fractures in patients who have sustained severe trauma: depiction with multi-detector row CT. Radiology 2003; 227: 681–9. doi: 10.1148/radiol.2273020592
11. Kim S, Yoon CS, Ryu JA, Lee S, Park YS, Kim SS, et al. A comparison of the diagnostic performances of visceral organ-targeted ver- sus spine-targeted protocols for the evalua- tion of spinal fractures using sixteen-channel multidetector row computed tomography: is additional spine-targeted computed tomog- raphy necessary to evaluate thoracolumbar spinal fractures in blunt trauma victims? J Trauma 2010; 69: 437–46. doi: 10.1097/ TA.0b013e3181e491d8
12. Pizones J, Castillo E. Assessment of acute thoracolumbar fractures: challenges in mul- tidetector computed tomography and added value of emergency MRI. Semin Musculoskelet Radiol 2013; 17: 389–95. doi: 10.1055/s- 0033-1356468
13. Emery SE, Pathria MN, Wilber RG, Masaryk T, Bohlman HH. Magnetic resonance imag- ing of posttraumatic spinal ligament injury. J Spinal Disord 1989; 2: 229–33. doi: 10.1097/ 00002517-198912000-00003
14. Zhang JS, Huan Y. Multishot diffusion- weighted MR imaging features in acute trauma of spinal cord. Eur Radiol 2014; 24: 685–92. doi: 10.1007/s00330-013-3051-3
15. Talbott JF, Whetstone WD, Readdy WJ, Ferguson AR, Bresnahan JC, Saigal R, et al. The Brain and Spinal Injury Center score:
a novel, simple, and reproducible method for assessing the severity of acute cervical spinal cord injury with axial T2-weighted MRI findings. J Neurosurg Spine 2015; 23: 495–504. doi: 10.3171/2015.1.SPINE141033
16. Boese CK, Oppermann J, Siewe J, Eysel P, Scheyerer MJ, Lechler PJ. Spinal cord injury without radiologic abnormality in children: a systematic review and meta-analysis. Trauma Acute Care Surg 2015; 78: 874–82. doi: 10.1097/TA.0000000000000579
17. Brown RL, Brunn MA, Garcia VF. Cervical spine injuries in children: a review of
103 patients treated consecutively at a level 1 pediatric trauma center. J Pediatr Surg 2001; 36: 1107–14. doi: 10.1053/jpsu.2001.25665
18. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983; 8: 817–31. doi: 10.1097/ 00007632-198311000-00003
19. Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 1994; 3: 184–201.
20. Patel AA, Dailey A, Brodke DS, Daubs M, Harrop J, Whang PG, et al; Spine Trauma Study Group. Thoracolumbar spine trauma classification: the Thoracolumbar Injury Classification and Severity Score system and case examples. J Neurosurg Spine 2009; 10: 201–6. doi: 10.3171/2008.12.SPINE08388
21. Aebi M. Classification of thoracolumbar fractures and dislocations. Eur Spine J 2010; 19(Suppl. 1): S2–7. doi: 10.1007/s00586-009-1114-6
22. Muto M, Marcia S, Guarnieri G, Pereira V. Assisted techniques for vertebral cementoplasty: why should we do it? Eur J Radiol 2015; 84: 783–8. doi: 10.1016/j.ejrad.2014.04.002

Additional Topics: Acute Back Pain
Back pain is one of the most prevalent causes of disability and missed days at work worldwide. Back pain attributes to the second most common reason for doctor office visits, outnumbered only by upper-respiratory infections. Approximately 80 percent of the population will experience back pain at least once throughout their life. The spine is a complex structure made up of bones, joints, ligaments, and muscles, among other soft tissues. Because of this, injuries and/or aggravated conditions, such as herniated discs, can eventually lead to symptoms of back pain. Sports injuries or automobile accident injuries are often the most frequent cause of back pain, however, sometimes the simplest of movements can have painful results. Fortunately, alternative treatment options, such as chiropractic care, can help ease back pain through the use of spinal adjustments and manual manipulations, ultimately improving pain relief.

EXTRA IMPORTANT TOPIC: Sciatica Pain Chiropractic Therapy
Post Disclaimer
Professional Scope of Practice *
The information herein on "The Role of Emergency Radiology in Spinal Trauma" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.