Table of Contents
Meniscal Tears
- Acute or chronic. Imaged with MRI (95% sensitivity & 81% specificity)
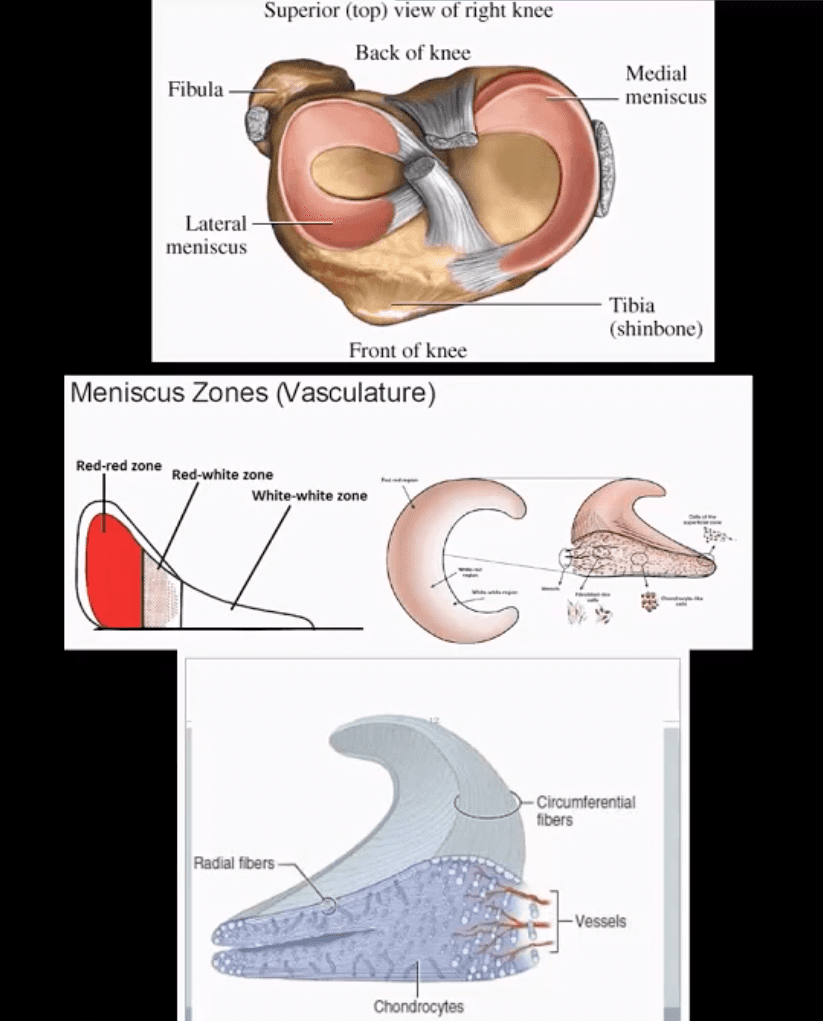
- Menisci are formed by a composition of radial and circumferential collagen fibers (97% type 1) mixed with cartilage, proteoglycans etc. 65-75% H2O
- Aging can lead to meniscal attrition
- Acute tears are d/t rotational and compressive forces, ACL deficient knees show greater chances of meniscal tears
- Posterior horn of medial meniscus is m/c torn except in acute ACL tears when lateral meniscus is m/c torn
- Meniscus is well vascularized in children. In adults 3-zones exist: inner, middle and outer (above bottom image)
- Injury of the inner zone has no chance of healing
- Injury of the outer zone (25% in total) has some healing/repair
Clinical Presentation
- Pain, locking, swelling
- Most sensitive physical sign: pain on palpation at the joint line
- Tests: McMurry, Thessaly, Apply compression in prone
- Management: conservative vs. operative depends on lacation, stability, patient’s age and DJD and the type of tear
- Partial meniscectomy is performed. 80% good functions on follow up. Less favorable if >40-y.o and DJD
- Total meniscectomy is not performed and only viewed historically. 70% OA 3-years after surgery 100% OA after 20 years post surgery.
Axial MR
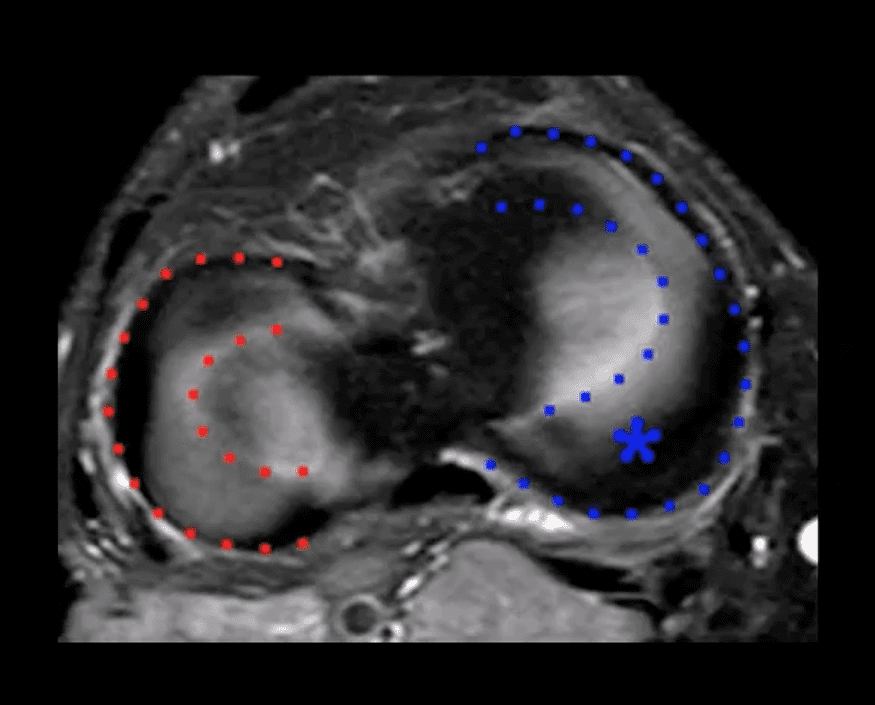
- Appearance the medial (blue) and the lateral meniscus (red)
Menisci Play Significant Role
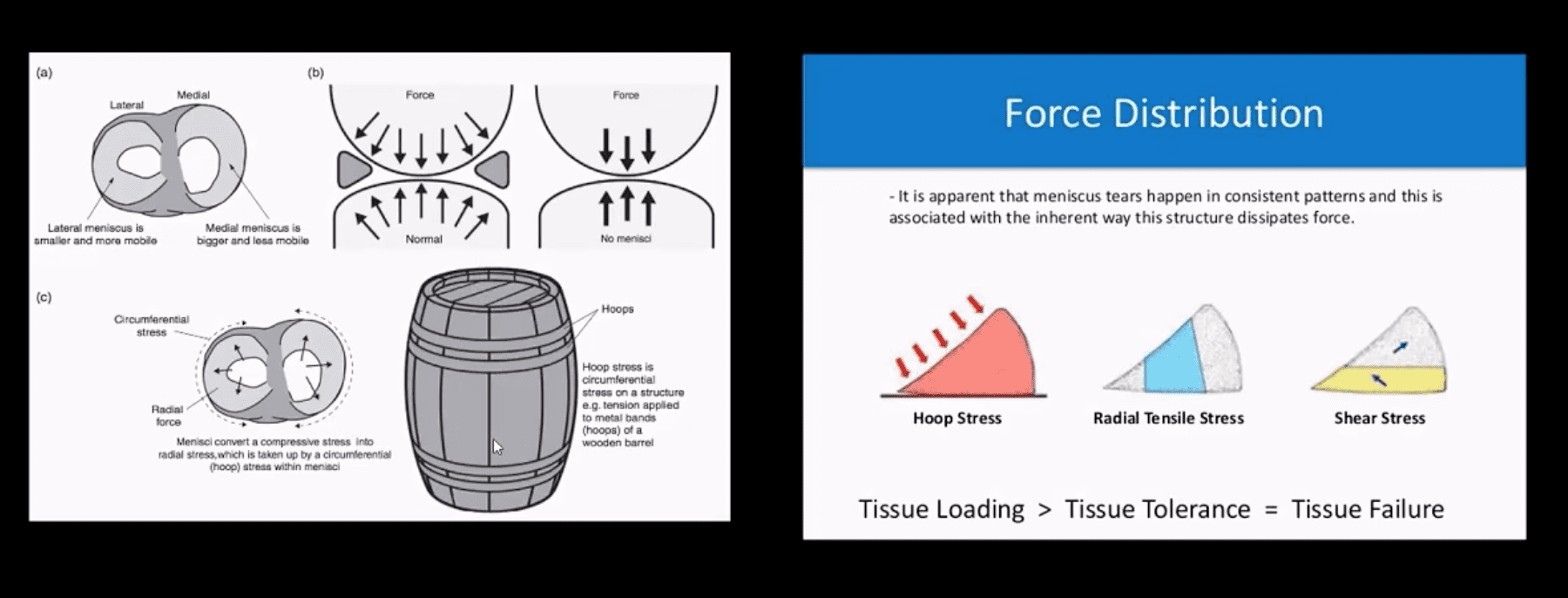
- One of the important roles is “hoop-stress” mechanism.
- Particularly radial tears may significantly interfere with this mechanism.
- Further reading: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3435920/
Types Location & Stability

- Types, location and stability of tears are v. important during MRI Dx
- Vertical/longitudinal tears especially occur in acute ACL tears. Some longitudinal tears found at the periphery or “red zone” may heal
- Bucket handle tear: longitudinal tear in the inner edge that is deep and vertical extending through long axis and may displace into notch
- Oblique/flap/parrot-beak are complex tears
- Radial tear at 90-degree to plateau
Axial T2
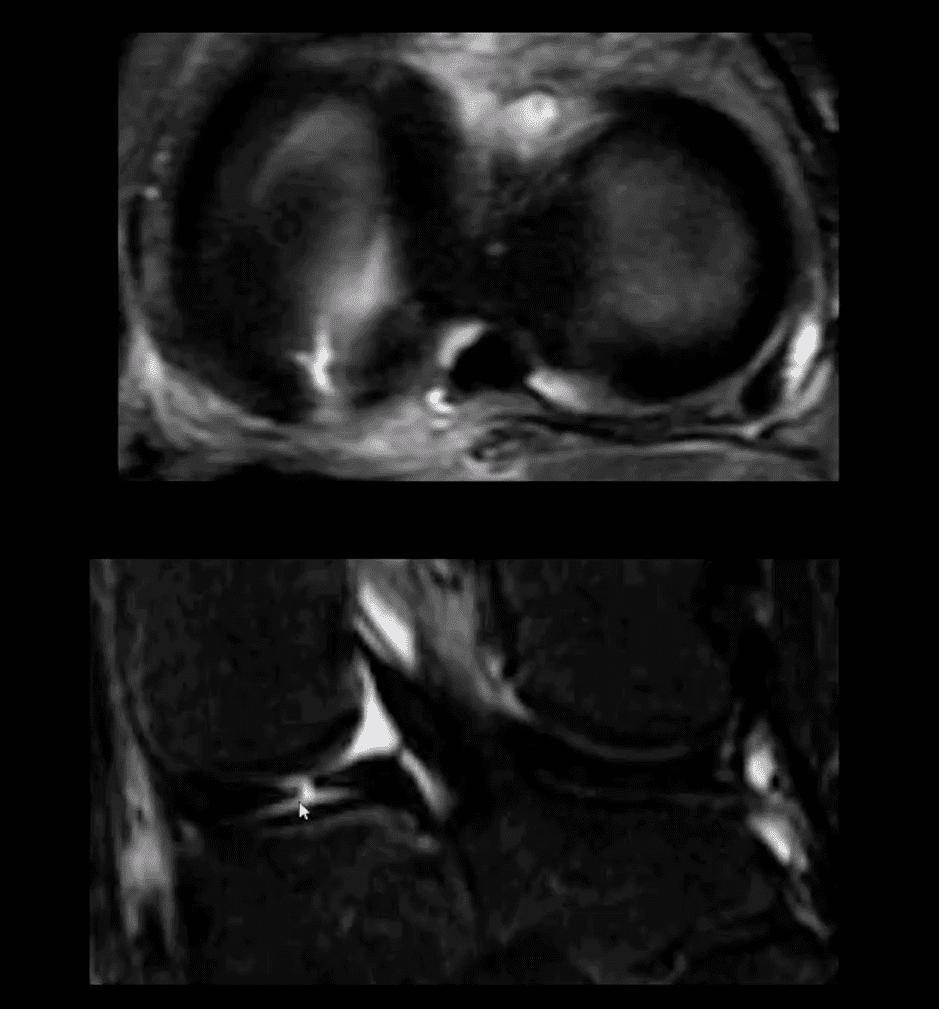
- Axial T2 WI fat-sat and coronal STIR slices of the posterior horn of the medial meniscus.
- Note a radial tear of the posterior horn of the medial meniscus near meniscal root. This is potentially an unstable lesion requiring operative care
- The meniscus in this case is unable to provide a “hoop-stress mechanism”
MRI Slices Coronal & Sagittal
- Fat-sat coronal and sagittal proton density MRI slices revealing horizontal (cleavage) tear that is more typical in the aged meniscus
- In some cases, when this tear does not contain a radial component it may partially heal obviating the need for operative care
T2 w GRE Sagittal MRI Slice
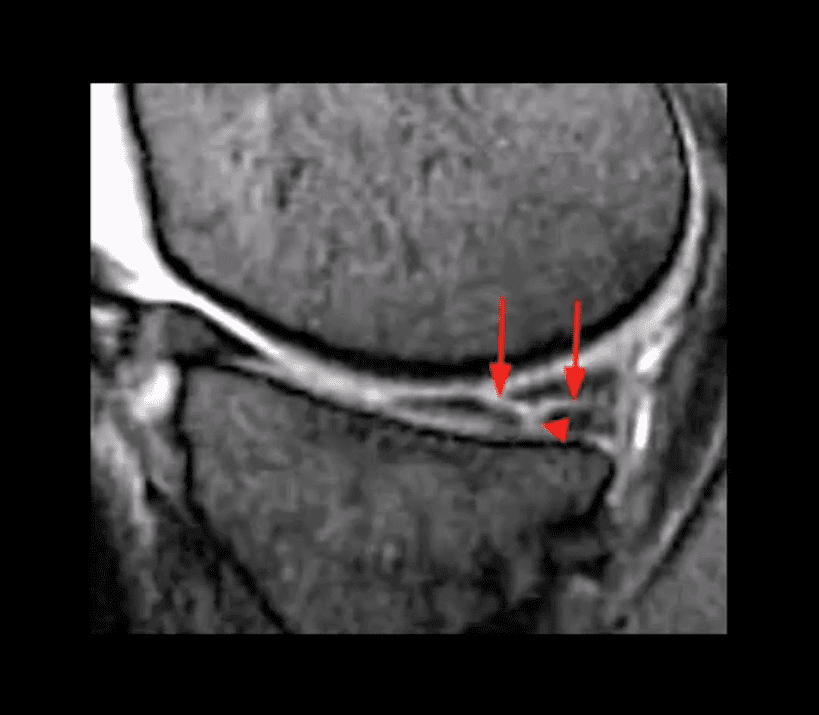
- Complex tear with a horizontal oblique and radial component.
- This type of tear is very unstable and in most cases may need operative care
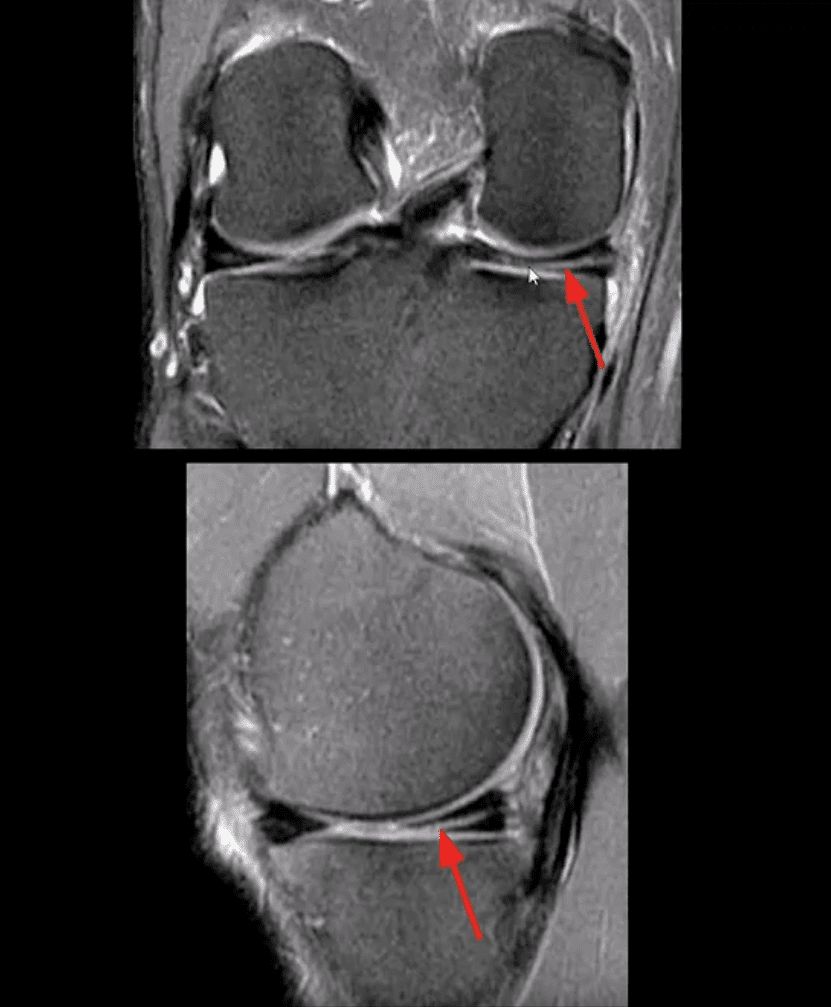
Bucket Handle Tear
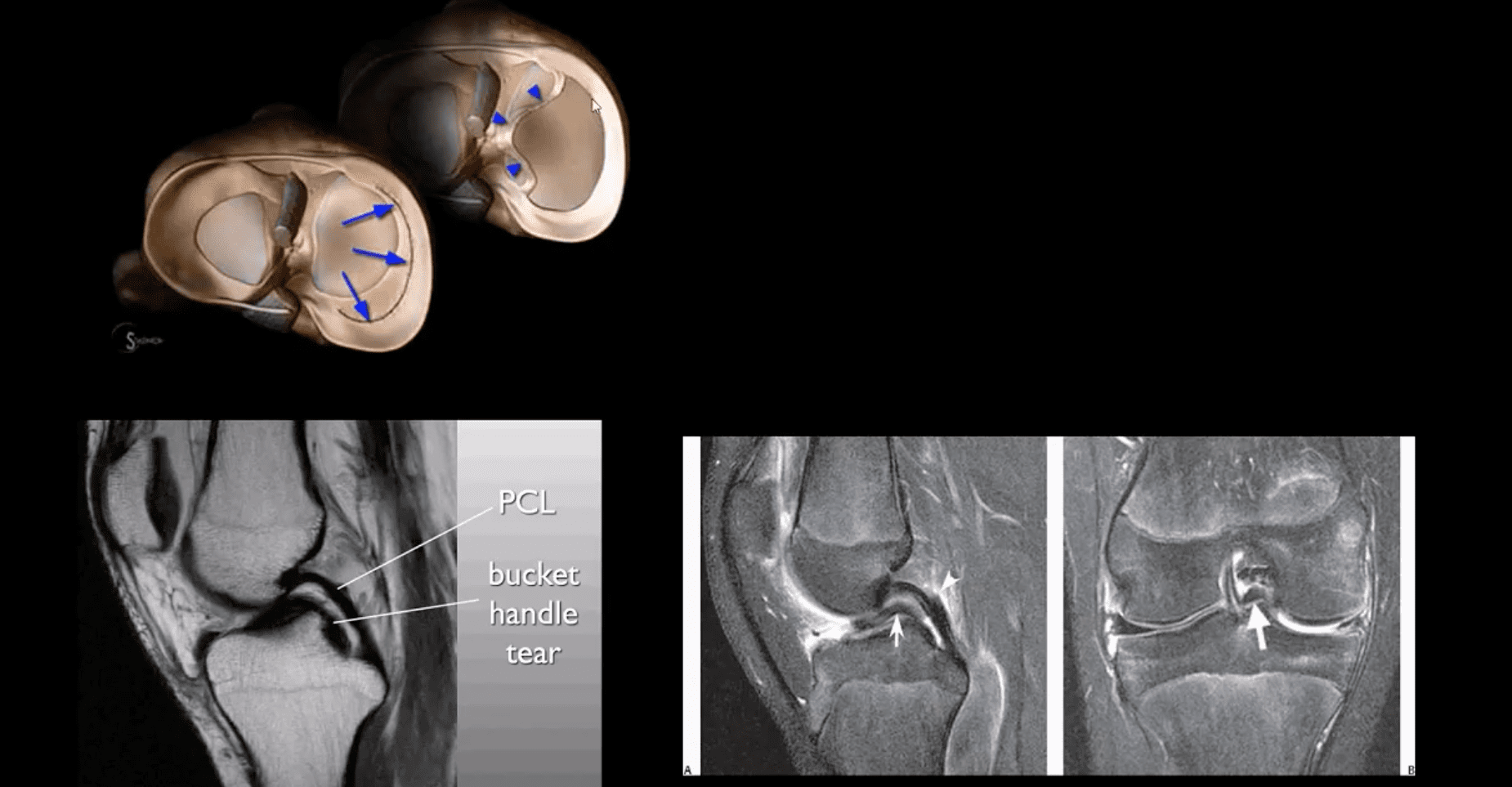
- Bucket handle tear are m/c in the medial meniscus esp. with acute ACL and MCL tear
- MRI signs; double PCL sign on sagittal slices
- Absent “bow-tie” sign and others
- Most cases require operative care
DDx From Meniscal Degeneration

- Occaisionally meniscal tears need to be DDx from meniscal degeneration which may also appear bright (high signal) on fluid sensitive MRI
- The simplest rule is that if there is a true meniscal tear aka Grade 3 lesion it always reaches/extends to the tibial plateau surface
The Role of MSK Ultrasound (US) in Knee Examination
- MSK US of the knee permits high resolution and dynamic imaging of primarily superficial anatomy (tendons, bursae, capsular ligaments)
- MSK US cannot adequately evaluate cruciate ligaments and the menisci in their entirety
- Thus MR imaging remains modality of choice
Potential Pathologies Successfully Evaluated by MSK US
- Patellar
tendionosis /patellar tendon rapture - Quadriceps tendon tear
- Prepatellar bursitis
- Infrapatellar bursitis
- Pes Anserine bursitis
- Popliteal cyst (Baker cyst)
- Inflammation/joint effusion with synovial thickening and hyperemia can be imaged with US (e.g. RA) especially with the addition of color power doppler
Patient Presented With Atraumatic Knee Pain & Swelling
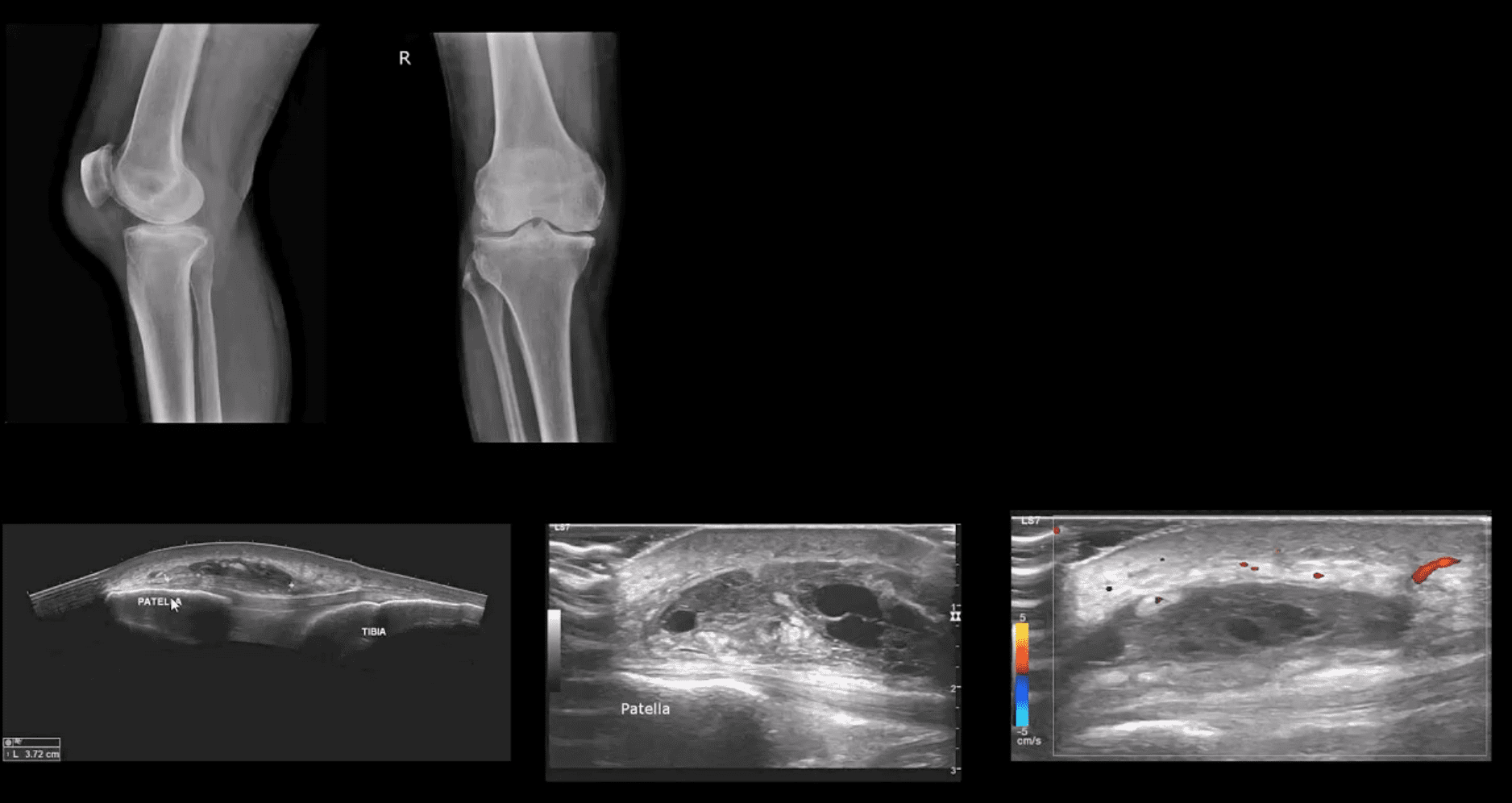
- Radiography revealed large soft tissue density within superficial pre-patella region along with mild-to-moderate OA
- MSK US demonstraded large septated heterogeneous fluid collection with mild positive Doppler activity on the periphery indicating inflammation d/t Dx of Superficial pre-patella bursitis
Long Axis US Images
- Note normal laterral meniscus and fibers of LCL (above bottom image) compared to
- Horizontal degenerative cleavage tear along with protrusion of lateral meniscus and LCL bulging (above top image)
- Major limitation: unable to visualize the entire meniscus and the ACL/PCL
- MRI referral is suggested
Rupture of Distal Tendon of Quadriceps
- Note rupture of distal tendon of the Quadriceps muscle presented as fiber separation and fluid (hypo to anechoic) fluid collection within the substance of the tendon
- Advantages of MSK US over MRI to evaluate superficial structures:
- Dynamic imaging
- Availability
- Cost-effective
- Patient’s preparation
- Disadvantages: limited depth of structures, inability to evaluated bone and cartilage etc.
Osteochondral Knee Injuries (OI)
- osteochondral knee injuries can occur in children 10-15 y.o presented as Osteochondritis Dissecance (OCD) and in mature skeleton m/c following hyperextension and rotation trauma particularly in ACL tear.
- OCD-typically develops from repeated forces in immature bone and affects m/c postero-lateral portion of the medial femoral condyle.
- OI in mature bone occurs m/c during ACL tears particularly affecting so-called terminal sulcus of the lateral femoral condyle at the junction of the weight-bearing portion opposed to tibial plateau an the part articulating with the patella
- Osteochondral injuries may potentially damage the articular cartilage causing secondary OA. Thus need to be evaluated surgically
- Imaging plays an important role and should begin with radiography often followed by MR imaging and orthopedic referral.
OCD Knee
- 95% associated with some trauma. Other etiology: ischemic bone necrosis especially in adults
- Other common location for osteochondral injuries: elbow (capitellum), talus
- 1st step: radiography may detect osteochondral fragment potentially attached or detached
- Location: posterior-lateral aspect of medial femoral condyle. Tunnel (intercondylar notch) view is crucial
- MRI: modality of choice >90% specificity and sensitivity. Crucial for further management. T1-low signal demarcating line with T2 high signal demarcating line that signifies detachment and unlikely healing. Refer to orthopedic surgeon
- Management: stable lesion esp. in younger children>off weight-bearing-heals in 50-75%
- Unstable lesion and older child or impending physeal closure>operative fixation.
Knee Trauma
Post Disclaimer
Professional Scope of Practice *
The information herein on "Knee Pain & Acute Trauma Diagnosis Imaging Part II | El Paso, TX" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Chiropractic Scientist wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.