Surgery options when back pain is becoming chronic or so severe that an individual cannot function normally and negatively affects their life. Pretty much everyone experiences back pain at some point. This is often from:
- Lifting heavy/non-heavy objects incorrectly
- Improper posture
- Twisting in an awkward way
- Overreaching
- Muscle spasms
- Physical activity the body is not used to doing
Most cases of backaches and pain go away by themselves or with conservative treatment. But sometimes, surgery is necessary.
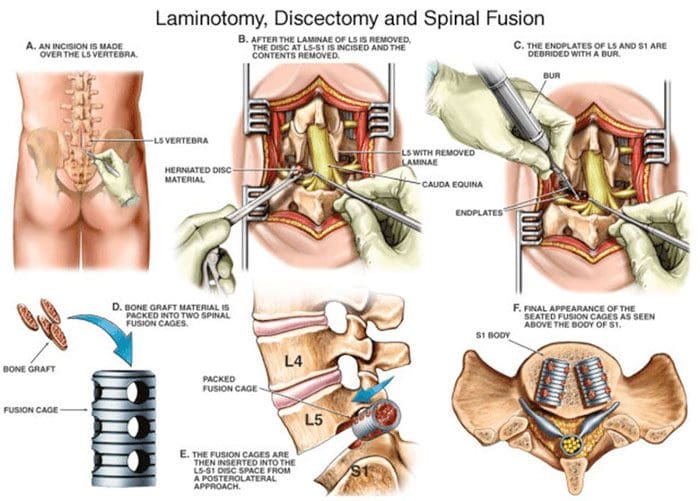
Table of Contents
When Surgery Is Necessary
Acute back pain can last for days or weeks and can often resolve with physical therapy, chiropractic, and self-care. Back pain that continues for 12 weeks or longer is considered chronic. Around twenty percent of individuals who experience acute low back pain after a year begin developing chronic back pain. Doctors try to treat most back pain cases with non-surgical approaches.
- They usually begin with physical therapy/chiropractic.
- If that doesn’t work, then medication is incorporated.
- However, many individuals do not want to take long-term medication, which is when surgery may be recommended.
- In most cases, surgery is a last resort.
When the pain radiates to the legs or if it is causing problems with bladder and/or bowel function, these are definite signs/symptoms that surgery is needed. If the pain/dysfunction continues after thorough and effective non-surgical treatment, surgery could be recommended to preserve the spine to improve spinal strength and function before the problem worsens, causing further injury and damage. Some of the most common and effective spine surgery options include.
Surgery Options
Microdiscectomy
Microdiscectomy is the most common back surgery in the United States. It is minimally invasive spine surgery. Microdiscectomy patients have low back pain combined with leg pain, tingling, numbness, and weakness. In between the vertebrae are the body’s shock-absorbing discs. The discs can begin to bulge out, a bulging or herniated disc, and press on the surrounding nerve roots, causing pain, tingling, numbness, or weakness. A microdiscectomy removes the portions of the disc pressing on the nerve.
It is called micro because the surgeon wears specialized glasses known as loupes that act as microscopes. This is so the surgeon can see the details when they’re operating. The surgery is performed through a small incision in the middle of the back or on the affected side. Patients can go home a few hours after the surgery and return to normal activities within two weeks. The success rate is 85 – 95%, especially if the surgery is done early before the damage begins to spread out.
Laminectomy
The spinal canal contains a special lining. This is where the nerves and ligaments run through. Age, along with normal wear and tear on the body, causes the ligaments to thicken. This is when bone spurs can develop from osteoarthritis, and the discs can begin to bulge or rupture/herniate. This clogs and impinges the space where the nerves should easily flow through. This narrowing is called spinal stenosis. A laminectomy opens up the space relieving the compression/pressure. The procedure requires removing part of the back of a vertebra called the lamina. This enlarges the spinal canal and relieves the pressure on the nerves. The procedure is done through a small incision in the middle of the back but can also be done through a minimal incision. Leg pain improves after surgery. A traditional incision full recovery takes 6 to 12 weeks. The success rate is around 85 percent.
Spinal Fusion
A spinal fusion joins/fuses two or more bones in the spine. This is done when an individual has severe compression of the nerves, severe instability, or spinal revision surgery. A fusion can help stabilize spinal fractures. Other reasons for a spinal fusion are spine deformity, cancer of the spine, and sometimes used for intractable pain. A fusion stabilizes the spine with screws and rods. The disc causing the compression is replaced with a fusion device and bone graft. The surgery is often performed in combination with a laminectomy. Recovery and returning to activities can take around 3-4 months after the procedure. The success rate is 85-90% with pain improvement.
Kyphoplasty
Spinal compression fractures are common in individuals with osteoporosis. When they happen, the pain can be so intense that braces and medication don’t help. Kyphoplasty can bring pain relief. It can be performed by a pain management doctor, interventional radiologist, or surgeon in an outpatient X-ray facility and operating room. The procedure involves conscious sedation, sometimes accompanied by general anesthesia. A small instrument is inserted into the vertebra, and a balloon is inflated to make room for bone cement. After the bone cement is injected, patients can go home within a few hours. The success rate is around 85%, and recovery time could be several days.
Disc Replacement
This is a procedure that can replace spinal fusion for certain cases. A disc replacement can be done in the lumbar/low back or the cervical/neck spine. This procedure is performed to treat a pinched nerve and/or spinal cord compression. The injured/damaged disc is removed and is replaced with an artificial disc. The device allows for motion, whereas fusion procedures fuse the bones to stabilize and immobilize the area. Disc replacement is recommended for younger patients that don’t have serious arthritis. This is because they still have mobility. If significant arthritis is present, the patient could experience more pain and require spinal fusion. Recovery takes around six weeks. Intense physical activity is off-limits for two or three weeks after the initial recovery period. The success rate is more than 90%.
Anterior Cervical Discectomy and Fusion – ACDF
This is a common neck/cervical spine procedure. This surgery is for pain relief, weakness, tingling, and numbness of the arms caused by a pinched nerve or stenosis. The damaged disc is removed through a small incision in the side of the front of the neck. The disc is replaced with a bone graft or specialized spacer and a small plate with screws. This is to stabilize the spine. It is highly effective in relieving pain and in preventing neurological decline from spinal cord compression. Recovery time is around 12 weeks before a full return to normal activities. However, individuals report feeling better after two weeks.
Back Surgery Options
The majority of cases involving back pain get better on their own or with conservative treatment. But if an individual cannot find relief, there are safe and effective surgery options that can help.
Body Composition
When The Immune System Activates
When the body gets sick from a bacterial infection, virus, etc., the body’s defense system activates, causing inflammation. This immune response serves as the first wave of defense against foreign invaders. The infected area becomes red and swollen from increased blood flow. For example, when the nose gets red from a cold, this is inflammation. The reaction is caused by white blood cells known as macrophages, and the proteins they emit called cytokines encourage inflammation. Inflammation that’s triggered by the immune system is normally a good thing. It means the body is releasing a proper amount of hormones and proteins. These activate the white blood cells to start the healing process and work to fight the infection.
References
Low Back Pain Fact Sheet. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Low-Back-Pain-Fact-Sheet
A review of complication rates for Anterior Cervical Diskectomy and Fusion (ACDF). Surg Neurol Int. 2019. https://pubmed.ncbi.nlm.nih.gov/31528438/
Rheumatology Advisor. (2017.) “Back Pain.†https://www.rheumatologyadvisor.com/home/decision-support-in-medicine/rheumatology/back-pain/
Post Disclaimer
Professional Scope of Practice *
The information herein on "Spinal Surgery Options" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.