Table of Contents
Summary
- Neoplasms
- The vast majority of clinically suspected bone Mets are found in the axial skeleton and proximal femurs/humeri
- Radiography is the most cost-effective and readily available initial imaging tool to investigate bone Mets but often fails early metastatic detection
- Tc99 bone scintigraphy is the most sensitive and cost-effective imaging modality to demonstrate metastatic foci
- MR imaging may help regional identification of bone Mets especially if x-radiography is unrewarding
- Significant limitations of MRI: inability to perform a whole-body MRI scan
- Cost and other contraindications such as cardiac pacemakers and cochlear implants may be another limiting factor
Marrow Based Neoplasms
- Malignancy originating from the marrow cells are often referred to as “round-cell tumors.”
- Multiple Myeloma (MM)
- Lymphoma
- Ewing’s sarcoma
- The last two are less frequent than MM
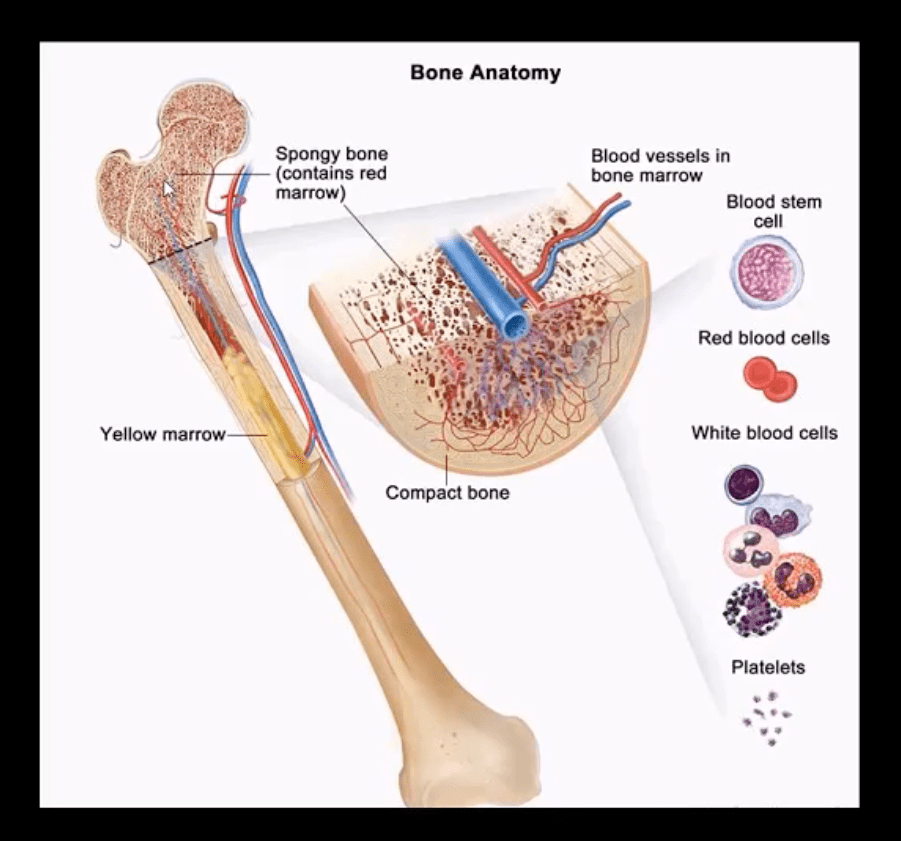
- Red marrow in adults is in the axial skeleton and proximal femurs/humeri d/t gradual marrow “retraction” following the childhood
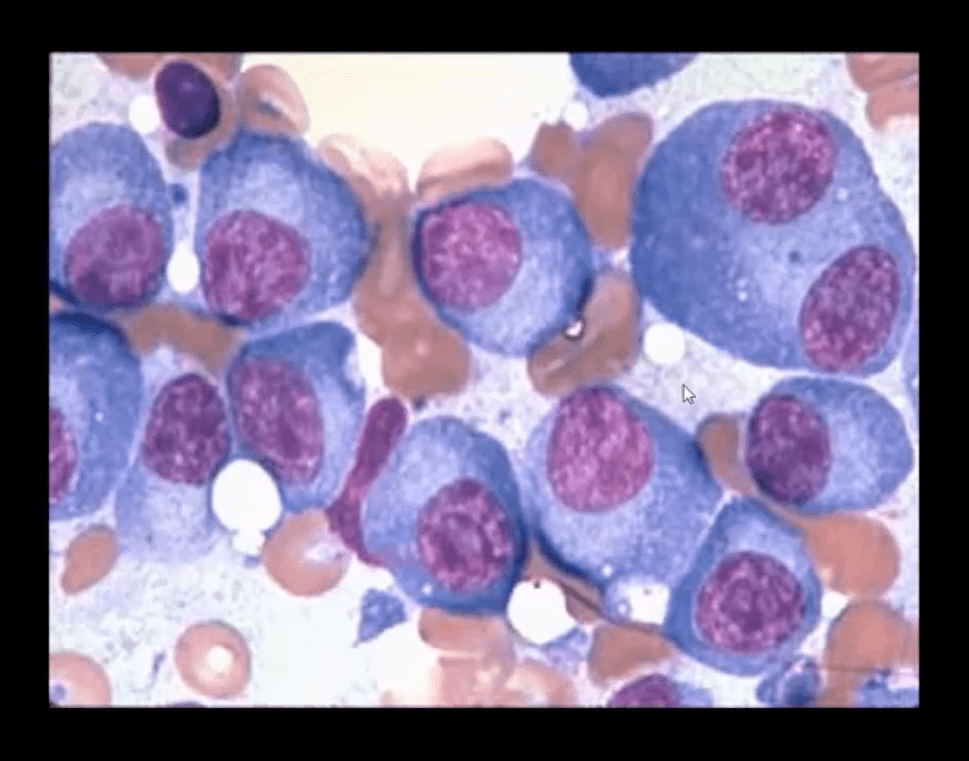
- Note bone marrow biopsy histopathology specimen of MM with abnormal plasma cells replacing regular marrow residents (above image)
- Multiple Myeloma (MM) is the most common primary bone neoplasm in adults>40s. Etiology is unknown, but many theories exist (e.g., genetic, environmental, radiation, chronic inflammation, MGUS)
- MM: malignant proliferation of plasma cells >10% of red marrow, with subsequent replacement of normal marrow cells by myeloma cells and overproduction of monoclonal antibodies paraproteins (M protein) with heavy chains IgG (52%), IgA (21%), IgM (12%) and light chains kappa or lambda aka Bence-Jones proteins
Clinical Presentation of MM
- MM is occasionally detected as unexplained anemia on routine blood studies for unrelated complaints
- Common MSK symptoms: Bone pain/Pathologic fractures
- Constitutional: Weakness/malaise
- Systemic: bleeding, anemia, Infection (especially pneumococcal) d/t marrow replacement and pancytopenia
- Hypercalcemia d/t bone resorption
- Renal failure aka myeloma kidney
- Neuropathies
- Amyloidosis
- Gout
- Diagnostic imaging plays an essential role during the Dx of MM
- Bone marrow aspiration biopsy, blood tests, and serum protein electrophoresis may be usedÂ
- Imaging approach: bone pain is investigated with initial x-radiographs if radiographs are unrewarding MR imaging may help to reveal bone marrow abnormality. MRI is recommended as myeloma survey
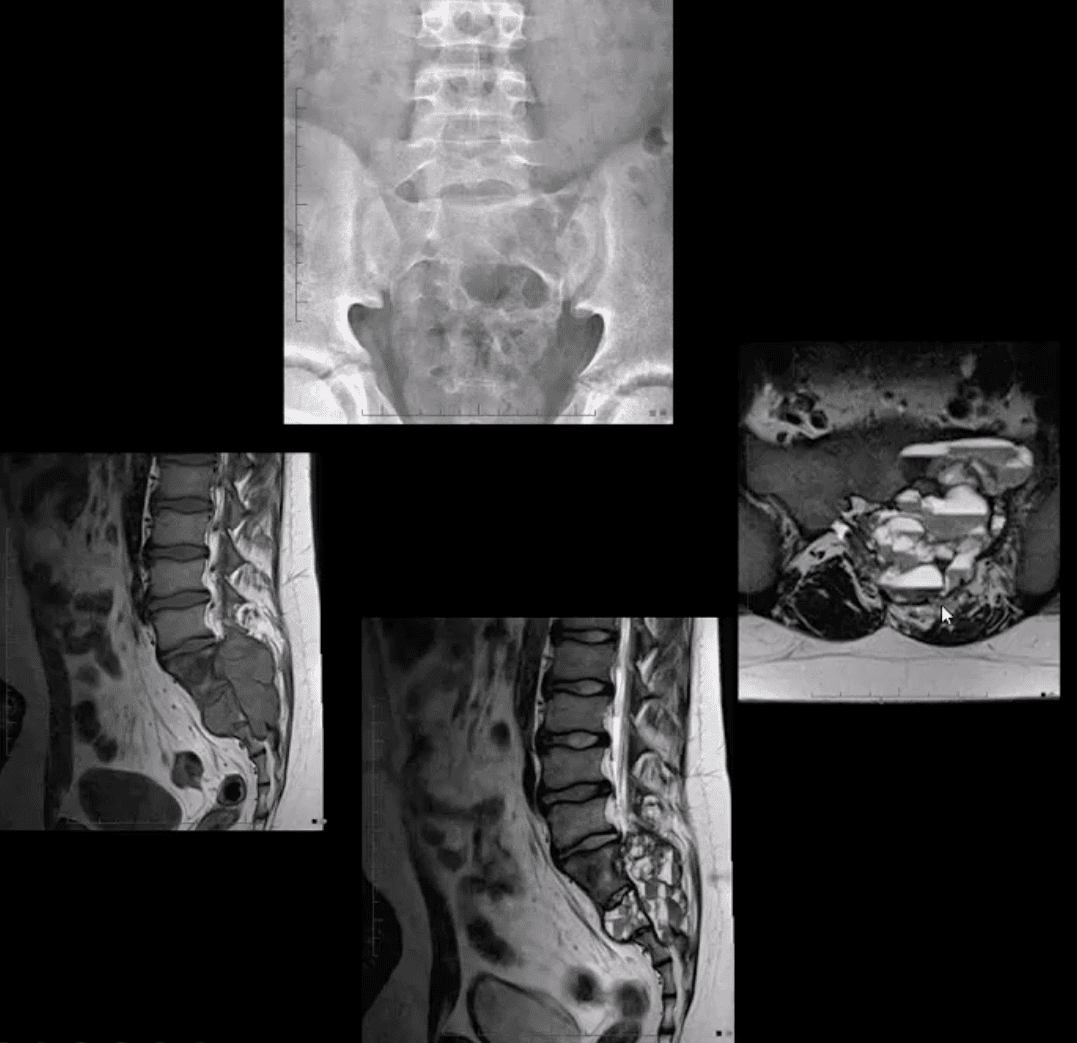
- Currently, MRI protocol known as “whole body myeloma scan” consisting of T1, T2-fat suppressed, and T1+C coronal sequences can detect MM in the skull, spine, pelvis, ribs and femurs/humeri. This technique is much more superior to radiographic “skeletal myeloma survey.”
- Tc99 bone scintigraphy is not typically used for MM because over 30% of MM lesions are “cold” or photopenic on radionuclide bone scan d/t highly lytic nature of MM with osteoclasts outpacing osteoblasts.
- A radiographic skeletal survey is considered more sensitive than bone scintigraphy in MM
- PET-CT scanning of MM is gaining popularity due to the high level of detection of multiple sites of MM

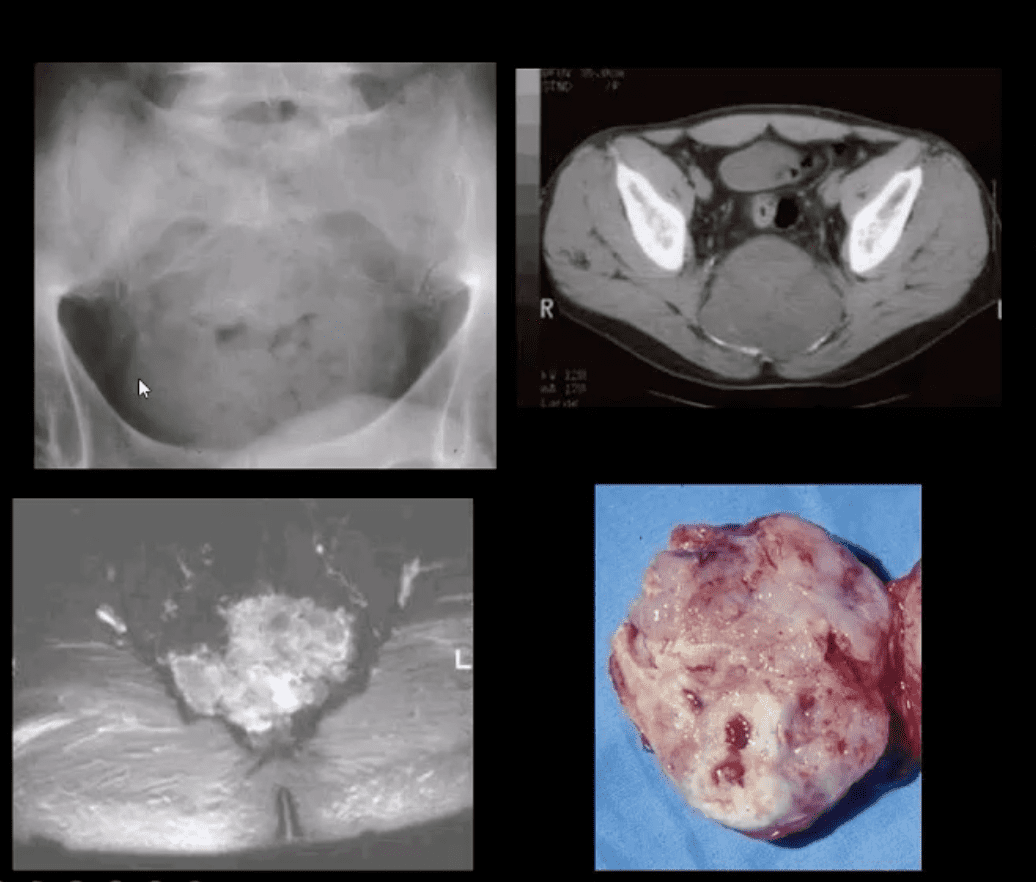
- Radiographic Dx of MM: consists of identification of characteristically localized focal osteolytic “punched out” or “moth-eaten” lesions of variable sizes following the distribution of adults red marrow
- Note rad abnormality is known as “raindrop skull” is characteristic of MM

- Radiographic appearance of MM may vary from “punched out” round radiolucencies to “moth-eaten” or permeating osteolytic lesion producing endosteal scalloping (yellow arrow)
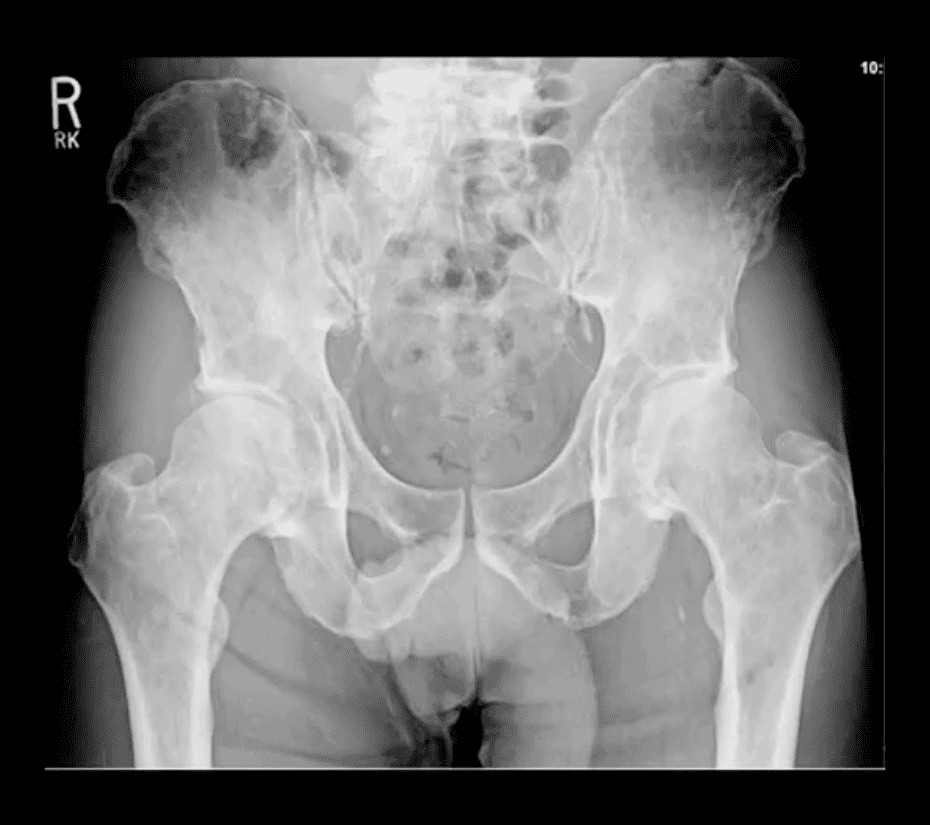
- Pelvis and femurs are commonly affected by MM and present radiographically as round lytic punched out or moth-eaten lesions
- N.B. Occasionally MM may pose radiographic dilemma by presenting as generalized osteopenia in the spine that can be difficult to differentiate from age-related osteoporosis
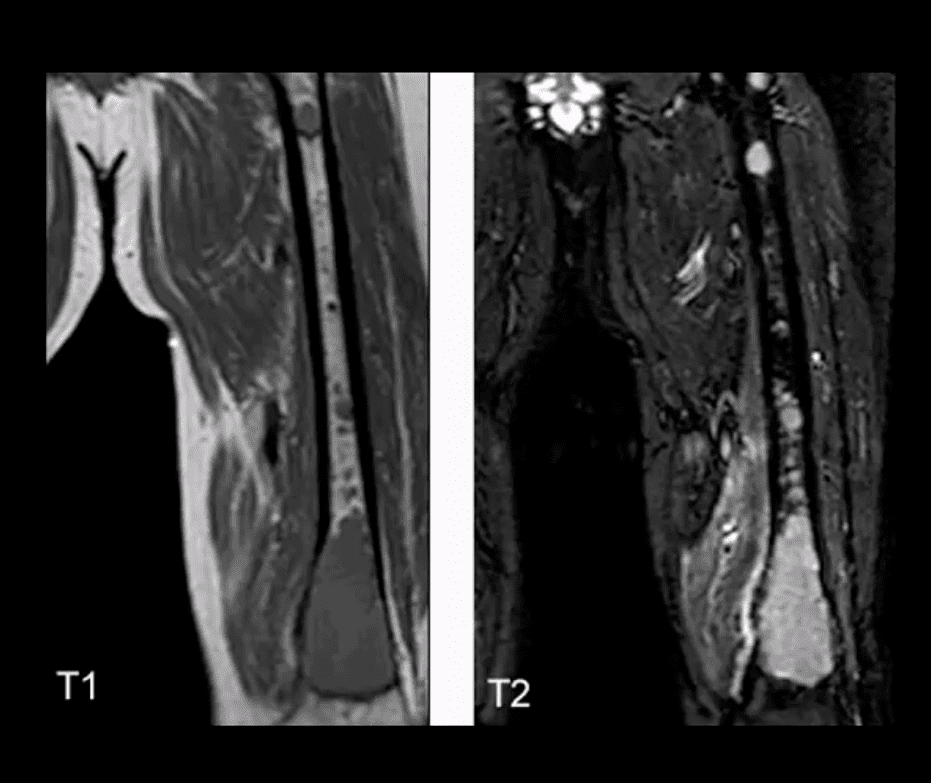
- MR imaging of MM reveals marrow changes with low signal on T1, a high signal on fluid-sensitive sequences and bright contrast enhancement on T1+C gad d/t increased vasculature and high activity of MM cells

- Example of full-body MRI of “whole body myeloma scan” with T2-fat suppressed (A), T1 (B) and T1+C (C) pulse sequences produced in coronal slices
- Note multiple foci of bone marrow changes in the spine pelvis and femurs
Miscellaneous Neoplasms of the Spinal Column
- Chordoma: is relatively uncommon but considered the m/c primary malignant neoplasm that only affects the spine. D/t slow growth is often misdiagnosed for a considerable length of time as LBP
- Pathology: derives from malignant transformation of notochordal cells presented as mucoid, gelatinous mass containing physaliphorous cells
- Demo:Â M: F 3:1 (30-70S). 50%-sacrococcygeal, 35% spheno-occipital 15%-spine
- Clinically: asymptomatic for a long time until non-specific LBP, changes in bladder & bowel, neurological signs are less common d/t midline “outward” growth & inferior to S1. Local invasion worsens prognosis. 60%-survive 5-years, 40%-10-years, Mets are delayed, poor prognosis d/t local invasion. >50% can be id. on DRE.
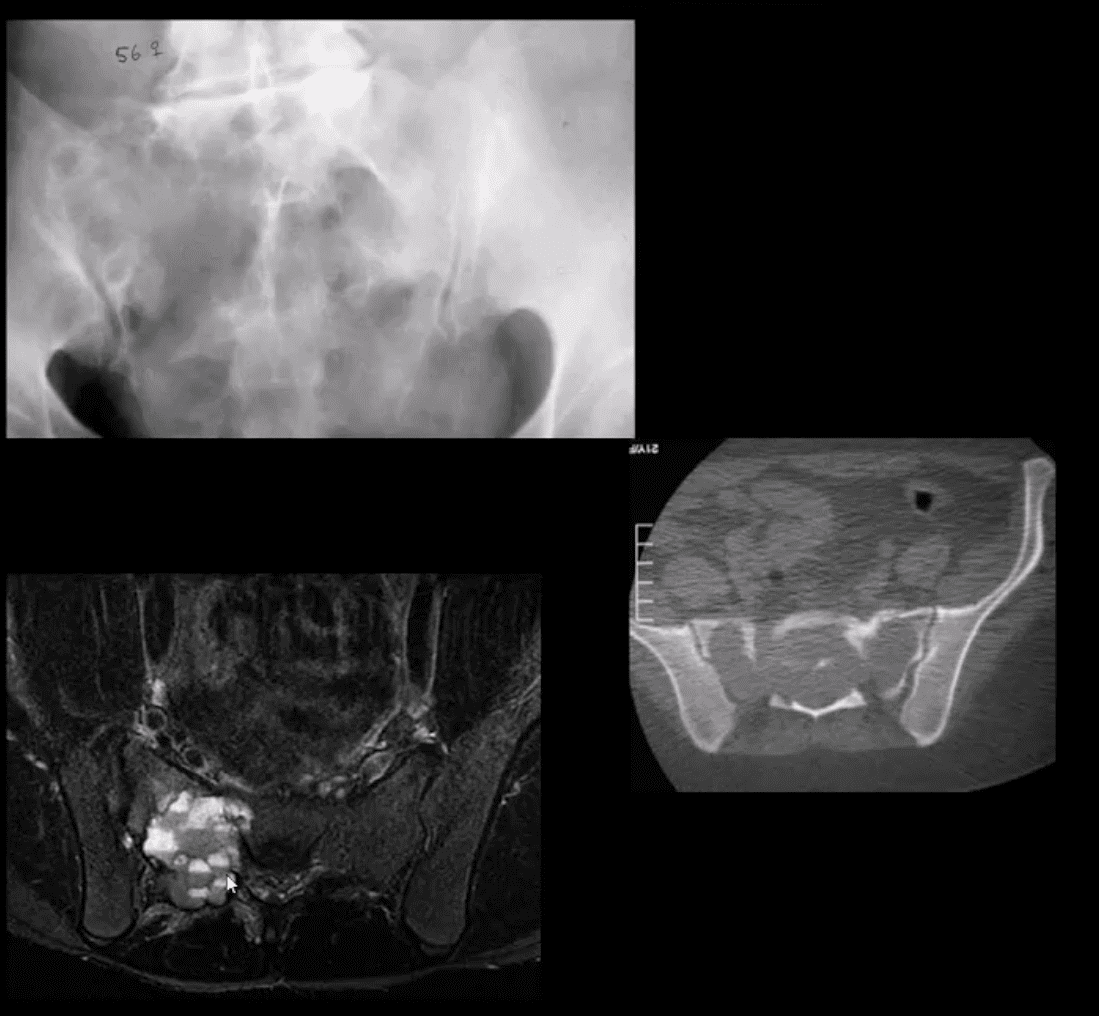
- Imaging:Â x-rays often tricky d/t overlying gas/feces. CT is >sensitive to id the bone mass and internal calcifications. MRI: T2 bight signal, T1 heterogeneously low and high d/t mucus/blood decomposition, MRI best detects local invasion and essential for care planning. Rx:Â complete excision is often impossible d/t local vascular invasion.
- Giant cell tumor (GCT):Â 2nd most common primary sacral tumor. It is a histolgically benign neoplasm containing multinucleated Giant cells of Monocyte-Osteoclast origin
- Imaging Dx:Â x-radiography is the 1st step usually in response to complaints of LBP. Often challenging to id on x-rays d/t bowel gas/feces
- Key rad feature: osteolytic expansile lesion noted by destruction of sacral arcuate lines. CT may id the lesion better. MRI is the modality of choice folowing x-rays. MRI: T1 low to intermediate signal. Heterogenously high d/t edema with areas of low signal on T2 d/t blood degradation and fibrosis. Characteristic fluid-fluid levels may be noted especially if ABC develops within a GCT. Rx: operative. Prognosis is less favorable than GCT in long bones d/t lung Mets (deposits) in 13.7%
- Aneurysmal Bone Cysts (ABC) are benign expansile tumor-like bone lesions (not a true neoplasm) composed and filled with numerous blood-filled channels. Thus the term “blood sponge.” ABC is m/c id in children and adolescents
- Unknown etiology: trauma and pre-existing bone neoplasm (e.g., GCT) often reported. Clinically: pain that may be progressive d/t rapid nature of ABC expansion. In the spine, ABC m/c affects posterior elements and presented as expansile, soap-bubbly or lytic lesion.
- DDx: can be broad, but Osteoblastoma and GCT are the top DDxs.
- Imaging: x-rays demo expansile mass in posterior elements, CT is more sensitive than x-rays, MRI will demo characteristic fluid-fluid levels and mixed high and low signal d/t edema and blood decomposition/aging with some septations.
- N.B. MRI fluid-fluid levels are not exclusive to ABC, and DDx includes
GCT, osteoblastoma, telangiectatic osteosarcoma. - Rx: operative curettage and bone grafting, fibrosing agents. Recurrence 10-30%.
Spinal Neoplasms
Additional Resources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4931792/
- https://emedicine.medscape.com/article/1267223-overview#a4
- https://www.ncbi.nim.nih.gov/pmc/articles/PMC2958273/
- http://bonetumor.org/
Post Disclaimer
Professional Scope of Practice *
The information herein on "Spinal Neoplasms Diagnostic Imaging Approach Part II" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card




 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.