Individuals that experience nerve pain in the foot could be caused by a number of different conditions, can recognizing the most common causes help in developing an effective treatment plan?
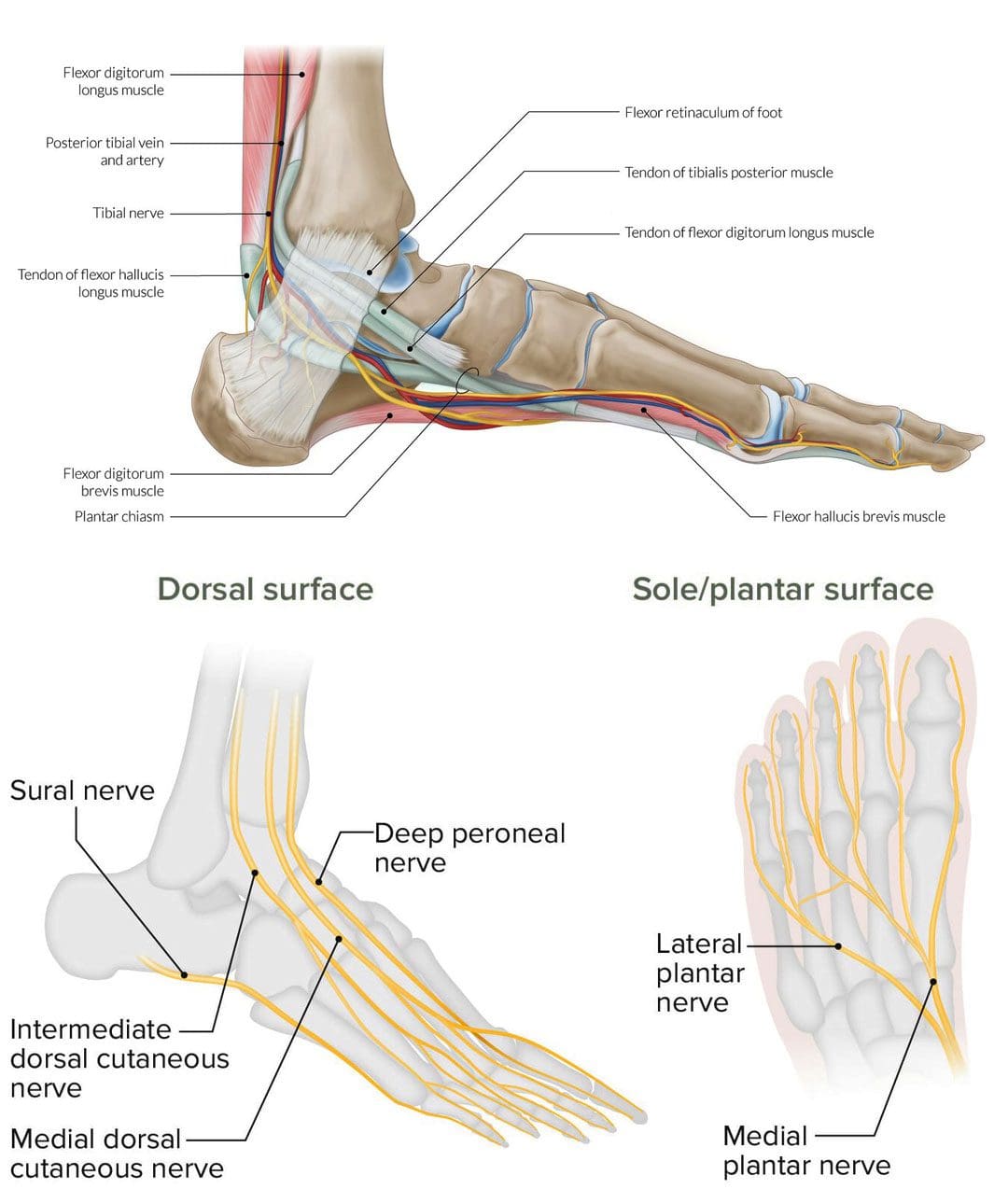
Table of Contents
Nerve Pain In The Foot
These sensations can feel like a burning, shooting, electrical, or stabbing pain and can happen while in motion or at rest. It can occur on the top of the foot or through the arch. The area closest to the nerve may be sensitive to the touch. A number of different conditions can cause nerve pain in the foot, including:
- Morton’s neuroma
- Pinched nerve
- Tarsal tunnel syndrome
- Diabetic peripheral neuropathy
- Herniated disc
Morton’s Neuroma
Morton’s neuroma involves the nerve that runs between the third and fourth toes, but can sometimes occur between the second and third toes becoming thicker. Typical symptoms include a burning or shooting pain in the area, usually while walking. (Nikolaos Gougoulias, et al., 2019) Another common symptom is the sensation of pressure beneath the toes like the sock is bunched up underneath. Treatments can include:
- Arch supports
- Cortisone injections to decrease swelling
- Footwear modifications – can include lifts, orthotics combined with metatarsal pads, and rocker soles, to provide cushion where needed.
Things that increase the risk of developing the condition include:
- Regularly wearing high-heels – the condition occurs more frequently in women.
- Shoes that are too tight.
- Participating in high-impact sports like running.
- Having flat feet, high arches, bunions, or hammertoes.
Pinched Nerve
A pinched nerve can feel like shooting or burning pain. Nerve entrapment can occur in various regions of the foot or the area on top of the foot may feel sensitive. Causes can be caused by: (Basavaraj Chari, Eugene McNally. 2018)
- Trauma that causes swelling.
- Blunt impact.
- Tight shoes.
Treatment can include:
- Massage
- Physical therapy
- Rest
- Footwear modifications
- Anti-inflammatories.
Things that increase the risk of developing a pinched nerve in the foot include:
- Poor-fitting footwear.
- Repetitive stress injury.
- Trauma to the foot.
- Obesity.
- Rheumatoid arthritis.
Tarsal Tunnel Syndrome
Another type of nerve entrapment is tarsal tunnel syndrome. Tarsal tunnel syndrome is “anything that produces compression on the posterior tibial nerve.” (American College of Foot and Ankle Surgeons. 2019) The tibial nerve is located near the heel. Symptoms include numbness and foot cramps, burning, tingling, or shooting sensations that often radiate from the instep/arch. Both can worsen while the foot is at rest, like when sitting or sleeping. Treatment can consist of:
- Placing padding in the shoe where the foot is being compressed to relieve the pain.
- Custom foot orthotics.
- Cortisone shots or other anti-inflammatory treatments.
- Surgery may be necessary to release the nerve.
Conditions that compress the tibial nerve and can lead to tarsal tunnel syndrome include:
- Flat feet
- Fallen arches
- Ankle sprain
- Diabetes
- Arthritis
- Varicose veins
- Bone spurs
Diabetic Peripheral Neuropathy
Long-term high blood sugar/glucose associated with diabetes can lead to a form of nerve damage known as peripheral neuropathy. (Centers for Disease Control and Prevention. 2022) Neuropathy pain feels like burning or shooting pain, or the sensation of walking on bubble wrap that usually shows up overnight. The pain can come and go as well as a gradual loss of feeling in the feet that begins in the toes and moves up the foot. It’s estimated that around half of individuals with diabetes will eventually develop neuropathy. (Eva L. Feldman, et al., 2019) Treatments can include:
- Physical therapy massage to increase circulation.
- Topical treatments with capsaicin.
- Vitamin B.
- Blood sugar management.
- Alpha lipoic acid.
- Medication.
Individuals with diabetes have an increased risk of developing peripheral neuropathy if:
- Blood sugar is not well-controlled.
- Diabetes has been present for many years.
- Kidney disease.
- Smoke.
- Overweight or obese.
Herniated Disc
Nerve pain in the foot can be caused by spinal issues. A herniated disc in the lower back can irritate and compress the nerves, causing pain that radiates down the leg and foot. Additional symptoms usually include muscle weakness in the legs and/or numbness and tingling. Most herniated discs don’t require surgery and get better with conservative treatment. (Wai Weng Yoon, Jonathan Koch. 2021) If symptoms don’t improve or worsen, a healthcare provider may recommend surgery. Herniated discs are most common in young and middle-aged adults. Increased chances of developing a herniated disc can come from:
- Degenerative changes in the spine from normal age wear and tear.
- Physically demanding job.
- Lifting incorrectly.
- Overweight or obese.
- Genetic predisposition – family history of herniated discs.
Spinal Stenosis
Spinal stenosis occurs when the spaces in the spine begin to narrow, creating pressure on the spinal cord and nerve roots. It is usually caused by wear and tear on the spine as the body ages. Stenosis in the lower back can cause burning pain in the buttocks and leg. As it progresses pain can radiate into the feet along with numbness and tingling. Conservative treatment consists of physical therapy exercises and non-steroidal anti-inflammatory medications/NSAIDs. (Jon Lurie, Christy Tomkins-Lane. 2016) Cortisone injections can be beneficial and if the condition worsens, surgery may be an option. Risk factors include:
- Age 50 or older.
- A narrow spinal canal.
- Previous injury.
- Previous spinal surgery.
- Osteoarthritis that is affecting the back.
Other Possible Causes
Other conditions can result in nerve damage and pain symptoms and sensations. Examples include: (Nathan P. Staff, Anthony J. Windebank. 2014)
- Vitamin deficiencies (Nathan P. Staff, Anthony J. Windebank. 2014)
- Physical trauma – after surgery or an automobile or sports accident.
- Certain cancer, antiviral medications, or antibiotics.
- Complex regional pain syndrome.
- Tumors that irritate and/or compress a nerve.
- Liver or kidney disease.
- Infectious diseases – Lyme disease complications or viral infections.
Nerve pain in the foot is definitely a reason to see a healthcare provider. Early diagnosis can help prevent symptom progression and future problems. Once the cause of the pain has been identified, the healthcare team can work together to develop a personalized treatment plan to release compressed nerves and restore mobility and function. See a healthcare provider right away if the pain and symptoms worsen, or if there are difficulties standing or walking.
Chiropractic After Accidents and Injuries
References
Gougoulias, N., Lampridis, V., & Sakellariou, A. (2019). Morton’s interdigital neuroma: instructional review. EFORT open reviews, 4(1), 14–24. https://doi.org/10.1302/2058-5241.4.180025
Chari, B., & McNally, E. (2018). Nerve Entrapment in Ankle and Foot: Ultrasound Imaging. Seminars in musculoskeletal radiology, 22(3), 354–363. https://doi.org/10.1055/s-0038-1648252
American College of Foot and Ankle Surgeons. Tarsal tunnel syndrome.
Centers for Disease Control and Prevention. Diabetes and nerve damage.
Feldman, E. L., Callaghan, B. C., Pop-Busui, R., Zochodne, D. W., Wright, D. E., Bennett, D. L., Bril, V., Russell, J. W., & Viswanathan, V. (2019). Diabetic neuropathy. Nature reviews. Disease primers, 5(1), 42. https://doi.org/10.1038/s41572-019-0097-9
Yoon, W. W., & Koch, J. (2021). Herniated discs: when is surgery necessary?. EFORT open reviews, 6(6), 526–530. https://doi.org/10.1302/2058-5241.6.210020
Lurie, J., & Tomkins-Lane, C. (2016). Management of lumbar spinal stenosis. BMJ (Clinical research ed.), 352, h6234. https://doi.org/10.1136/bmj.h6234
Staff, N. P., & Windebank, A. J. (2014). Peripheral neuropathy due to vitamin deficiency, toxins, and medications. Continuum (Minneapolis, Minn.), 20(5 Peripheral Nervous System Disorders), 1293–1306. https://doi.org/10.1212/01.CON.0000455880.06675.5a
Post Disclaimer
Professional Scope of Practice *
The information herein on "The Causes and Symptoms of Nerve Pain in the Foot" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.