Metastatic Bone Disease (aka Mets) or “Secondaries.” Are the most common malignant bone neoplasms affecting the spine, aka spinal neoplasms (>70%) and the rest of the skeleton in adults.
- 5-Primaries are m/c involved:
- Breast (16-37%)
- Lung (12-15%)
- Thyroid (4%)
- Renal (3-6%)
- Prostate (9-15%)
- Spine, pelvis, proximal femurs & proximal humeri are m/c affected in that particular order of frequency
- Thoracic & upper Lumbar spine considered the m/c site of spinal Mets
Table of Contents
Pathophysiology & Etiology of Metastasis
- Malignant cells a very good at evading immune detection and elimination
- They gain access to circulation expressing Vascular Endothelial Adhesion Molecules (e.g., integrines & selectins)
- Once reaching their target organs, malignant cells stimulate the production of various vasogenic growth factors and by exiting blood vessels invade their target tissues
- Lung, Liver, and Bone are particularly at risk due to the character of their blood supply
- Baston venous plexus-is a network of valveless freely communicating veins connecting axial skeleton/meninges and proximal femurs/humeri with abdomino-pelvic and thoracic cavities
- The risk of Mets is increased during daily variations in the intra-abdominal and intra-thoracic pressure
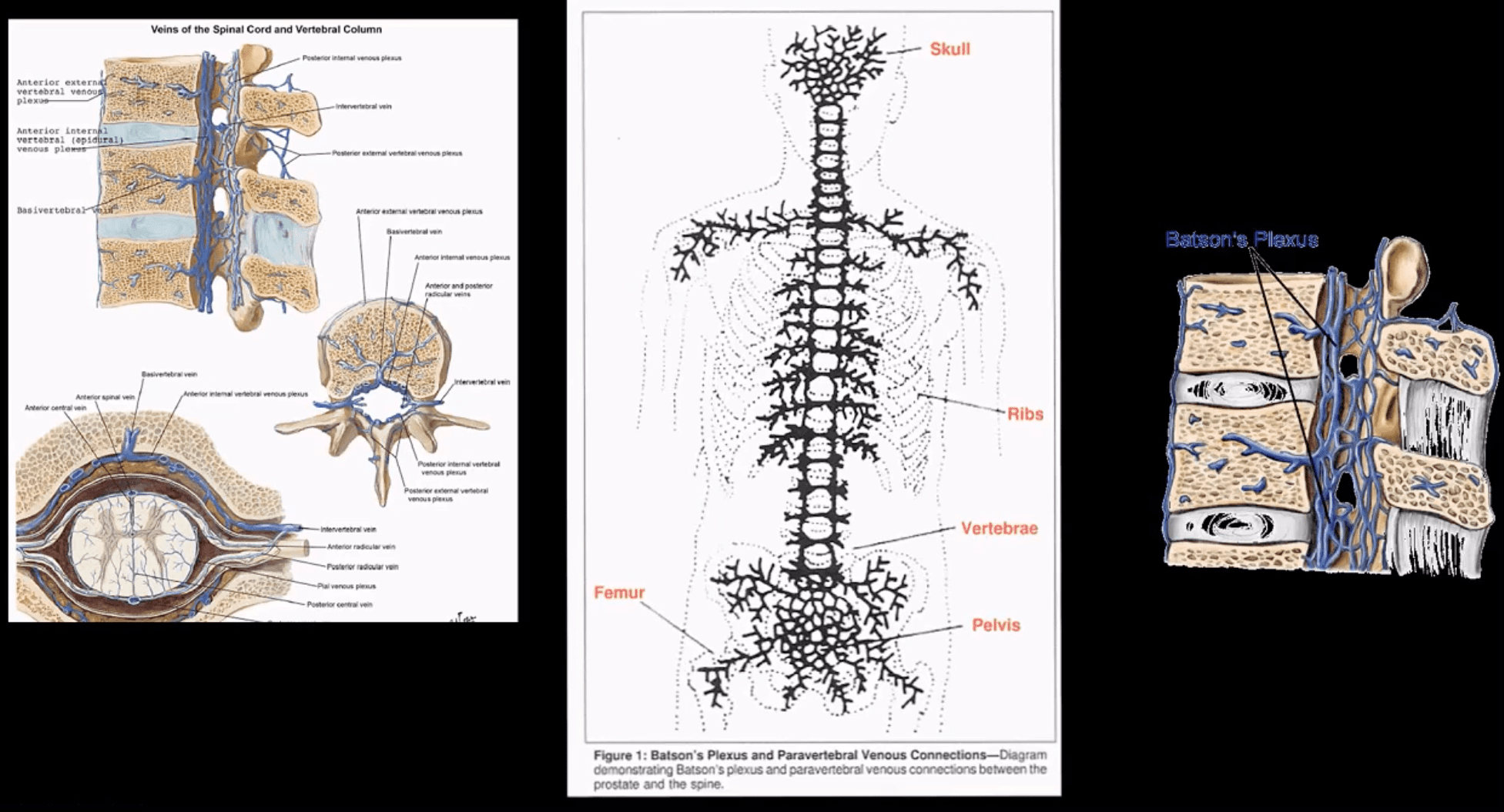
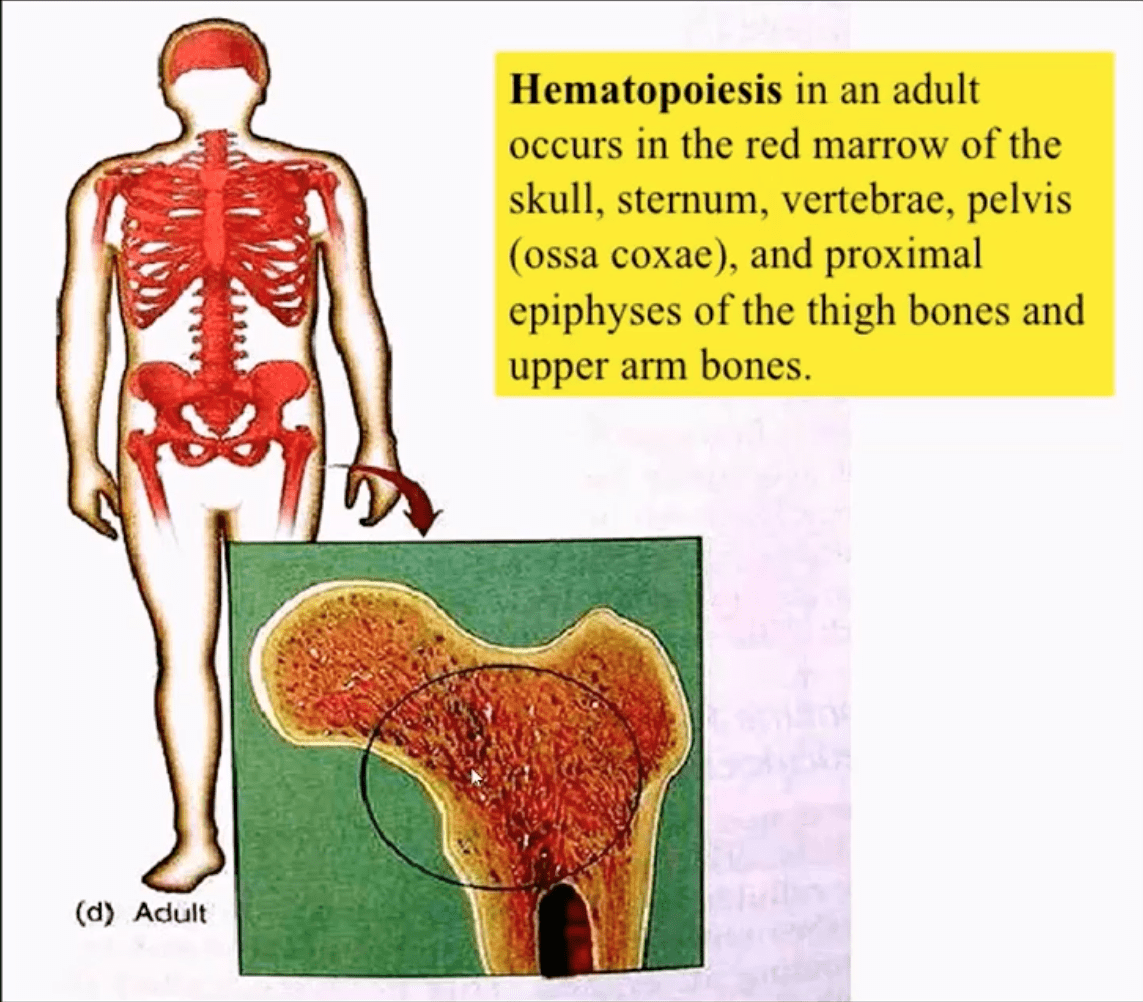
- In adults, the axial skeleton is involved in hematopoiesis, and it is particularly vulnerable to metastatic deposits via an abundant network of sinusoids within a spongy bone
- The vast majority of bone Mets will be detected in the axial skeleton
Clinical Presentation
- Back pain often mimicking “mechanical back pain” is the m/c and often misleading symptom
- Chiropractors and other manipulators should be particularly aware of this dangerous pitfall.
- Nocturnal pain or pain unresponsive to NSAID may be reported in more advanced cases
- Advanced cases may also present with a neurological deficit due to pathologic vertebral fractures and spinal cord/nerves compression
- Metastatic hypercalcemia may occasionally develop in severe cases and considered a medical emergency that potentially presents with confusion, muscle weakness, and renal signs
- Imaging plays a significant role in the Dx and management of bone metastasis
- Lab tests are of limited value, but hypercalcemia and alkaline phosphatase (Alk Phos) may be elevated
- In some cases, a bone biopsy may be used to confirm bone Mets
When Bone Mets are Detected, Patients Prognosis is Significantly Worsened
- Median survival:
- Thyroid – 48 – months
- Prostate – 40 – months
- Breast – 24 – months
- Renal Cell – may vary, can be as low as 6 – months
- Lung – 6 – months
Imaging Diagnosis
- Begins with radiography investigating a clinical complaint of back/bone pain
- If radiographs are unrewarding or equivocal, unique imaging modalities are required
- MRI may help to show marrow replacement by Mets foci but limited to specific regions
- Tc99 radionuclide bone scan (scintigraphy) is considered one of the most sensitive and reliable imaging steps in evaluating bone Mets
- Bone scintigraphy is good at detecting both lytic and blastic Mets
- However, very aggressive/vascular osteolytic Mets and Multiple Myeloma often appear “cold” or photopenic on bone scan due to greater stimulation/activation of osteoclasts which “outpace” osteoblasts ability to uptake the radiopharmaceutical
- CT scanning is an excellent modality to show bone destruction, but it is not widely used during bone Mets Dx especially if radiography, bone scintigraphy, and MRI provide adequate information about the process
- CT scanning may be particularly helpful with delineation of pathological fractures
General Radiographic Features of Bone Mets
- Osteolytic (lytic), osteoblastic (blastic) aka sclerotic Mets or misec Mets can be identified radiographicallyÂ
- However, it takes between 30-50% of lamella (cortical) bone and 50-75% of trabecular (cancellous) or spongy bone to be destroyed before it can be detected on plain film radiographs
- This can make early radiographic detection of bone Mets very difficult, requiring particular imaging modalities (e.g., MRI)
- Also, bowel gas/fecal matter and numerous soft tissue densities in the abdomino-pelvic and thoracic cavities may pose challenges of bone Mets detection
- Different tumors often manifest with different metastatic appearance, depending on tumor activity and release of cytokines (IL6, IL11), endothelin 1 or other growth factors that will be responsible for either osteolytic, osteoblastic or mixed Mets
- For example: purely lytic bone Mets are noted in Lung, Thyroid, and Renal cell CA (very vascular)
- Breast CA may present with 60% of blastic Mets
- Prostate CA presents with 90% of blastic Mets
- Other blastic Mets may derive from urinary bladder, melanoma and GI adenocarcinomas
- Sclerotic foci may also represent as previously treated primaries
- Very vascular Mets like Renal cell and Thyroid may present with markedly lytic and expansile foci often called “blow out Mets.”
- Mets found distal to elbows and knees (acro-metastasis) are commonly associated with Lung CA
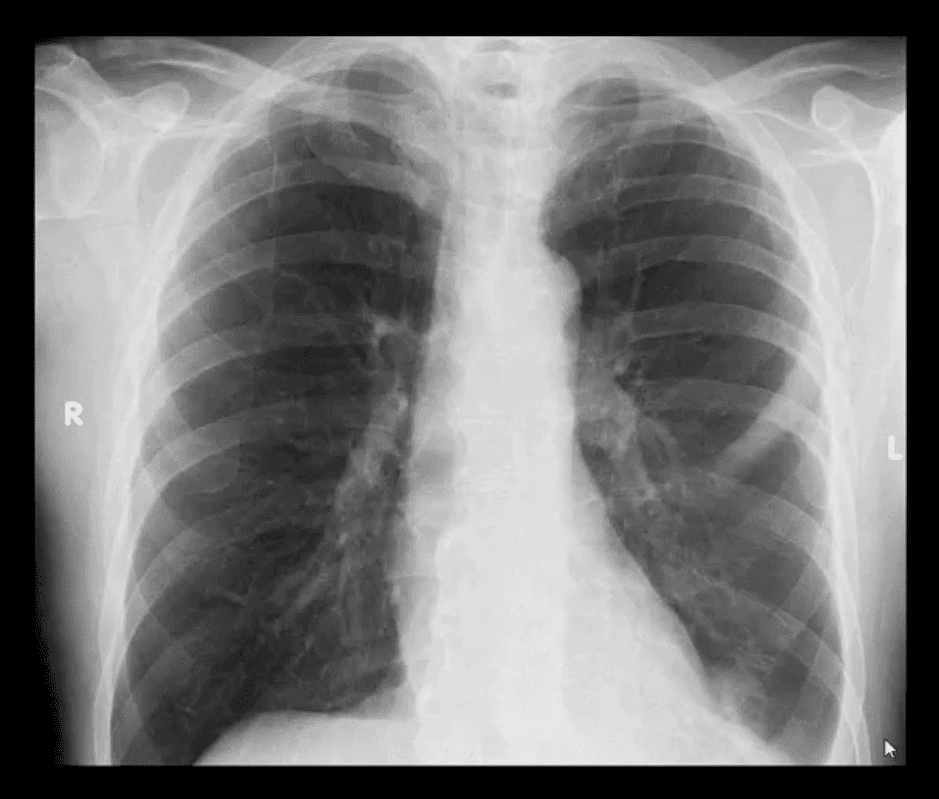
- PA chest view of a routinely screened patient with a known Hx of Prostatic adenocarcinoma
- Note sclerotic lesion identified in the left posterior Rib 5
- What imaging modality is required next?
- Radionuclide bone scan should be suggested
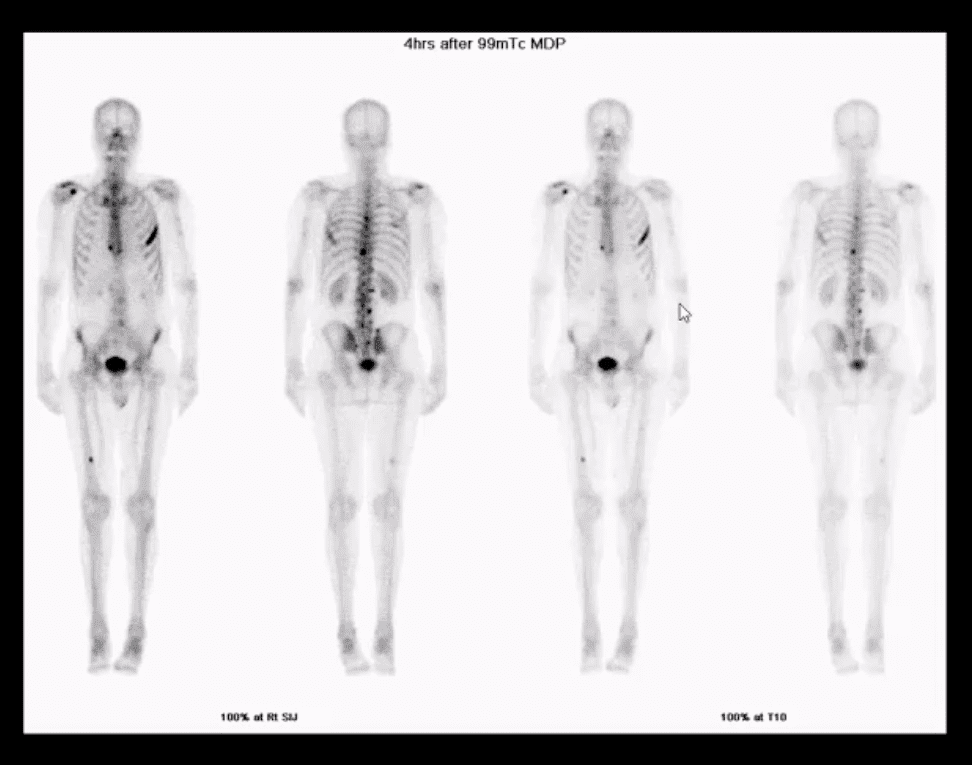
- Multiple foci of high uptake of the Tc99 radiopharmaceutical
- This is due to Mets and increased osteoblastic activity in the thoracic and lumbar spine, ribs and other sites of the skeleton
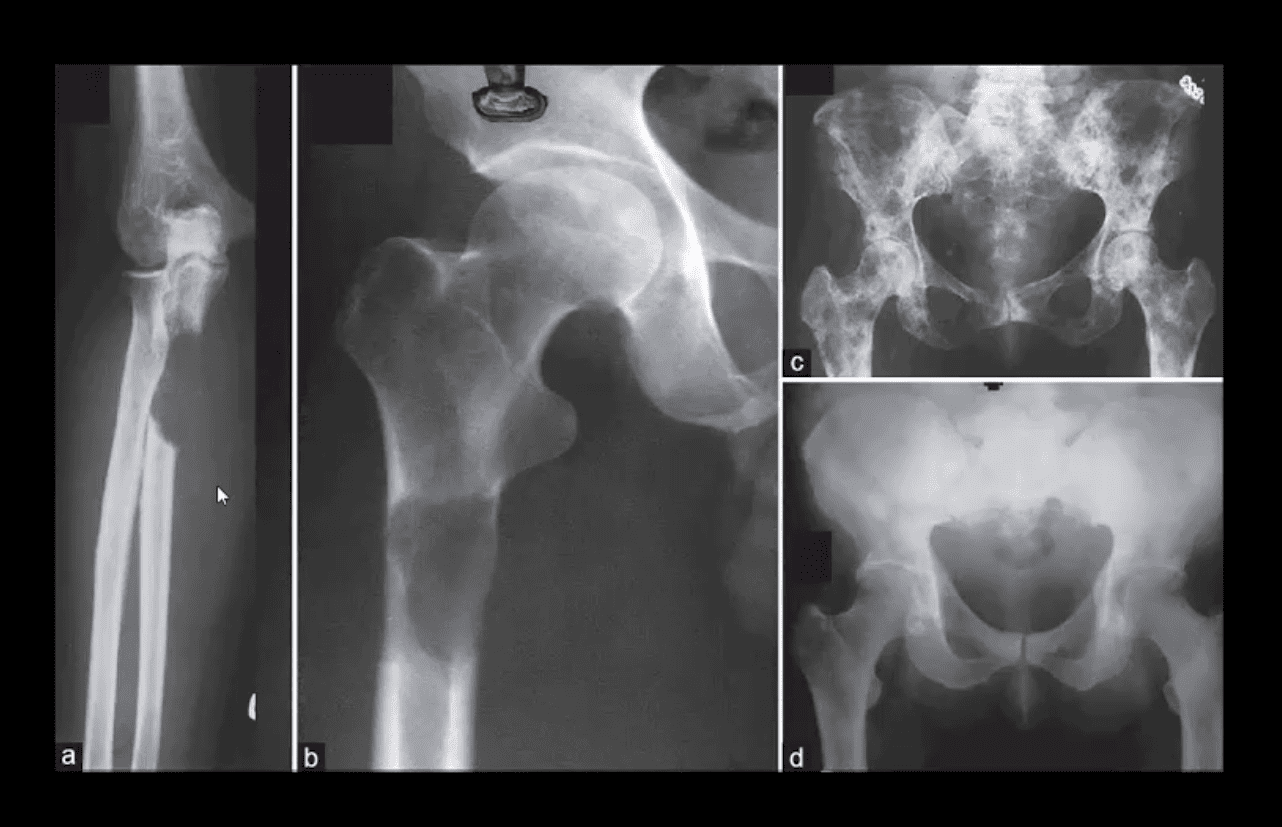
- Comparison of purely lytic (a and b) versus blastic (d) and mixed (c) Mets
- What primaries to consider?

- Frog leg view of the hip
- Clinical Dx: Prostatic adenocarcinoma
- Note diffuse blastic Mets in the proximal femur
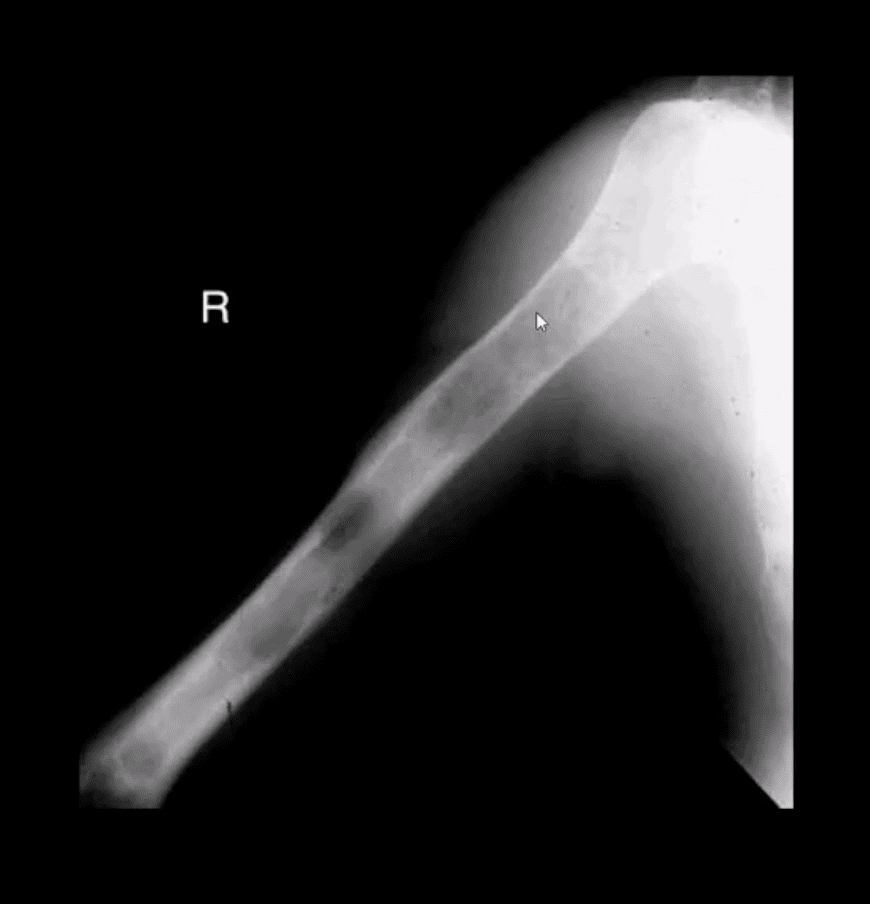
- Hx: severe shoulder and arm pain unrelieved by rest
- Rad DDx: Mets, Myeloma or less frequently Lymphoma
- This classic DDx is used by the majority of Radiologists when aggressive osteolytic bone lesions are noted
- The patient had a known Hx of Breast CA
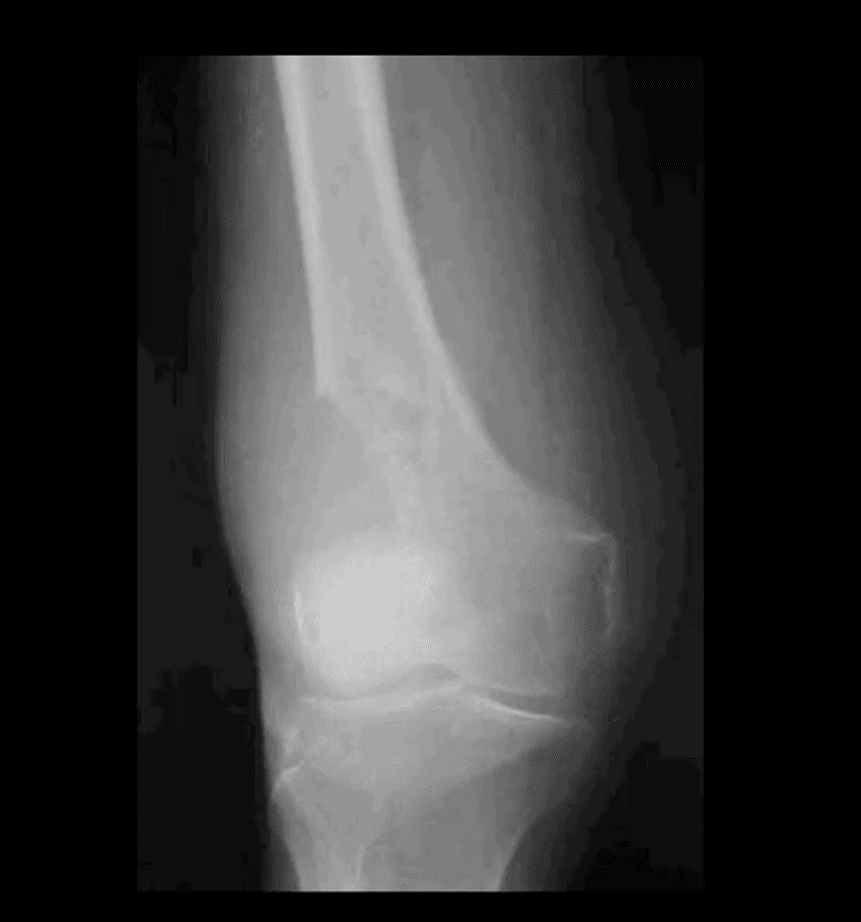
- A 51-year-old female with Breast CA
- Large lytic destructive lesion in the distal femoral metaphysis characteristic of aggressive osteolytic Mets
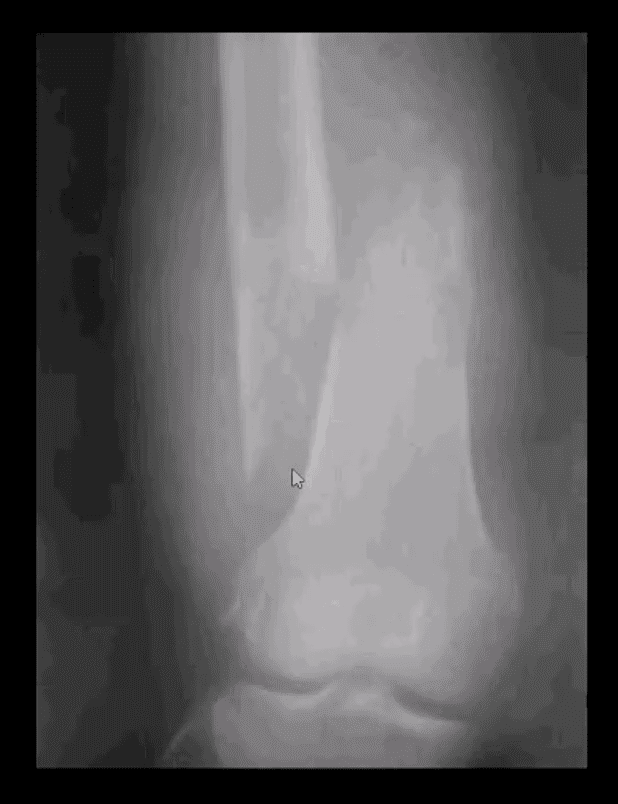
- Sudden onset of severe leg pain and inability to stand in a 53-year-old female with Breast CA
- Dx: Pathological fracture through the distal femoral shaft
- Pathological Mets fractures in the spine and extremities are dreaded by most Oncologists due to higher association with severe complications and poor clinical prognosis
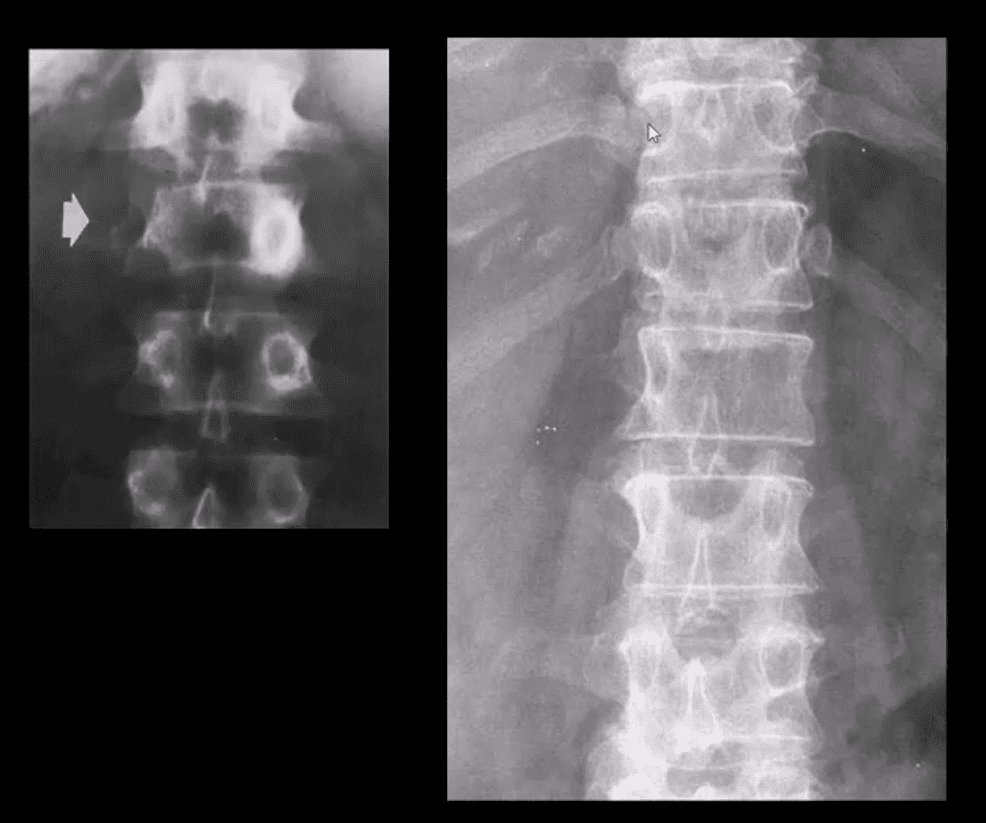
- Radiographic Dx of vertebral Mets should be suspected if a “missing pedicle sign” aka “winking owl sign” is noted
- DDx: pedicle agenesis (above left) shows hypertrophy and sclerosis of a contralateral pedicle d/t increased mechanical stress
- Pedicle Mets are often thought of as the m/c initial site of spinal Mets
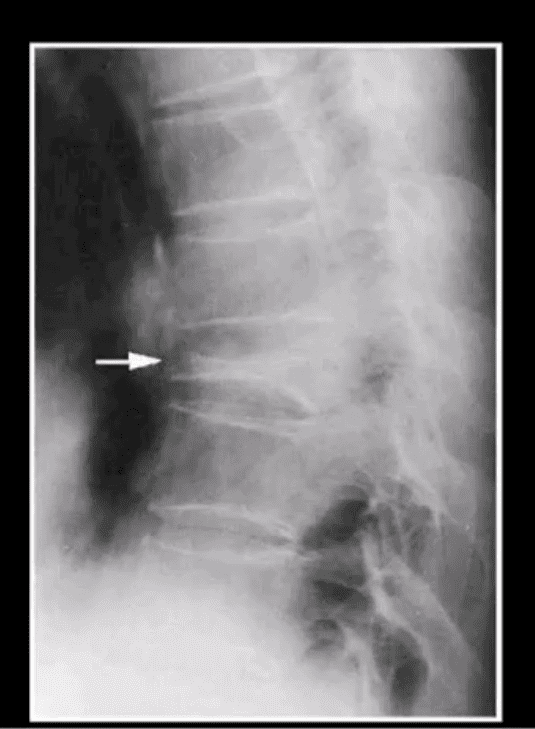
Vertebral Body Pathologic Fracture (VERTEBRA PLANA)
- Isolated compression fracture at the T8 segment noted (above arrow)
- The loss of the posterior and anterior height suggest an underlying pathologic condition for which the differential diagnosis includes:
- Multiple myeloma
- Metastatic Carcinoma
- Other malignancy
- Osteoporosis
- Differentiating Pathological Fx of the vertebral body from an osteoporotic insufficiency Fx can be a significant challenge
- Close inspection of the posterior body height is helpful but often not reliable
- In metastasis, the posterior body is collapsed
- In OSP, the posterior body may be maintained appearing more as anteriorly wedge fracture
- MR imaging and/or radionuclide bone scan need to be performed
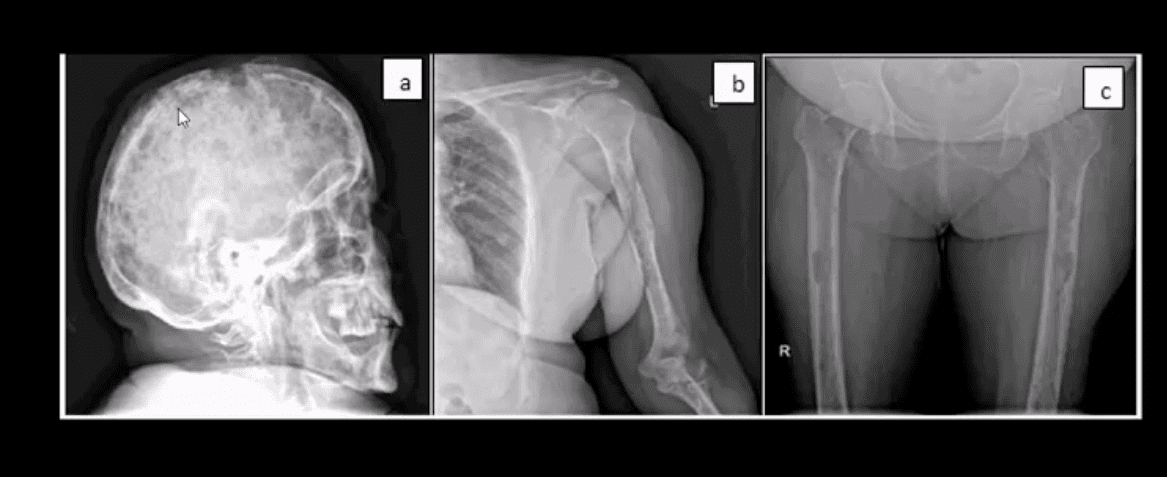
- A skeletal radiographic survey may be used occasionally for the evaluation of bone Mets especially in well-established cases
- It includes bilateral AP & lateral Thoracic and Lumbar views, AP pelvis, humeri, femurs, and the skull
- Availability of special imaging has supplanted the use of skeletal radiographic survey
- However, in a clinical practice skeletal radiographic study of Multiple Myeloma may still be used primarily if the diagnosis was previously established

Technetium-99 (99mTc) bone scintigraphy is very sensitive and cost-effective study:
- For the detection/localization of Mets and often an assessment of their biologic activity and response to treatment
- This modality is a well-established part of the workup for known as well as unknown primaries
- It may also help with determination of lesions that will be most accessible and easy to biopsy
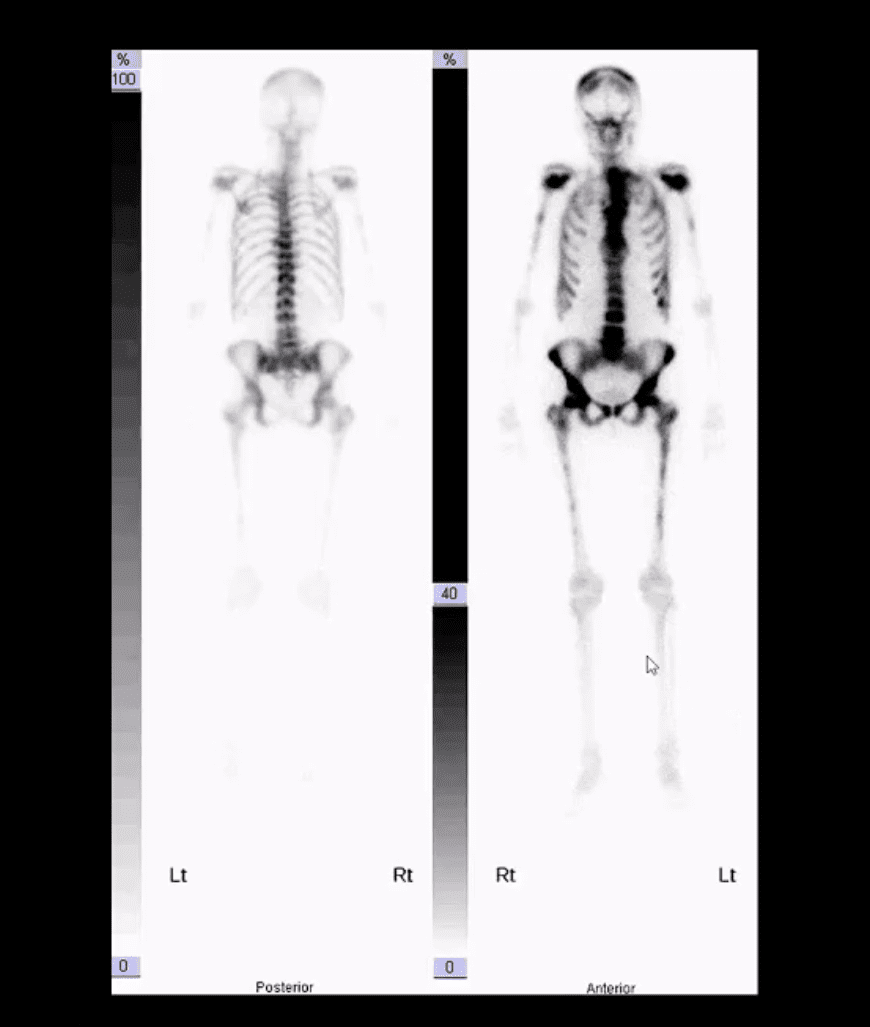
- When the burden of Mets is significantly high as shown in the case above
- The radiotracer uptake is being almost entirely taken in by metastatic lesions
- No material is left for the kidneys to excrete
- This is known as a “super scan”

- Sagittal Lumbar and Lower Thoracic MRI. Multiple metastasis are noted on T1 (above right) and T2 (above left)Â WI as hypointense foci of marrow replacement of the vertebral bodies in a patient with Hx of Prostate CA
- MR imaging protocol with T1, T2, and T1+C gad can be used in many cases if x-radiography is unrewarding or questionable
- Â MRI can reveal bone marrow changes due to bone marrow replacement by Mets and surrounding edema
- Typically blastic Mets appear as abnormally decreased signal intensity (hypointense) lesions on T1 and T2 pulse sequences
- Purely lytic Mets often appear as hypo-intense on T1 and hype-intense on T2
- Increased gadolinium uptake may also be evident on T1+C fat suppressed sequence d/t increased vascularity of malignant foci especially in very aggressive vascular neoplasms
Spinal Neoplasms
Post Disclaimer
Professional Scope of Practice *
The information herein on "Spinal Neoplasms Diagnostic Imaging Approach Part I" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics




 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.