Table of Contents
What Happens to Your Spine After a Work Injury, Car Crash, Sports Impact, or Fall?

Overview
High-impact events—like a rear-end collision, a hard fall, or a football tackle—load your spine very fast. Your neck and back can bend, stretch, twist, and compress in the blink of an eye. These forces can strain muscles, sprain ligaments, shift joints out of normal alignment, herniate discs, fracture vertebrae, or, in severe cases, injure the spinal cord. When the spinal cord is affected, changes in strength, sensation, and even paralysis can occur. Concussions and traumatic brain injuries (TBIs) often happen in the same split-second because the head whips and the brain moves inside the skull. (Mayo Clinic, 2024; UT Southwestern Medical Center, n.d.; van den Hauwe et al., 2020). Mayo Clinic+2UT Southwestern Medical Center+2
This article explains, in simple terms, what those forces do to the spine and nerves, how doctors evaluate these injuries, and where integrative chiropractic care can fit safely inside a team-based plan.
The Spine Under Sudden Force: What Actually Happens
The core forces
In a crash or fall, the neck and back experience flexion (bending), extension (arching back), rotation (twisting), shear (sliding), and compression (squeezing). A fast “snap” into extension—common in rear-end collisions—can overstretch the front of the neck and pinch structures in the back. Rotational and compressive loads can cause bulging or rupture of discs and stress the facet joints. (Weiss & Anderson, 2024; van den Hauwe et al., 2020). MDPI+1
Why these forces are so common
Most spine trauma comes from motor-vehicle collisions, falls, and sports. Epidemiology studies across large reviews indicate MVAs as the leading cause, followed by falls and sports-related injuries. (van den Hauwe et al., 2020). NCBI
Common Injury Patterns (From “Mild” to Severe)
1) Soft-tissue injuries: strains, sprains, and whiplash
-
Muscle strains and ligament sprains develop when tissues are stretched past their normal length.
-
Whiplash describes the acceleration-deceleration of the neck, resulting in micro-tearing of the soft tissues. Symptoms include neck pain, stiffness, headaches, and reduced motion. Rear-end collisions are classic triggers. (Casper & de Toledo, n.d.; Brain and Spinal Cord, n.d.). Northwest Florida Physicians Group
2) Joint dysfunction and “subluxation” (misalignment)
High-speed forces can disturb the normal glide of small spinal joints (facet joints) and the alignment of motion segments. In pediatrics and teens—especially with TBI—upper-cervical instability patterns can appear, including atlanto-occipital and atlantoaxial problems, which require careful medical assessment. (Weiss & Anderson, 2024). MDPI
3) Disc injuries (bulge or herniation)
A disc herniation happens when the disc’s inner gel pushes through the outer ring, sometimes contacting a nerve root and causing radiating pain, tingling, or weakness. Sudden compression and twist increase risk. (General clinical overviews). Invalid URL
4) Fractures of the spine
Crashes and high-energy sports can cause compression, burst, teardrop, and “Hangman” (C2) fractures. Hangman fractures result from forceful hyperextension (e.g., whiplash) and may be treated with immobilization or, if unstable, surgery. (Weiss & Anderson, 2024). MDPI
5) Spinal cord injury (SCI)
When impact compresses or bruises the cord, the function below the injury can change.
-
Complete SCI: No motor/sensory function below the injury.
-
Incomplete SCI: Some function remains.
Typical causes include MVAs, sports, and falls. Emergency care focuses on stabilization, preventing secondary damage, and rapid imaging. (UT Southwestern Medical Center, n.d.; Mayo Clinic, 2024). UT Southwestern Medical Center+1
6) Blood vessel injuries to neck arteries (BCVI)
High-energy neck trauma can injure the carotid or vertebral arteries, raising the risk of stroke hours to days later—even when the initial neck exam seems mild. Guidelines recommend CT angiography screening in high-risk cases and early antithrombotic therapy when safe. (Brommeland et al., 2018; Stone et al., 2018). PubMed+1
Brain–Spine Link: Why Concussions Travel with Neck Injuries
The same sudden stop or twist that loads the neck also moves the brain inside the skull. During fast deceleration or rotation, delicate brain fibers can stretch or shear. That is why concussion or TBI can occur alongside neck injuries. Some pediatric and sports scenarios show overlap between cervical spine injuries and TBI, which complicates diagnosis and recovery planning. (Weiss & Anderson, 2024; Weill Cornell Medicine Neurological Surgery, n.d.; Physio-Pedia, n.d.). MDPI+2Weill Cornell Neurosurgery+2
Red-Flag Symptoms: When to Seek Emergency Care
Call emergency services or go to the ER after trauma if you notice:
-
Profound neck or back pain with numbness, weakness, or paralysis in the arms/legs
-
Loss of bladder or bowel control
-
Severe headache, confusion, repeated vomiting, or loss of consciousness
-
Worsening neck pain with limited motion after a crash or fall
These can signal SCI or significant nerve involvement. Early immobilization and evaluation reduce complications. (Mayo Clinic, 2024; UT Southwestern Medical Center, n.d.). Mayo Clinic+1
How Doctors Evaluate Spine Injuries
Step 1: History and exam
Clinicians review the mechanism of injury (rear-end crash vs. fall, speed, seatbelt/helmet use) and perform neurologic testing of strength, reflexes, sensation, and balance. (UT Southwestern Medical Center, n.d.). UT Southwestern Medical Center
Step 2: Imaging
-
X-rays can show alignment and fractures.
-
CT defines bone injury well, especially after high-energy trauma.
-
MRI scans show the discs, ligaments, spinal cord, and nerve roots.
Emergency teams immobilize the spine and select imaging based on risk and symptoms. (UT Southwestern Medical Center, n.d.; Mayo Clinic, 2024; Alaska Department of Health, 2023). UT Southwestern Medical Center+1
Step 3: Special vascular imaging when indicated
If risk factors for BCVI are present (e.g., high-energy mechanism, cervical fractures, neurological deficits not explained by brain imaging), clinicians may order CT angiography to check carotid/vertebral arteries. (Brommeland et al., 2018). PubMed
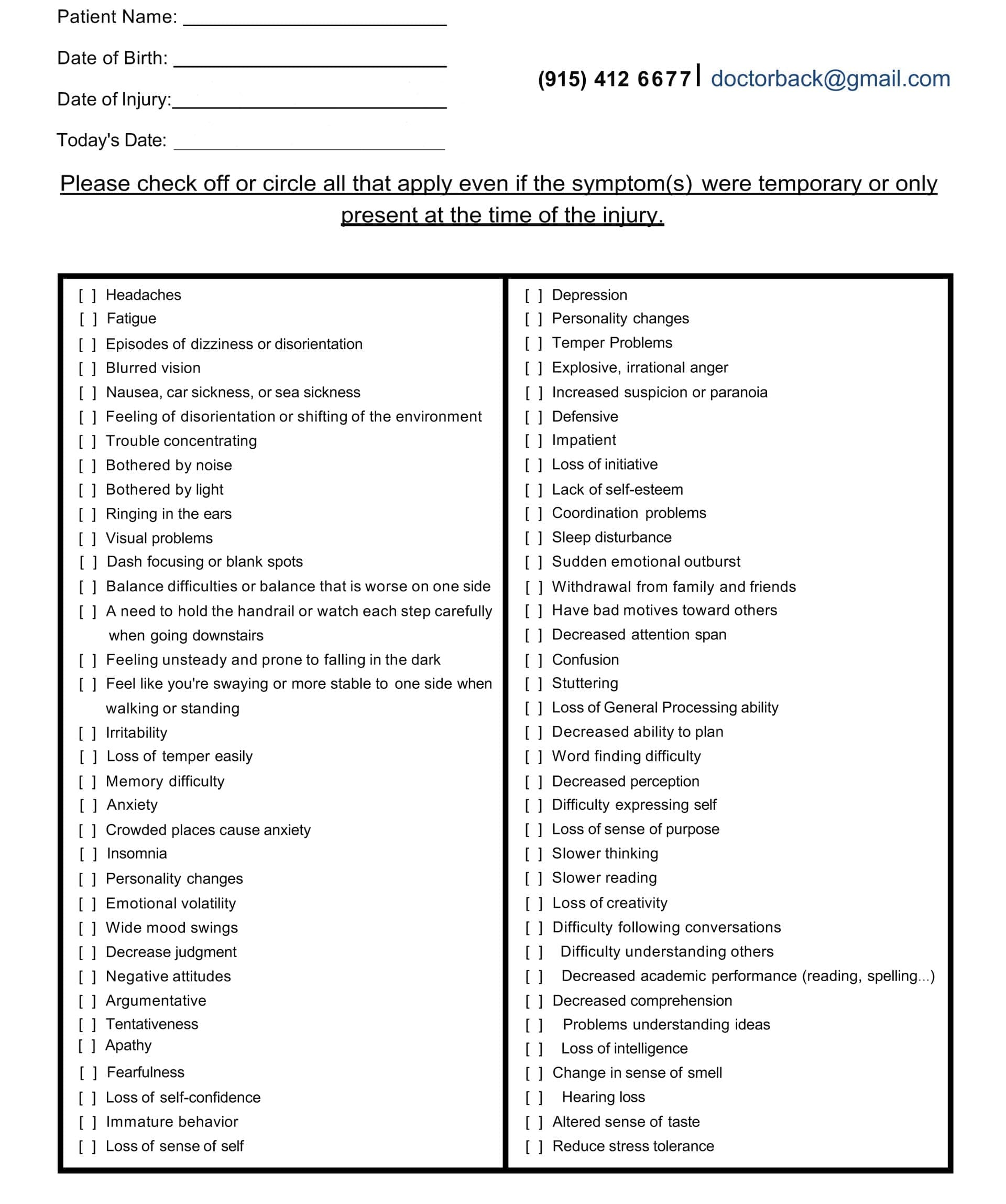
Head Injury/TBI Symptom Questionnaire:
Medical Treatment Pathways (Acute to Rehab)
At the scene and ER: Emergency teams stabilize the head and neck, protect breathing and circulation, and prevent secondary damage. Surgery may be needed to decompress the cord or stabilize unstable fractures. (Mayo Clinic, 2024; UT Southwestern Medical Center, n.d.). Mayo Clinic+1
Inpatient and early rehabilitation: As swelling settles, teams begin mobility, strength, and daily function training to restore independence and prevent complications such as clots or pressure ulcers. (Mayo Clinic, 2024; UT Southwestern Medical Center, n.d.). Mayo Clinic+1
Vascular injury care: When BCVI is diagnosed, early antithrombotic therapy is typically recommended (if safe) with follow-up vascular imaging. (Brommeland et al., 2018; Stone et al., 2018). PubMed+1
Where Integrative Chiropractic Care Fits
Integrative chiropractic care emphasizes non-invasive methods to alleviate pain, enhance joint mobility, restore muscle balance, and promote optimal posture and function. It is not a replacement for emergency medicine or surgery; serious injuries must be evaluated medically first. In many cases, chiropractic care works in conjunction with primary care, neurology, neurosurgery, and physical medicine/rehab. (The Neck and Back Clinics, n.d.; Function First Indy, n.d.). The Neck and Back Clinics+1
Potential roles after medical clearance:
-
Gentle, evidence-informed spinal manipulation or mobilization for mechanical neck/back pain and stiffness that linger after soft-tissue injury.
-
Active rehab: graded exercises for mobility, strength, and posture; movement retraining to protect the spine during daily tasks and sports.
-
Ergonomic and activity advice for work and life.
-
Team communication: sharing exam findings and progress notes with your medical team.
Community clinics and educational sources describe how chiropractic care can help reduce pain and stiffness related to auto/work injuries and how care plans can include soft-tissue methods and home exercises to support function and return to activity. (The Neck and Back Clinics, n.d.; Dr. Kal, n.d.; Sea Change Chiropractic, n.d.; NWHSU/Chiropractic Economics feature, 2023; Dominguez Injury Centers, n.d.). NICHD+4The Neck and Back Clinics+4Northwestern Health Sciences University+4
Important safety note: If you have red-flag symptoms (progressive weakness, numbness in a limb, bowel/bladder changes, fever with back pain, or suspected fracture), seek medical care first. Manipulation is not appropriate for unstable fractures, acute cord compression, or a fresh post-op spine—those are medical/surgical domains. (Mayo Clinic, 2024). Mayo Clinic
Special Considerations: Head Injury + Neck Injury Together
When concussion/TBI signs are present—headache, dizziness, fogginess, balance changes—your care team should screen both brain and cervical spine. Pediatric data show that cervical issues can coexist with TBI and alter outcomes, underscoring the need for cautious, age-appropriate imaging and clearance. (Weiss & Anderson, 2024). MDPI
Clinics sometimes discuss how post-crash chiropractic care may support neck-related headaches, stiffness, and posture, while your medical team addresses brain injury recovery and vestibular/oculomotor rehab when needed. This is an integrative, not either-or, model. (The Neck and Back Clinics, n.d.; NWHSU/Chiropractic Economics feature, 2023). The Neck and Back Clinics+1
Practical Recovery Phases (Simplified)
-
Emergency & diagnostics: rule out fracture, dislocation, SCI, and BCVI; protect the spine; image as needed. (UT Southwestern Medical Center, n.d.; Mayo Clinic, 2024; Brommeland et al., 2018). UT Southwestern Medical Center+2Mayo Clinic+2
-
Acute symptom control: pain relief, inflammation control, bracing if ordered, and gentle motion when safe. (Mayo Clinic, 2024). Mayo Clinic
-
Rehab: restore mobility, strength, and endurance; address balance and gait; retrain posture and body mechanics. (UT Southwestern Medical Center, n.d.). UT Southwestern Medical Center
-
Return to work/sport planning: graded loading, task-specific drills, protective gear, and workplace or ergonomic changes. (UT Southwestern Medical Center, n.d.). UT Southwestern Medical Center
-
Maintenance & prevention: sustained exercise, sleep, nutrition, and periodic reassessment for flare-ups. (General rehab principles). Mayo Clinic
Prevention Tips You Can Start Today
-
Seatbelts for every ride and the correct headrest height.
-
Helmets for biking, skating, skiing, football, and motorcycling.
-
No diving into shallow or unknown water.
-
Declutter walkways, add rails, and wear grip shoes to prevent falls. (UT Southwestern Medical Center, n.d.). UT Southwestern Medical Center
Clinical Observations from Dr. Alexander Jimenez, DC, APRN, FNP-BC
In a dual-scope, integrative clinic, Dr. Jimenez emphasizes:
-
Careful history of mechanism (rear-end vs. rollover vs. fall) to predict the likely injury pattern and guide imaging referrals.
-
Early team communication with primary care, neurology, neurosurgery, physiatry, and physical therapy when red flags appear.
-
A staged plan that begins with pain-modulating, low-risk methods (gentle mobilization, soft-tissue work, and graded movement) once serious conditions are ruled out.
-
Active rehabilitation (mobility + strength + balance), plus ergonomic and return-to-activity coaching to lower re-injury risk. (Dr. Alex Jimenez — clinical practice portal). El Paso, TX Doctor Of Chiropractic
Bottom Line
After a crash, fall, sports injury, or work-related injury, your spine absorbs complex forces that can injure soft tissues, joints, discs, bones, and—at the most severe end—the spinal cord or neck arteries. Rapid medical triage and imaging protect you from complications. Once dangerous problems are ruled out or treated, integrative chiropractic care can be a non-invasive part of a team plan to reduce pain, improve motion, and build long-term resilience.
References
Brommeland, T., Helseth, E., Aarhus, M., Moen, K. G., & Dyrskog, S. (2018). Best practice guidelines for blunt cerebrovascular injury. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. https://doi.org/10.1186/s13049-018-0559-1 PubMed
Casper & de Toledo, LLC. (n.d.). How a rear-end collision can impact your spine and brain. https://www.casperdetoledo.com/how-a-rear-end-collision-can-impact-your-spine-and-brain/
DrKal Chiropractic. (n.d.). Chiropractic care for accident victims: The science. https://drkal.com/chiropractic-care-for-accident-victims-the-science/ Northwestern Health Sciences University
Dominguez Injury Centers. (n.d.). How chiropractic care supports effective injury healing. https://www.dominguezinjurycenters.com/how-chiropractic-care-supports-effective-injury-healing/ NICHD
Mayo Clinic Staff. (2024, August 17). Spinal cord injury: Diagnosis & treatment. https://www.mayoclinic.org/diseases-conditions/spinal-cord-injury/diagnosis-treatment/drc-20377895 Mayo Clinic
Northwestern Health Sciences University. (2023). Reis writes for Chiropractic Economics: Chiropractic and traumatic brain injuries. https://www.nwhealth.edu/news/reis-writes-for-chiropractic-economics-chiropractic-and-traumatic-brain-injuries/ Northwestern Health Sciences University
Physio-Pedia. (n.d.). Sports injuries of the head and neck. https://www.physio-pedia.com/Sports_Injuries_of_the_Head_and_Neck Brain and Spinal Cord
Sea Change Chiropractic. (n.d.). How chiropractic helps reset the nervous system after car crash trauma. https://seachangechiropractic.com/how-chiropractic-helps-reset-the-nervous-system-after-car-crash-trauma/ seachangechiropractic.com
Stone, D. K., Viswanathan, V. T., & Wilson, C. A. (2018). Management of blunt cerebrovascular injury. Current Neurology and Neuroscience Reports. https://pubmed.ncbi.nlm.nih.gov/30353308/ PubMed
The Neck and Back Clinics. (n.d.). How chiropractic care may alleviate neck and back pain from auto and work-related accidents. https://theneckandbackclinics.com/how-chiropractic-care-may-alleviate-neck-and-back-pain-from-auto-and-work-related-accidents/ The Neck and Back Clinics
UT Southwestern Medical Center. (n.d.). Spinal cord injury—Peter O’Donnell Jr. Brain Institute. https://utswmed.org/conditions-treatments/spinal-cord-injury/ UT Southwestern Medical Center
van den Hauwe, L., Sundgren, P. C., & Flanders, A. E. (2020). Spinal trauma and spinal cord injury (SCI). In Diseases of the Brain, Head and Neck, Spine 2020–2023: Diagnostic Imaging (NCBI Bookshelf). https://www.ncbi.nlm.nih.gov/books/NBK554330/ NCBI
Weill Cornell Medicine Neurological Surgery. (n.d.). About brain and spine injuries. https://neurosurgery.weillcornell.org/service/brain-and-spine-injury/about-brain-and-spine-injuries Weill Cornell Neurosurgery
Weiss, H. K., & Anderson, R. C. E. (2024). Challenges and insights: Cervical spine injuries in children with traumatic brain injury. Children, 11(7), 809. https://www.mdpi.com/2227-9067/11/7/809 MDPI
Additional supportive sources referenced for soft-tissue and patient-facing education:
Brain and Spinal Cord. (n.d.). Motor vehicle accident overview. https://brainandspinalcord.org/motor-vehicle-accident/ Northwest Florida Physicians Group
Function First Indy. (n.d.). The role of chiropractic care in personal injury recovery. https://www.functionfirstindy.com/the-role-of-chiropractic-care-in-personal-injury-recovery functionfirstindy.com
Dr. Alex Jimenez. (n.d.). El Paso’s Premier Chiropractic Clinic—Integrative injury and spine care. https://dralexjimenez.com/ El Paso, TX Doctor Of Chiropractic
Alaska Department of Health. (2023). Stabilization and interfacility management of spinal cord injuries (clinical guide). https://health.alaska.gov/media/hvunl5ji/stabilization-and-interfacility-management-of-spinal-cord-injuries.pdf
Post Disclaimer
Professional Scope of Practice *
The information herein on "Spine Risks in High Impact Accidents: What to Know" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.