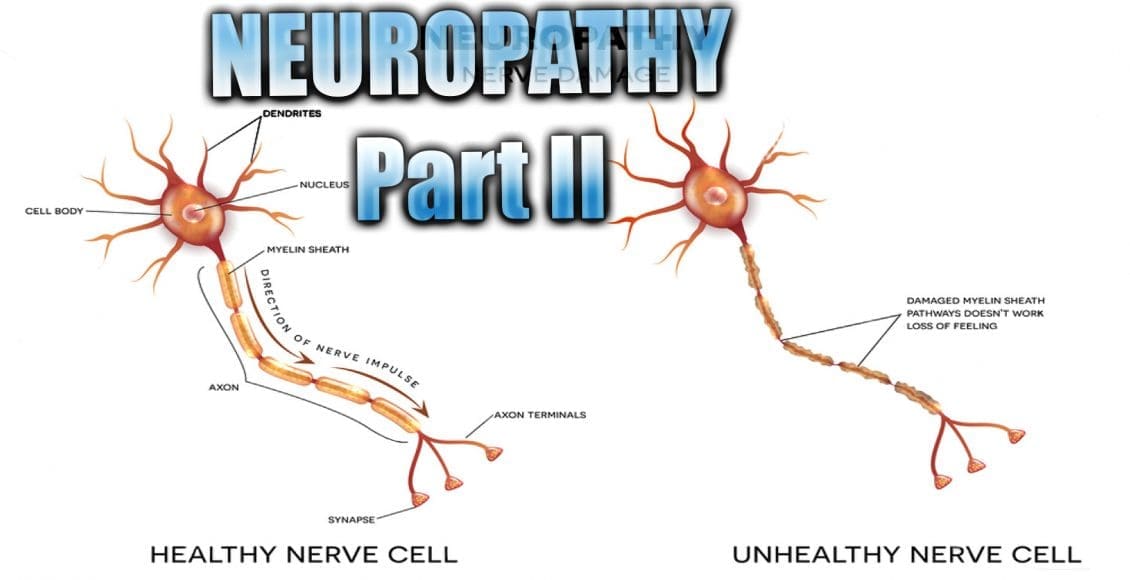
Neuropathy Presentation II: El Paso, TX. Chiropractor, Dr. Alexander Jimenez continues the overview with neuropathy part II. Continued are the most common neuropathies to be seen in practice. Because the human body is composed of many different kinds of nerves which perform different functions, nerve damage is classified into several types. Neuropathy can also be classified according to the location of the nerves being affected and according to the disease causing it. For instance, neuropathy caused by diabetes is called diabetic neuropathy. Furthermore, depending on which nerves are affected will depend on the symptoms that will manifest. The complications which follow neuropathy depends on the type of nerves that are damaged. According to Dr. Jimenez, different neuropathies can cause numbness and/or tingling sensations, increased pain or the loss of ability to feel pain, muscle weakness along with twitching and cramps, even dizziness and/or loss of bladder control function.
Table of Contents
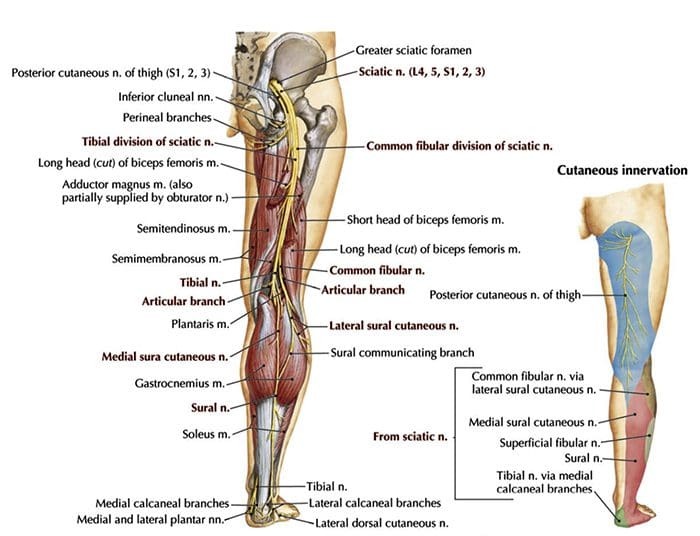
Sciatic Nerve Entrapment
- Piriformis Syndrome
- Peroneal Nerve Entrapment
- Tarsal Tunnel Syndrome
Sciatic N. Piriformis Syndrome
 Causes
Causes
- Anatomic variation
- Piriformis overuse/tension
Exam
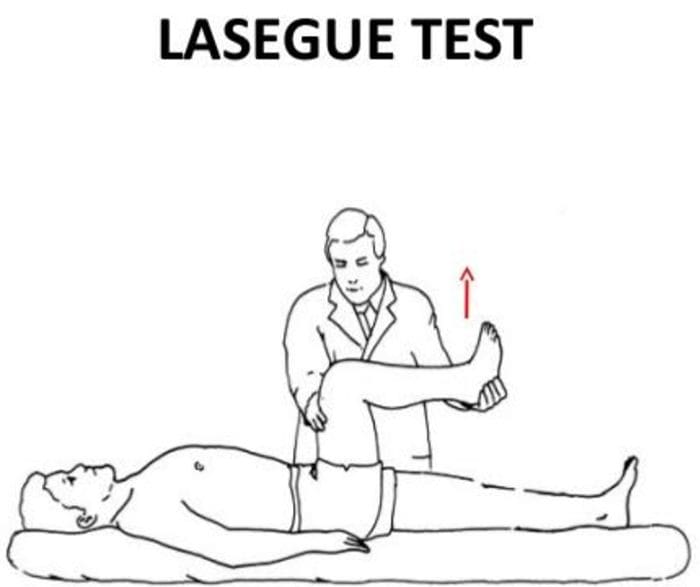
- Positive Lasègue test possible
- Doctor extends patient’s leg passively, while patient is lying supine positive test if maneuver is limited by pain
- Tenderness and palpable tension in piriformis muscle which elicits symptoms
Sciatic N. Peroneal Nerve Entrapment
- Peroneal or Fibular branch of Sciatic nerve entrapped at the fibular head
- Tinel’s sign may be present at fibular head/neck
- Usually affects common peroneal nerve, therefore motor and sensory symptoms can be seen
- Weakness of ankle dorsiflexion and eversion (tibialis anterior m.)
- Sensory disruption on the dorsum of the foot and lateral aspect of the calf
Sciatic N. Tarsal Tunnel Syndrome
- Tibial nerve impinged in the tarsal tunnel
- Sensory changes in the sole of the foot
- Tinel’s sign may be present with percussion posterior to the medial malleolus
 Radiculopathy
Radiculopathy
- A mononeuropathy – located in one specific area
- Neuropathy involving spinal nerve roots
- Presents as changes in sensory and/or motor function affecting a single or a few nerve root level(s)
- Most commonly seen radiculopathies include:
- Sciatica
- Cervical radiculopathy
Common Causes Of Radiculopathy
- Disc herniation
- Osteophytes
- Spinal Stenosis
- Trauma
- Diabetes
- Epidural abscess or metastasis
- Nerve sheath tumors (schwannomas and neurofibromas)
- Guillain-BarreÌ syndrome
- Herpes Zoster (shingles)
- Lyme disease
- Cytomegalovirus
- Myxedema/Thyroid disorder
- Idiopathic neuritis
Narrowing Down Common Causes Of Radiculopathy
-
Disc Herniation
- Most commonly affected nerve roots are C6, C7, L5 & S1
-
Spinal Stenosis
- Lumbar stenosis may produce neurogenic claudication
- Pain & weakness with ambulation
- Cervical stenosis may present with mixed picture of radiculopathy and myelopathy due to long tract involvement
-
Trauma
- May cause compression, trauma or avulsion of the nerve roots
-
Diabetes
- More likely to cause a polyneuropathy, but mononeuropathy is possible
-
Herpes Zoster (Shingles)
- Most often on the trunk, accompanied by vesicular lesions in a single dermatome
- If pain persits past vesicular regression = post-herpetic neuralgia
Patient History Of Radiculopathy
- The patient will often complain of burning pain or tingling that radiates or shoots down an affected area in a dermatomal pattern.
- Sometimes patient will complain of motor weakness, however if onset is recent, there is often no motor involvement
Exam Of Radiculopathy
- Most often hypoesthesia in the affected dermatome level
- Best to evaluate for pain, as light touch can be difficult for these patient’s to distinguish
- Fasciculations and/or atrophy may be seen if radiculopathy is chronic, due to lower motor neuron being impinged
- Motor weakness may be seen in muscles innervated by the same root level
Orthopedic tests:
-
Straight-leg raise test (SLR)
- Pain between 10-60 degrees likely indicates nerve root compression
-
Well-leg raise/Crossed straight-leg raise test (WLR)
- If positive, 90% specificity for L/S nerve root compression
-
Valsalva Maneuver
- Positive if increase in radicular symptoms
-
Spinal Percussion
- Pain may indicate metastatic disease, abscess or osteomyelitis
Examinations: Merck Manual Professional
How To Test Reflexes
How To Do A Sensory Exam
How To Do A Motor Examination
Dermatomes
 Testing Cervical Nerve Roots
Testing Cervical Nerve Roots
 Testing Lumbosacral Nerve Roots
Testing Lumbosacral Nerve Roots
Specific Radiculopathy Patterns
-
T1 radiculopathy can cause Horner’s syndrome
- This is due to affect on cervical sympathetic ganglia
- Ptosis, miosis, anhidrosis
-
Below L1, radiculopathies can cause Cauda Equina syndrome
- Saddle anesthesia (sensory loss in S2-S5 distribution)
- Urinary retention or overflow incontinence
- Constipation, decreased rectal tone or fecal incontinence
- Loss of erectile function
- Must be referred for emergency care immediately to prevent permanent dysfunction
Other Patterns Of Neuropathy
-
Cape/Shawl distribution of symptoms
- Intramedullary lesion
- Syringomyelia
- Intramedullary tumor
- Central cord damage
-
Stocking and Glove Distribution of Symptoms
- Diabetes mellitus
- B12 deficiency
- Alcoholism/hepatitis
- HIV
- Thyroid dysfunction/myxedema
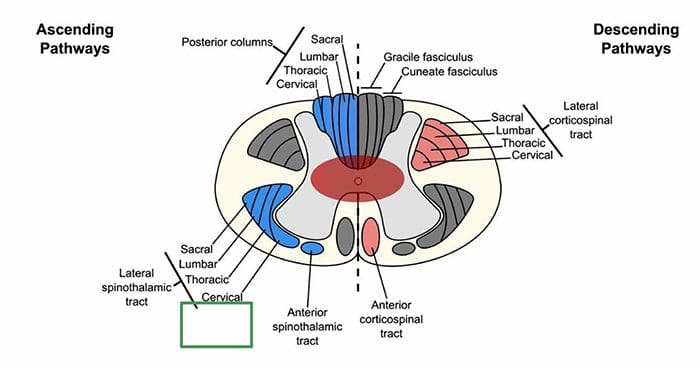
Cape/Shawl Pattern
- Intramedullary lesion such as tumor, syringomyelia or hyperextension injury in patient with C/S spondylosis
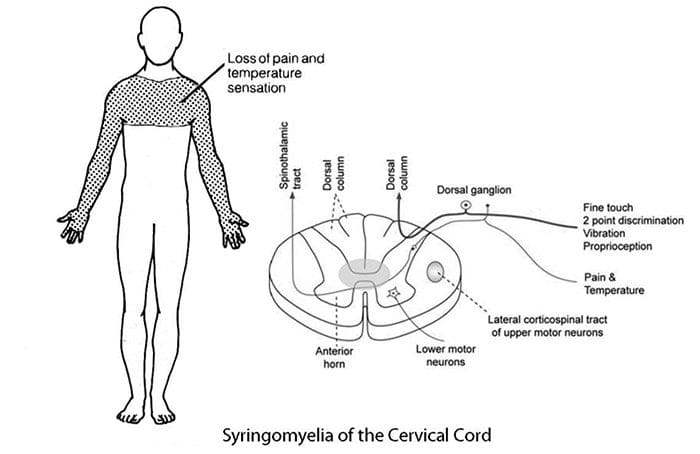
- Loss of pain and temp sensation in C/T dermatomes because of arrangement of lateral spinothalamic tract
 Stocking & Glove Pattern
Stocking & Glove Pattern
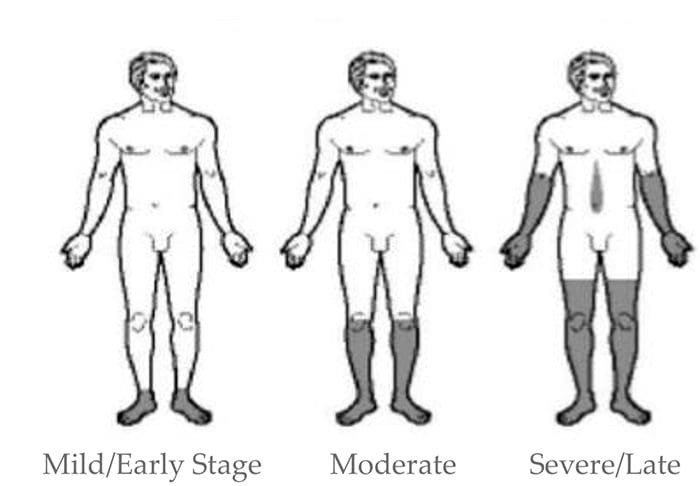
- Symmetrical polyneuropathy
- Feet/legs usually affected first, followed by hands/arms
- Vibration sensation in the smallest toes is usually the first thing lost and neuropathy progresses across foot to great toe and then upward through the ankle and leg, then hands, arms and finally trunk if sever
- Most likely cause of this distribution is diabetes mellitus, but other possible causes include B12 deficiency, alcoholism, HIV, chemotherapy treatment, thyroid dysfunction and multiple other causes
Diabetic Neuropathy
- Diabetic neuropathy often presents as a polyneuropathy but can also present as a mononeuropathy, usually with acute onset
- Most common in CN III, femoral and sciatic nerves
Demyelinating Neuropathies
- Acute inflammatory demyelinating polyneuropathy (Guillain-BarreÌ syndrome)
- Chronic inflammatory demyelinating polyneuropathy
Guillain-BarreÌ Syndrome (AIDP)
- Onset 1-2 weeks post viral infection
- Progressive weakness
- Loss of DTRs/areflexia
- Paresthesia in hands and feet
- More motor involvement than sensory
- Potential autonomic fiber involvement
- Elevated CSF protein
- EMG/NCV studies indicate demyelination
- May require treatment with plasmapheresis or IV Ig therapy
Chronic Inflammatory Demyelinating Polyneuropathy
- Appears similar to AIDP but does not follow infection
- Symptoms must be present for at least 8 weeks for this diagnosis to be considered
- Anti-inflammatory treatments may help
By Rachel Klein, ND, DC, DACNB
National University of Health Sciences Master of Science (MS) – Advanced Clinical Practice (ACP) MS ACP 551: Clinical Neurology © 2018
Sources
Blumenfeld, Hal. Neuroanatomy through Clinical Cases. Sinauer, 2002.
Evans, Ronald C. Illustrated Orthopedic Physical Assessment. Mosby/Elsevier, 2009.
“Radial Nerve Entrapment: Background, Anatomy, Pathophysiology.†Medscape, 25 Oct. 2017, emedicine.medscape.com/article/1244110- overview#a8.
Post Disclaimer
Professional Scope of Practice *
The information herein on "Neuropathy Presentation | El Paso, TX. | Part II" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


 Causes
Causes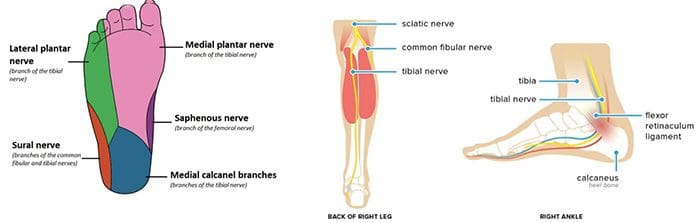 Radiculopathy
Radiculopathy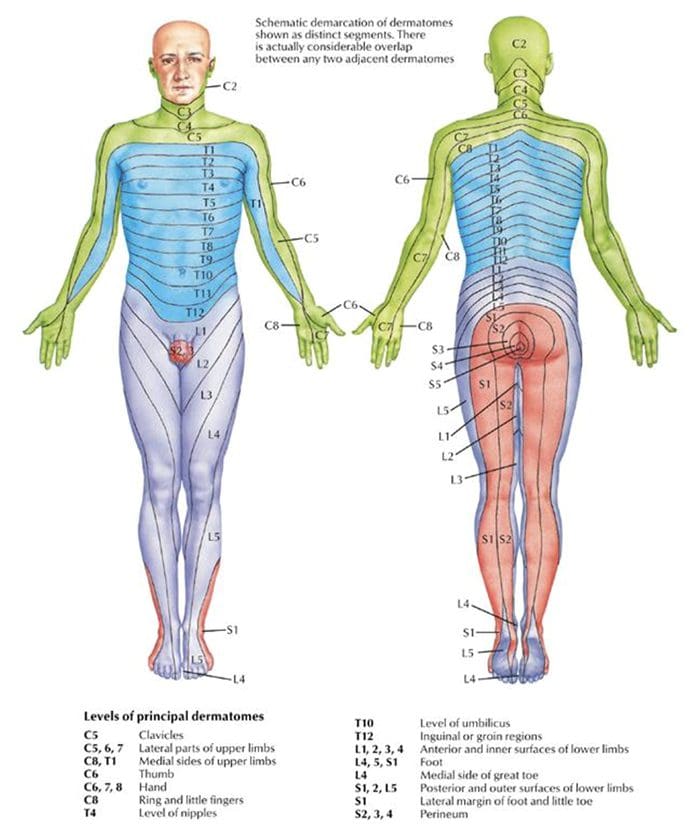 Testing Cervical Nerve Roots
Testing Cervical Nerve Roots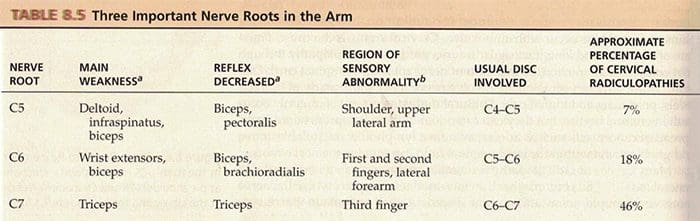 Testing Lumbosacral Nerve Roots
Testing Lumbosacral Nerve Roots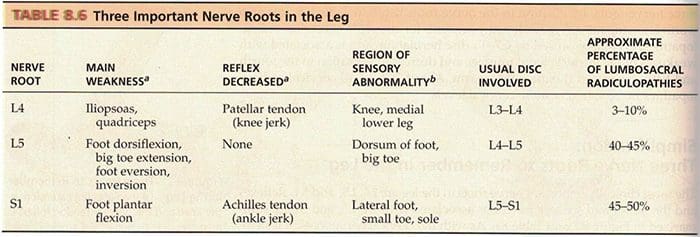
 Stocking & Glove Pattern
Stocking & Glove Pattern

 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.