Sooner or later, you’re going to tweak your back, and there’s nothing you’ll ever experience, perhaps shy of limb dismemberment, that’ll put a stop to your training as cruelly or effectively. Of course, if you’ve already had some back problems, you know what we’re talking about. Either way, we recommend you bone up on the back. It’s one complex little beastie.
A few years ago, I authored the “Shoulder Savers†series here at T Nation. It was, without a doubt, the most popular collection of articles I’ve ever written. I still get feedback every day relating to these articles, and I’ve actually had people come to Boston from other countries just to have me look at their chronic shoulder issues — in spite of the fact that I’m not even a physical therapist.
In the course of working with these individuals, I came to realize several things, most notably:
- A lot of them got sub-par, outdated physical therapy.
- They were just as concerned about maintaining a training effect while injured as they were about actually fixing the injury.
- They lived and died by their diagnostic imaging (MRI, x-ray, etc.), but paid little attention to the relationship of those scans to their symptoms and functional deficits.
- Most sought to learn more about their injuries so that they could be informed consumers in dealing with doctors and therapists, but they wound up more confused because of the varying opinions in the field today.
- They were looking for direction in how to progress back into a “regular†training regimen, but all that most of them could seem to get from their clinicians was contraindications (“don’t do thisâ€).
To me, the Shoulder Savers series was popular “accidentally†because it addressed a lot of these issues. It’s my hope that in this series, we can do the exact same thing with lower back pain, which is likely an even bigger issue in the weight-training population.
So, without further ado (and in no particular order), here are some recommendations for you.
Table of Contents
1 – Read Dr. Stuart McGill’s Work.
I firmly believe that the secret to ever becoming an expert in anything is to recognize that there’s a ton you still have to learn. I’ve read from each of the varying schools of thought on back pain, and Dr. McGill’s theories and recommendations are the ones that have proven the most valuable in training my athletes.
I firmly believe that his versatility is what makes him the best in the world. In addition to seeing patients with debilitating back pain, he also sees athletes in both injury prevention and rehabilitation contexts. And, he’s done research on everything from pig spines to Strongman competitors. He’s written books from both the clinical perspective and the applied perspective.
So, if there’s one recommendation I can make to kick this series off on the right foot, it’s that you should get your hands on Dr. McGill’s works. When it comes to back pain, he’s the best around.
2 – Recognize that you will almost certainly have back pain in your life — at least the way we’re going.
I’ve seen estimates that approximately 80% of Americans suffer from lower back pain during the course of their lives, and roughly 25% of Americans are in pain at any given time. In consideration of these numbers, I’ll recite a great quote I heard back in 2003 from Dr. Jeff Anderson, head of sports medicine at the University of Connecticut: “If you live your life the right way, you’ll likely find yourself in an orthopedist’s office at some point. If you live it the wrong way, you’ll likely end up in cardiologist’s office instead.â€
Both athletes and non-athletes get back pain. Both sedentary and active folks get back pain. Men and women both get back pain. The sooner we realize that spines are weird SOBs, the better off we’ll be. Rest assured that we’ll probably tweak them here and there over the course of a lifetime, even with perfect form, ideal warm-ups, perfect programming, and appropriate load selection. Get used to the idea.
Think about it this way…
How many of you have a friend who has had his back go out simply from tying a shoe or picking up a pencil? I know of a guy who squatted over 800 pounds in competition who threw out his back picking up his cat. Many spine problems are the result of years and years of cumulative trauma — repeated flexion/extension, lateral flexion, and rotation. Who is to say that a lot of that trauma didn’t take place before you ever took up weight training or your sport of choice? Just ask the 4.4% of six-year olds who already have spondylolysis (vertebral fractures).(1)
3 – Recognize that you may never get a definitive diagnosis.
Everyone has known someone with back pain so bad that it stumps every doctor out there. One of my relatives, for instance, has been to hell and back with back pain since some clueless 20-year old girl rear-ended his car at a red light while she was talking on her cell phone. That was over 18 months ago, and he still hasn’t gotten a set-in-stone answer on why he has a crazy burning sensation in his big toe. This is a classic L4-L5 pain pattern, yet everything appears normal at that nerve root.
This actually isn’t uncommon at all. In fact, the author of one meta-analysis in the New England Journal of Medicine found that 85% of back pain cases have no definitive diagnosis.(2) It kind of makes you wonder why they do those MRIs anyway, doesn’t it?
Which leads me to…
4 – Recognize that even though you may be asymptomatic, you’re probably still a complete structural mess.
In 1994, the New England Journal of Medicine published a study that showed that when doctors looked at MRIs of 98 asymptomatic backs. Researchers noted the following:
“52 percent of the subjects had a bulge at at least one level, 27 percent had a protrusion, and 1 percent had an extrusion [82% of subjects]. Thirty-eight percent had an abnormality of more than one intervertebral disk.â€(3)
And, that’s just talking disc issues. In a great study of elite Spanish athletes, spondylolysis (vertebral fractures) proved to be highly prevalent in a wide variety of sports (most notably, track and field throwers, weightlifters, rowers, and gymnasts), yet only 50-60% of those diagnosed under imaging actually reported having lower back pain. (4)
Here you’ve got loads of people with absolutely no pain, yet they have diagnostic imaging that’d tell you that they ought to be in absolute misery.
Here’s a great excerpt from an interview I did with Dr. Jason Hodges, a fantastic radiologist in New York City:
“Regarding the low back, I am a radiologist and I see MRIs every day describing what you said in the newsletter. Lots of people have bulging discs without symptoms. This is especially true of older patients who can have bulging discs at every level but without focal neurologic symptoms. In my experience, younger patients tend to have focal neurological signs with even mild disc bulges or disc herniations. But very often, the symptoms don’t match up with the imaging findings. I have seen patients with symptoms down the right leg, but the disc herniation is on the left side.
“Often imaging findings do not correlate with clinical findings. Older patients often have very degenerative spines without symptoms. Whereas younger patients can have small bulging discs or herniated discs and have debilitating pain. The human body has a great reserve capacity. I see many “normal†kidneys that are in chronic renal failure.
“Medical imaging generally deals with anatomy: how organs “look,†not so much how they function. Obviously, they are linked, but function can decline long before anatomic changes occur. Symptoms can occur without imaging abnormalities. This leads doctors to conclude that nothing is wrong because the x-ray/CT scan/MRI looks normal. This is simply not the case.
“Medical imaging is simply one piece of the clinical puzzle. An analogy can be made with astronomy. You can image the universe at visible light, x-ray, ultraviolet, infrared, etc. Each modality provides a vital, but incomplete picture of the universe. You have to put it all together to get the big picture.â€
So, the next time your favorite athlete goes on the disabled list with a disc bulge, raise an eyebrow and wonder what else is going on. And, be careful when you get up from your chair after reading this article; at least four out of five of you are walking disasters!
5 – Appreciate that your pain and the cause(s) of that pain are usually found in different places.
This point is probably best illustrated by an athlete I first met seven months after he competed at the 2006 Winter Olympics. He had some pretty significant back pain, and a doctor had attributed it to a disc bulge at L4-L5 that had been diagnosed on MRI.
It seemed like a logical assumption — until you actually asked him where his pain was. It turns out it was about four inches up from L4-L5. Anyone who knows anything about pain that originates with disc issues can tell you that it doesn’t radiate up. I introduced him to John Pallof, a fantastic manual therapist that works with a lot of our athletes, and it became pretty clear that his issues came from irritation up near T12-L1.
Essentially, this athlete had locked up the injured L4-L5 segment as a protective adaptation, and while it isn’t a region that should have much motion, it does need a little, so he had to go elsewhere to get that motion.
The result was a crazy hypermobile “hinge†a bit farther up his spine. One treatment of mobilizations four segments lower virtually eliminated his pain altogether.
This same principle can be applied in a variety of contexts. In many cases, acutely improving hip rotation or extension — whether it’s with soft tissue work, mobilizations, or a combination of the two — can relieve one-sided back pain. If a therapist spends all his time just massaging and ultrasounding the area that hurts, though, he’s just studying for the wrong test.
6 – Appreciate the different between flexion-intolerant and extension-intolerant back pain.
Broadly speaking, you can classify the majority of back pain sufferers into extension-based or flexion-based back pain.
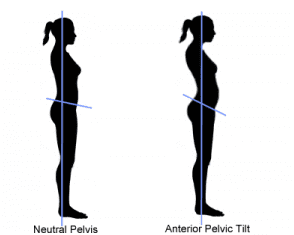
Extension-based back pain typically is worse with standing than with sitting. These folks will present with everything from spondylolysis (fractures), to spondylolisthesis (vertebral slippage), to diffuse lumbar erector “tightness.†Typically, those who suffer from extension-based back pain will have short hip flexors, poor glute function, and a lack of anterior core stability.
Effectively, the hip flexor shortness and insufficient glute contribution leads athletes to substitute lumbar extension for hip extension in movements such as deadlifting, jumping, throwing, or any other task that requires hip extension. The end result is typically some very prominent anterior pelvic tilt, as seen in the photo at right.
Conversely, flexion-intolerant individuals have more pain in sitting, as they tend to have flatter backs and therefore increased stress on the posterior ligaments of the spine. This is your classic symptomatic disc pain patient — with or without radicular pain into the legs.
Flexion intolerance is very common in office workers and cyclists, and you’ll typically see folks with poor psoas function. The psoas is the only hip flexor active above 90 degrees of hip flexion, and typically, these folks will substitute lumbar flexion for hip flexion in these positions.
Unfortunately, it’s been my experience that correcting flexion-based back pain can be a long battle for the exact same reason it develops: it is difficult to get a person to stop sitting so much in today’s world.
As counterintuitive as it may seem, flexion-intolerant individuals will sit in positions of flexion (extension-intolerant patients will sit in positions of extension, too). It might give them temporary relief, but it’s really just making the problem worse in the long run. Modifications such as lumbar support and frequent breaks from sitting can help flexion-intolerant individuals, though.
7 – Appreciate the difference between athletes and desk jockeys.
Several months ago, I was on the phone with a female trainer from the west coast. Somehow, during the course of our conversation, I asked flat-out, “What do you feel the overwhelming majority of back pain patients need?â€
Without hesitation, she responded, “Extension.â€
I nearly dropped the phone; a large percentage of back pain folks who walk through my door are in pain because they already have too much extension. I would have at least expected a response like “multi-directional lumbar stability.â€
However, as I thought about it more, I realized that comparing her clientele to mine was like comparing apples and oranges. I was dealing with almost exclusively athletes, and she was dealing with older adults. My clients spend a ton of time on their feet competing, and hers spent a lot of time seated at a desk.
These two populations need to be treated differently. The extension exercises from McKenzie therapy may exacerbate symptoms in a basketball player with a spondylolisthesis (vertebral slippage), but save a secretary with a disc issue from a world of pain. This is why you never want a clinician who is a carpenter who only owns a hammer: everything starts looking like a nail.
Different people, different spines.
(McKenzie therapy is a method comprising assessment, treatment, and prevention as practiced by therapists trained in the method.)
8 – Recognize that lumbar spine range-of-motion is positively correlated with injury risk.
By now, you’ve probably already read several articles at T Nation that espouse the benefits of training the core for stability and not mobility. If you haven’t, take a look at the following:
High-Performance Core Training
Real “Core†Exercise
Anterior Core Training
Complete Core Training
The premise is pretty simple: you want to move predominantly at your hips and thoracic spine, and while a small amount of movement at the lumbar segments is normal, you don’t want to encourage extra motion there.
As I noted above, there are specific situations that call for individualized mobilization protocols at the lumbar spine, but in terms of what you can accomplish with your own training, the general principles of “mobilize thoracic spine and hips, stabilize lumbar spine†apply.
Here’s where it gets interesting. The American Medical Association (AMA) still uses lumbar spine range of motion as the qualifying criterion for allowing lower back pain patients to return to work. In other words, you needed to attain a certain amount of gross lumbar spine rotational range-of-motion to be considered “safe†to return to work.
Surprisingly, as Parks, Crichton, Goldford, and McGill observed in the discussion of their 2003 study (5), there isn’t a single study out there that shows the lumbar spine range of motion is correlated with having a healthy back; in fact, the opposite is true!
Those with high lumbar spine ROM and power are more likely to be injured, whereas those with better lumbar spine stabilizing endurance are the healthy ones. And, interestingly, there really isn’t any way of knowing what an individual’s original “normal†spine ROM was, so they have to assume that someone had “average†spine ROM.
Yes, that study from the world’s premier spine researchers was published just over six years ago (meaning that the data was probably collected at least seven years ago). Meanwhile, the AMA hasn’t caught on, and chances are many doctors haven’t, either, as this has been the “standard†for decades (28 years, actually, to my knowledge). Why?
Well, for starters, lawyers like solid numbers to which they can adhere to in court. When you have a collection of problems that go undiagnosed in 85% of cases, and a certain percentage of the population who will lie about back pain to get out of work or win a lawsuit, this number becomes even more important.
Until Next Time…
Hopefully, this piece gave you some background on a somewhat nebulous problem that faces a huge portion of both our athletic and non-athletic population. In the articles that follow, I’ll outline more things you ought to know, and corrective strategies to address these issues.
References
- Morita T, Ikata T, Katoh S, Miyake R. Lumbar spondylolysis in children and adolescents. J Bone Joint Surg Br. Jul 1995;77(4):620-5
- Deyo, RA. Fads in the treatment of kow back pain. N Engl J Med. 1991 Oct 3;325(14):1039-40.
- Jensen MC, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med.1994 Jul 14;331(2):69-73.
- Soler T, Calderon C. The prevalence of spondylolysis in the Spanish elite athlete. Am J Sports Med. 2000 Jan-Feb;28(1):57-62.
- Parks KA, Crichton KS, Goldford RJ, McGill SM. A comparison of lumbar range of motion and functional ability scores in patients with low back pain: assessment for range of motion validity. Spine. 2003 Feb 15;28(4):380-4.
Sourced From: Lower Back Savers
Copy Rights: Circle of Docs
Post Disclaimer
Professional Scope of Practice *
The information herein on "Lower Back Savers" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics




 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.