Individuals suffering from hip, thigh, and/or groin pain could be experiencing iliopsoas syndrome. Could knowing the symptoms and causes help in diagnosis and treatment?
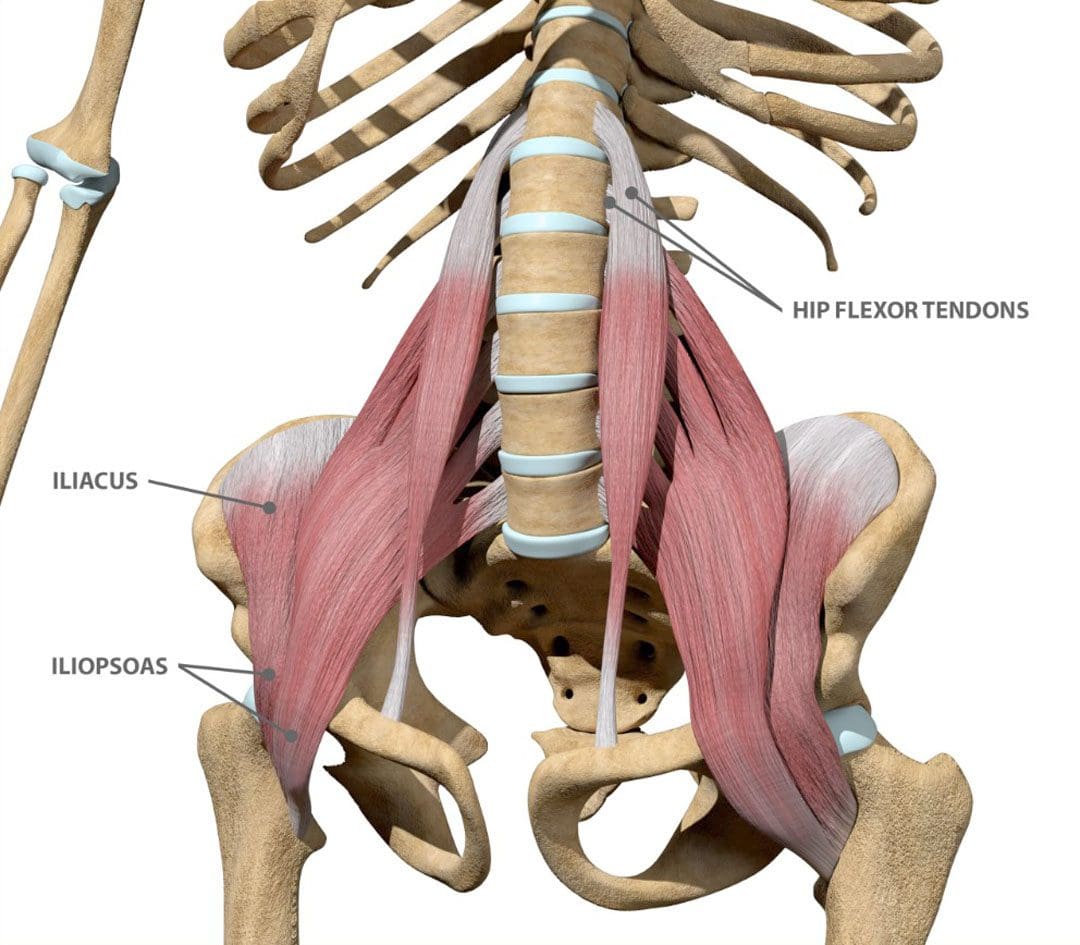
Table of Contents
Iliopsoas Syndrome
Iliopsoas syndrome encompasses several conditions that affect the inner hip muscle and can cause hip and thigh pain. The muscle helps to bend the leg toward the body.
- The condition is usually caused by overuse injuries and commonly affects individuals who perform repeated hip flexion movements, like cyclists, gymnasts, dancers, runners, and soccer players. (Liran Lifshitz, et al., 2020)
- The term is often used interchangeably with psoas syndrome, iliopsoas tendonitis, snapping hip syndrome, and iliopsoas bursitis. However, there are clinical differences.
Symptoms
Symptoms include: (American Association of Hip and Knee Surgeons. 2020)
- Tenderness in the hip and groin area.
- Hip or groin clicking or snapping that can be heard and/or felt during movement.
- Pain and/or stiffness in the hip and thigh area.
- Pain that worsens when bending the hip – walking, climbing stairs, squatting, sitting.
- Movements that involve bringing the knee toward the chest can worsen the pain.
Causes
The iliopsoas muscles are hip muscles on the front of the hip. They are made up of the psoas major, the psoas minor, and the iliacus. Small, fluid-filled sacs/bursae are within the hip joint between bones and soft tissues. The bursae reduce friction and provide cushioning to help the tendons, muscles, and other structures move smoothly over the bony prominences.
- The greater trochanteric bursa and the iliopsoas bursa can become inflamed, which can lead to the syndrome. (American Association of Hip and Knee Surgeons. 2020)
- Iliopsoas bursitis happens when the bursa, which is located between the iliopsoas tendon and the inside of the hip joint, becomes inflamed and irritated.
- Iliopsoas tendonitis/hip tendonitis happens when the tendon that attaches the thigh bone to the iliopsoas muscle becomes inflamed and irritated.
- Overuse injuries and intense activities like cycling, running, rowing, or strength training commonly cause iliopsoas bursitis and tendonitis.
Diagnosis
- Healthcare providers can diagnose iliopsoas syndrome based on symptom history and a hip examination.
- Imaging tests – MRI and X-rays may be used to rule out other injuries or conditions like muscle tears. (Paul Walker et al., 2021)
Treatment
Most mild cases of hip bursitis and hip tendonitis can be managed using the RICE method (American Association of Orthopedic Surgeons. 2020)
Rest
- Avoid putting weight on the hip for a few days after the injury.
Ice
- Apply ice immediately after the injury to bring the swelling down.
- Use a cold pack for 20 minutes at a time, several times a day.
- Do not apply ice directly on the skin.
Compression
- Wrap the area in a soft bandage or use compression shorts to prevent further swelling.
Elevation
- Rest as often as possible with the leg raised higher than the heart.
Medical Treatment
- Non-steroidal anti-inflammatory drugs like ibuprofen and naproxen sodium can alleviate pain and reduce inflammation. (Paul Walker et al., 2021)
- Steroid injections can be used if symptoms continue or come back with additional injections administered as necessary. (Paul Walker et al., 2021)
- After pain and swelling subside, physical therapy may be recommended, as well as mild exercises to gradually improve hip strength and flexibility. (Paul Walker et al., 2021)
- A healthcare provider may recommend surgery in severe cases where pain persists, and conservative treatments don’t provide enough relief.
- However, this is rare due to muscle weakness and nerve damage risks. (Paul Walker et al., 2021)
Hip Labral Tear – Chiropractic Treatment
References
Lifshitz, L., Bar Sela, S., Gal, N., Martin, R., & Fleitman Klar, M. (2020). Iliopsoas the Hidden Muscle: Anatomy, Diagnosis, and Treatment. Current sports medicine reports, 19(6), 235–243. https://doi.org/10.1249/JSR.0000000000000723
American Association of Hip and Knee Surgeons. Iliopsoas tendonitis/bursitis.
Walker, P., Ellis, E., Scofield, J., Kongchum, T., Sherman, W. F., & Kaye, A. D. (2021). Snapping Hip Syndrome: A Comprehensive Update. Orthopedic reviews, 13(2), 25088. https://doi.org/10.52965/001c.25088
American Association of Orthopedic Surgeons. OrthoInfo. Hip strains.
Post Disclaimer
Professional Scope of Practice *
The information herein on "Signs You Need to Get a Diagnosis for Iliopsoas Syndrome" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.