How does your brain know when you are experiencing pain? How does it know the difference between the soft touch of a feather and a needle prick? And, how does that information get to your body in time to respond? How can acute pain become chronic pain? These aren’t simple answers, but with a small explanation about how the nervous system works, you need to have the ability to comprehend the basics before considering any type of treatment approach for chronic pain.
Your nervous system is made up of 2 main parts: the brain and the spinal cord, which unite to form the central nervous system; and both sensory and motor nerves, that form the peripheral nervous system. The names make it easy to picture: the brain and spinal cord are the hubs, whereas the sensory and motor nerves stretch out to provide access to all areas of the body. Put simply, sensory nerves send impulses about what is going on in our environment to the brain through the spinal cord. The brain sends data back into the motor nerves, which help us execute tasks. It is like using an extremely complicated inbox and outbox for everything. The purpose of the article below is to demonstrate the process by which the human nervous system processes chronic pain.
Table of Contents
Pain Processing in the Human Nervous System: A Selective Review of Nociceptive and Biobehavioral Pathways
Abstract
This selective review discusses the psychobiological mediation of nociception and pain. Summarizing literature from physiology and neuroscience, first an overview of the neuroanatomic and neurochemical systems underpinning pain perception and modulation is provided. Second, findings from psychological science are used to elucidate cognitive, emotional, and behavioral factors central to the pain experience. This review has implications for clinical practice with patients suffering from chronic pain, and provides strong rationale for assessing and treating pain from a biopsychosocial perspective.
Keywords: pain, nociception, neurobiology, autonomic, cognitive, affective
Introduction
Pain is a complex, biopsychosocial phenomenon that arises from the interaction of multiple neuroanatomic and neurochemical systems with a number of cognitive and affective processes. The International Association for the Study of Pain has offered the following definition of pain: “Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.â€[1] (p210) Thus, pain has sensory and affective components, as well as a cognitive component reflected in the anticipation of future harm. The purpose of the following review is to integrate the literature on the neurobiological pathways within the central, autonomic, and peripheral nervous systems that mediate pain processing, and discuss how psychological factors interact with physiology to modulate the experience of pain.
Functional Neuroanatomy and Neurochemistry of Pain
Pain Processing in the Nervous System
When noxious stimuli impinge upon the body from external or internal sources, information regarding the damaging impact of these stimuli on bodily tissues is transduced through neural pathways and transmitted through the peripheral nervous system to the central and autonomic nervous systems. This form of information processing is known as nociception. Nociception is the process by which information about actual tissue damage (or the potential for such damage, should the noxious stimulus continue to be applied) is relayed to the brain. Nociception is mediated by specialized receptors known as nociceptors that are attached to thin myelinated Aδ and unmyelinated C fibers, which terminate in the dorsal horn of the spine. Sufficiently intense mechanical stimulation (such as stretching, cutting, or pinching), intense warming of the skin, or exposure to noxious chemicals can activate nociceptors.[2] In turn, activation of nociceptors is modulated by inflammatory and bio-molecular influences in the local extracellular environment.[3] Although under most circumstances transmission of nociceptive information results in pain perception, many physicians and patients are unaware that nociception is dissociable from the experience of pain. In other words, nociception can occur in the absence of awareness of pain, and pain can occur in the absence of measurably noxious stimuli. This phenomenon is observable in instances of massive trauma (such as that which might be incurred by a motor vehicle accident) when victims exhibit a stoic painless state despite severe injury, and conversely, when individuals with functional pain syndromes report considerable anguish in spite of having no observable tissue damage.
In contrast, perception of pain occurs when stimulation of nociceptors is intense enough to activate Aδ fibers, resulting in a subjective experience of a sharp, prickling pain.[4] As stimulus strength increases, C fibers are recruited, and the individual experiences an intense, burning pain that continues after the cessation of the stimulus. These types of experiences occur during the two phases of pain perception that occur following an acute injury.[2] The first phase, which is not particularly intense, comes immediately after the painful stimulus and is known as fast pain. The second phase, known as slow pain, is more unpleasant, less discretely localized, and occurs after a longer delay.
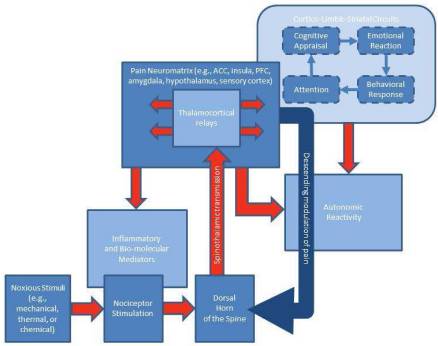
Activation of nociceptors is transduced along the axons of peripheral nerves which terminate in the dorsal horn of the spine. There, messages are relayed up the spinal cord and through the spinothalamic tract to output on the thalamus. In turn, the thalamus serves as the major “relay station†for sensory information to the cerebral cortex.[5] Nociceptive pathways terminate in discrete subdivisions of thalamic nuclei known as the ventral posterior lateral nucleus and the ventromedial nucleus.[6] From these nuclei, nociceptive information is relayed to various cortical and subcortical regions, including the amygdala, hypothalamus, periaqueductal grey, basal ganglia, and regions of cerebral cortex. Most notably, the insula and anterior cingulate cortex are consistently activated when nociceptors are stimulated by noxious stimuli, and activation in these brain regions is associated with the subjective experience of pain.[7] In turn, these integrated thalamocortical and corticolimbic structures, which collectively have been termed the pain “neuromatrix,†process somatosensory input and output neural impulses which influence nociception and pain perception.[8]
Neurochemistry of Pain
Nociception is mediated by the function of numerous intra- and extra-cellular molecular messengers involved in signal transduction in the peripheral and central nervous systems. All nociceptors, when activated by the requisite mechanical, thermal, or chemical stimulus, transmit information via the excitatory neurotransmitter glutamate.[9] In addition, inflammatory mediators are secreted at site of the original injury to stimulate nociceptor activation. This “inflammatory soup†is comprised of chemicals such as peptides (e.g., bradykinin), neurotransmitters (e.g., serotonin), lipids (e.g., prostaglandins), and neurotrophins (e.g., NGF). The presence of these molecules excites nociceptors or lowers their activation threshold, resulting in the transmission of afferent signals to the dorsal horn of the spinal cord as well as initiating neurogenic inflammation.[3] Neurogenic inflammation is the process by which active nociceptors release neurotransmitters such as substance P from the peripheral terminal to induce vasodilation, leak proteins and fluids into the extracellular space near the terminal end of the nociceptor, and stimulate immune cells which contribute to the inflammatory soup. As a result of these neurochemical changes in the local environment of nociceptors, the activation of Aδ and C fibers increases, and peripheral sensitization occurs.[10]
In turn, nociceptive signal transduction up the spinothalamic tract results in elevated release of norepinephrine from the locus coeruleus neurons projecting to thalamus, which in turn relays nociceptive information to somatosensory cortex, hypothalamus, and hippocampus.[11,12] As such, norepinephrine modulates the “gain†of nociceptive information as it is relayed for processing in other cortical and subcortical brain regions. Concomitantly, opioid receptors in the peripheral and central nervous systems (e.g., those in neurons of the dorsal horn of the spine and the periaqueductal grey in the brain) result in inhibition of pain processing and analgesia when stimulated by opiates or endogenous opioids like endorphin, enkephalin, or dynorphin.[13] The secretion of endogenous opioids is largely governed by the descending modulatory pain system.[14] The neurotransmitter GABA is also involved in the central modulation of pain processing, by augmenting descending inhibition of spinal nociceptive neurons.[15] A host of other neurochemicals are also involved in pain perception; the neurochemistry of nociception and central-peripheral pain modulation is extremely complex.
Descending Central Modulation of Pain
The brain does not passively receive pain information from the body, but instead actively regulates sensory transmission by exerting influences on the spinal dorsal horn via descending projections from the medulla.[16] In their seminal Gate Control theory of pain, Melzack and Wall proposed that the substantia gelatinosa of the dorsal horn gates the perception of noxious stimuli by integrating upstream afferent signals from the peripheral nervous system with downstream modulation from the brain.[17] Interneurons in the dorsal horn can inhibit and potentiate impulses ascending to higher brain centers, and thus they provide a site where the central nervous system controls impulse transmission into consciousness.
The descending pain modulatory system exerts influences on nociceptive input from the spinal cord. This network of cortical, subcortical, and brainstem structures includes prefrontal cortex, anterior cingulate cortex, insula, amygdala, hypothalamus, periaqueductal grey, rostral ventromedial medulla, and dorsolateral pons/tegmentum.7 The coordinated activity of these brain structures modulates nociceptive signals via descending projections to the spinal dorsal horn. By virtue of the somatotopic organization of these descending connections, the central nervous system can selectively control signal transmission from specific parts of the body.
The descending pain modulatory system has both anti- and pro-nociceptive effects. Classically, the descending pain modulatory system has been construed as the means by which the central nervous system inhibits nociceptive signals at the spinal outputs.[16] In a crucial early demonstration, Reynolds observed that direct electrical stimulation of the periaqueductal grey could produce dramatic analgesic effects as evidenced by the ability to undergo major surgery without pain.[18] Yet, this brain system can also facilitate nociception. For instance, projections from the periaqueductal grey to the rostral ventromedial medulla have been shown to enhance spinal transmission of nociceptive information from peripheral nociceptors.[19]
Central modulation of pain may have been a conserved across human evolution due to its potentially adaptive effects on survival. For instance, in situations of serious mortal threat (for example, in the face of war and civil accidents, or more primordially, when being attacked by a vicious animal), suppression of pain might enable a severely-injured individual to continue intense physical activity such as fleeing from danger or fighting a deadly opponent. Yet, the neurobiological linkages between the brain, the spinothalamic tract, the dorsal horn, and the peripheral nerves also provide a physiological pathway by which negative emotions and stress can amplify and prolong pain, causing functional interference and considerable suffering.
Cognitive, Affective, Psychophysiological, and Behavioral Processes in Pain Perception and Regulation
In addition to the somatosensory elements of pain-processing described above, cognitive and emotional factors are implicit within the definition of pain offered by the International Association for the Study of Pain. Pain perception involves a number of psychological processes, including attentional orienting to the painful sensation and its source, cognitive appraisal of the meaning of the sensation, and the subsequent emotional, psychophysiological, and behavioral reaction, which then feedback to influence pain perception (see Figure 1). Each of these processes will be detailed below.
Attention to Chronic Pain
In the brain, attention allows salient subsets of data to gain preeminence in the competitive processing of neural networks at the expense of other subsets of data.[20] The goal-relevance of a stimulus guides attention to select and distinguish it from the environmental matrix in which it is embedded.[21] Thus, attended stimuli receive preferential information processing and are likely to govern behavior. In this sense, attention allows for the evaluation of salient stimuli, and facilitates execution of approach behaviors in response to appetitive stimuli or avoidance behaviors in response to aversive ones. Thus, depending on its salience to the survival of the organism, the object of attention elicits the motivation to approach or avoid, while the resultant emotional state, as the manifestation of approach or avoidance motivations, tunes and directs attention.[22,23] By virtue of its significance for health and well-being, pain automatically and involuntarily attracts attention.[24,25] Yet pain experience varies according to the locus of attention; when attention is focused on pain, it is perceived as more intense,[26] and whereas when attention is distracted from pain, it is perceived as less intense.[27]
Attentional modulation of pain experience correlates with changes in activation of the pain neuromatrix; for instance, attentional distraction reduces pain-related activations in somatosensory cortices, thalamus, and insula, among other brain regions.[7] Concomitantly, distraction results in strong brain activations in prefrontal cortex, anterior cingulate cortex, and periaqueductal grey, suggesting an overlap and interaction between brain systems involved in attentional modulation of pain and the descending pain modulatory system.[28] In contrast, attentional hypervigilance for pain, a high degree of monitoring internal and external stimuli that is often observed among persons with chronic pain,[29] amplifies pain intensity and is associated with the interpretation of harmless sensations (like moderate levels of pressure) as painfully unpleasant.[30,31]
Cognitive Appraisal of Pain
Pain involves a process of cognitive appraisal, whereby the individual consciously or unconsciously evaluates the meaning of sensory signals emanating from the body to determine the extent to which they signify the presence of an actual or potential harm. This evaluation is decidedly subjective. For instance, experienced weightlifters or runners typically construe the “burn†they feels in their muscles as pleasurable and indicative of increasing strength and endurance; in contrast, a novice might view the same sensation as signaling that damage had occurred. The inherent variability of cognitive appraisal of pain may stem from the neurobiological dissociation between the sensory and affective aspects of the pain experience; change in pain intensity results in altered activation of somatosensory cortex, whereas change in pain unpleasantness results in altered activation of the anterior cingulate cortex.[32,33] Thus, a sensory signal originating from the muscles of lower back might be perceived as a warmth and tightness, or viewed as a terrible agony, in spite of the stimulus intensity being held constant. The manner in which the bodily sensation is appraised may in turn influence whether it is experienced as unpleasant pain or not.[34]
The extent to which a given bodily sensation is interpreted as threatening is in part dependent on whether or not the individual believes he or she is able to cope with that sensation. If, during this complex cognitive process of appraisal, available coping resources are deemed sufficient to deal with the sensation, then pain can be perceived as controllable. Pain intensity is reduced when pain is perceived to be controllable, whether or not the individual acts to control the pain. Ventrolateral prefrontal cortex activation is positively associated with the extent to which pain is viewed as controllable and negatively correlated with subjective pain intensity. This brain region is implicated in emotion regulation efforts, such as when threatening stimuli are reappraised to be benign.[35,36] Concomitantly, reinterpreting pain as a harmless sensation (e.g., warmth or tightness) predicts higher perceived control over pain,[37] and psychological interventions have been shown to reduce pain severity by increasing reinterpretation of pain sensations as innocuous sensory information.[38] In contrast, pain catastrophizing (i.e., viewing pain as overwhelming and uncontrollable) is associated with greater pain intensity irrespective of the extent of physical impairment[39] and prospectively predicts the development of low back pain.[40]
Emotional and Psychophysiological Reactions to Chronic Pain
The aversive nature of pain elicits a powerful emotional reaction that feeds back to modulate pain perception. Pain often results in feelings of anger, sadness, and fear depending on the how the pain is cognitively appraised. For instance, the belief “It’s not fair that I have to live with this pain†is likely to lead to anger, whereas the belief “My life is hopeless now that I have this pain†will likely result in sadness. Fear is a common reaction to pain when individuals interpret the sensations from the body as indicating the presence of serious threat.
These emotions are coupled with autonomic, endocrine, and immune responses which may amplify pain through a number of psychophysiological pathways. For example, pain induction significantly elevates sympathetic nervous system activity, marked by increased anxiety, heart rate, and galvanic skin response.[41] Furthermore, negative emotions and stress increase contraction of muscle tissue; elevated electromyographic activity occurs in the muscles of the back and neck under conditions of stress and negative affect and is perceived as painful spasms.[42,43] This sympathoexcitatory reaction coupled with emotions like anger and fear may reflect an evolutionarily conserved, active coping response to escape the painful stimulus. Yet negative emotional states intensify pain intensity, pain unpleasantness, and pain-induced cardiovascular autonomic responses, while reducing the sense of perceived control over pain.[44] Stress and negative emotions like anger and fear may temporarily dampen pain via norepinephrine release, but when the sympathetic “fight or flight†response is prolonged it can increase blood flow to the muscle and increase muscle tension which may aggravate the original injury.[45] Alternatively, pain inputs from the viscera and muscles may stimulate cardiac vagal premotor neurons, leading to hypotension, bradycardia, and hyporeactivity to the environment – a pattern of autonomic response that corresponds with passive pain coping and depressed affect.[46] In addition to autonomic reactivity, pro-inflammatory cytokines and the stress hormone cortisol are released during the experience of negative emotion; these bio-molecular factors enhance nociception, facilitate processing of aversive information in the brain, and when their release is chronic or recurrent, may cause or exacerbate tissue damage.[8,47,48]
Moreover, negative emotions are associated with increased activation in the amygdala, anterior cingulate cortex, and anterior insula – these brain structures not only mediate the processing of emotions, but are also important nodes of the pain neuromatrix that tune attention toward pain, intensify pain unpleasantness, and amplify interoception (the sense of the physical condition of the body).[49,50] Thus, when individuals experience negative emotions like anger or fear as a result of pain or other emotionally salient stimuli, the heightened neural processing of threat in affective brain circuits primes the subsequent perception of pain[51,52] and increases the likelihood that sensations from within the body will be interpreted as painful.[53–55] The fear of pain, a clinical feature of chronic pain patients, is associated with hypervigilance for and sustained attention to pain-related stimuli.[56] Thus, negative emotions bias attention toward pain, which then increase its unpleasantness. In addition, negative emotions and stress impair prefrontal cortex function, which may reduce the ability to regulate pain using higher order cognitive strategies like reappraisal or viewing the pain as controllable and surmountable.[57,58] Thus, anger, sadness, and fear may result from acute or chronic pain and in turn feedback into the bio-behavioral processes that influence pain perception to exacerbate anguish and suffering.
Behavioral Reactions to Pain
Pain is not only a sensory, cognitive, and emotional experience, but also involves behavioral reactions that may alleviate, exacerbate, or prolong pain experience. Typical pain behaviors in low back pain include grimacing, rubbing, bracing, guarded movement, and sighing.[59] These behaviors facilitate the communication of pain and exert social influences that may have vicarious gain for the individual suffering from pain; such benefits include sympathy, acts of kindness and generosity, tolerance, lowered expectations, and social bonding, among others.[60] In addition, guarding or avoidance of activities associated with pain may be negatively reinforcing by virtue of the temporary alleviation of pain experience.[61] The fact that these avoidant behaviors decrease the occurrence of pain results in increasing use of avoidance as a coping strategy. Yet, greater use of avoidance as a result of fear of pain predicts higher levels of functional disability.[62] It is not merely that persons with greater pain-related disability engage in more avoidant behaviors, but rather studies indicate that avoidant behavior and beliefs are a precursor to disability.[63–65] Avoidance contributes to negative clinical outcomes in patients with chronic low back pain. Fear-avoidance of pain influences physical impairment and is more strongly associated with functional disability than pain severity.[66–68] In contrast, progressive increase in activity through exercise has been shown to result in significant benefits in pain, disability, physical impairment, and psychological distress for low back pain patients.[69] In light of the robust relation between coping behaviors and pain, behavioral and psychosocial interventions hold great promise in reducing pain intensity and pain-related functional disability in chronic pain conditions such as low back pain.[70]

Dr. Alex Jimenez’s Insight
Different sensory nerve fibers respond to different stimulations and produce different chemical reactions which determine how different sensations are interpreted. Special pain receptors, known as nociceptors, activate when there has been trauma from an injury or even through potential damage to the human body. This impulse, immediately sends a signal through the nerve and into the spinal cord, eventually reaching all the way to the brain. The role of the spinal cord in pain perception is also to simultaneously direct impulses to the brain and back down the spinal cord to the region of the injury. These are referred to as reflexes. However, the pain signal still needs to continue to the brain so it can respond accordingly. The brain will assess the type of pain and where it came from, triggering a healing response as well as a variety of other bodily responses to address the pain signal effectively. In the case of chronic pain, pain perception may not be working accordingly along any of the pathways mentioned above. Treatment can help improve chronic pain as well as manage the painful symptoms.
Conclusion
The foregoing review attests to the multidimensionality of pain. Pain is a biopsychosocial experience that goes well beyond mere nociception. In this regard, identification of the physical pathology at the site of injury is necessary but not sufficient to explicate the complex process by which somatosensory information is transformed into the physiological, cognitive, affective, and behavioral response labeled as pain. Indeed, in the case of chronic low back pain, the magnitude of tissue damage may be out of proportion to the reported pain experience, there may be no remaining structural impairment, and physical signs that have a predominantly nonorganic basis are likely to be present.[71,72] In this and other chronic conditions, to consider such pain as malingering or somatization would be to grossly oversimplify the matter. Pain, whether linked with injured tissue, inflammation, or functional impairment, is mediated by processing in the nervous system. In this sense, all pain is physical. Yet, regardless of its source, pain may result in hypervigilance, threat appraisals, emotional reactions, and avoidant behavior. So in this sense, all pain is psychological. Our nomenclature and nosology struggle to categorize the pain experience, but in the brain, all such categories are moot. Pain is fundamentally and quintessentially a psychophysiological phenomenon.
Key Points
- Pain is a biopsychosocial experience that goes well beyond mere nociception. In this regard, identification of the physical pathology at the site of injury is necessary but not sufficient to explicate the complex process by which somatosensory information is transformed into the physiological, cognitive, affective, and behavioral response labeled as pain
- In the case of chronic low back pain, the magnitude of tissue damage may be out of proportion to the reported pain experience, there may be no remaining structural impairment, and physical signs that have a predominantly nonorganic basis are likely to be present.
- Pain, whether linked with injured tissue, inflammation, or functional impairment, is mediated by processing in the nervous system. In this sense, all pain is physical. Yet, regardless of its source, pain may result in hypervigilance, threat appraisals, emotional reactions, and avoidant behavior. So in this sense, all pain is psychological.
- Our nomenclature and nosology struggle to categorize the pain experience, but in the brain, all such categories are moot. Pain is fundamentally and quintessentially a psychophysiological phenomenon.
Acknowledgements
ELG was supported by grant DA032517 from the National Institute on Drug Abuse in the preparation of this manuscript.
Footnotes
Ncbi.nlm.nih.gov/pmc/articles/PMC3438523/
Plants as Medicine: Are Cannabinoids the Next Breakthrough in Plant Medicine?
If you’ve ever eaten a carrot, then you have consumed a cannabinoid. Most people associate cannabinoids with marijuana. The most commonly recognized cannabinoid is tetrahydrocannabinol, or THC, the chemical in marijuana that causes feelings of euphoria. Until recently, scientists had identified cannabinoids just in the cannabis plant, commonly called hemp or marijuana. Current research, however, has found cannabinoids in several plants, including clove, black pepper, Echinacea, ginseng and broccoli as well as carrots. No matter how many carrots you crunch, however, they will not get you too high. But understanding how the cannabinoids in different plants affect the human body may contribute to important health discoveries.
Plants as Medicine
Some of the most appreciated modern drugs were developed by analyzing plants used in conventional medicine. Researching the chemicals in these plants led to the discovery of life-saving drugs and furthered our knowledge of how the human body works. For instance, the foxglove plant introduced us to digoxin and digitoxin, two important heart medications.[1] As well as the Pacific yew contains paclitaxel, which can be used in the treatment of many cancers.[1] Throughout history, people have been especially adept at finding plants which either increase pleasure or reduce pain. Caffeine from tea and tea provides energy and keeps us awake, while smoking from tobacco is believed to be concurrently stimulating and relaxing, likely explaining why tobacco remains popular despite the known health risks of smoking.[2]
Several sorts of pain-relieving drugs originated with plants:
Opiates
By analyzing opium from the poppy plant, scientists discovered opiate receptors in the human body and their role in pain control, which led to the development of morphine, codeine, and other opiate drugs and/or medications.[3]
Aspirin
As far back as ancient Egypt, health practitioners used tea made from the willow tree to decrease pain and fever. It took tens of thousands of years for scientists to find and isolate the active chemical, or the fatty acid, which led to the discovery of aspirin and from there, finding insights into the processes involved with inflammation.[4]
Anesthetics
The leaves of the coca plant were used from the ancient Incan Empire from South America to deal with headaches, wounds and fractures. Coca eventually yielded the drug cocaine, which is a drug of misuse and abuse, but also an effective anesthetic. Recognizing how cocaine blocked pain led to the development of common anesthetics such as lidocaine, famous for making invasive dental procedures more comfortable.[5]
Cannabis and Human Health
Such as other medicinal plants, the cannabis species has been used for centuries. A Chinese text from the year AD 1 records the usage of hemp to treat more than 100 ailments dating back to 2737 BC.[6] Afterwards, the flowering tops of the Cannabis plant began to be cultivated for their psychoactive properties, while a different selection of the plant was increased as industrial hemp to be used in producing garments, paper, biofuels, foods, and other products.
Because of the controversy surrounding marijuana as a recreational drug, researchers have not been able to readily study the effects of the many non-THC ingredients in Cannabis. Although THC was identified from the 1940s, it was not until 50 years after that studies demonstrated that individuals, and nearly all animals, have an inner system of cannabinoid receptors. What is more, we really make cannabinoids in our bodies, known as endocannabinoids, that act on these receptors.[7]
This physiological system is called the endocannabinoid system, or ECS, and new science appears almost daily about its function in human health. The ECS is involved in multiple functions, such as pain feeling, hunger, memory, and disposition. If you’ve ever stubbed your toe, digested an apple, then forgotten a password, or happily smile, then your ECS was involved, little did you know.
The discovery of the ECS gave science and medicine a whole new outlook about the organic compounds being identified in Cannabis. Researchers started referring to these chemicals as phytocannabinoids, from the work “phyto” for plant. More than 80 phytocannabinoids have been found in hemp and marijuana. THC is only one of many compounds being studied for the advantages they can provide.[8]
Past Cannabis and THC
Now that many different crops are known to contain chemicals that influence the ECS, phytocannabinoids are no longer just associated with the cannabis plant.[9] Chances are you have some source of phytocannabinoids in your diet right now. But it might be a small quantity, rather than all of phytocannabinoids interact strongly with the ECS.
What exactly do we know up to now? Current research shows that a number of the phytocannabinoids in hemp, clove, and black pepper can encourage the ECS to promote relaxation, decrease nerve distress, and improve digestive health. As these compounds don’t possess the mind-altering effects of THC, more individuals are likely to flip to phytocannabinoids to acquire their health benefits without having high.[10] Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
1. Merskey H, Bogduk N. Classification of chronic pain, IASP Task Force on Taxonomy. IASP Press; Seattle: 1994.
2. Brodal P. The central nervous system: structure and function. Oxford Univ Pr; 2010.
3. Loeser JD, Melzack R. Pain: an overview. The Lancet. 1999;353(9164):1607–1609. [PubMed]
4. Bishop GH, Landau WM. Evidence for a Double Peripheral Pathway for Pain. Science. 1958;128(3326):712–713. [PubMed]
5. Sherman SM, Guillery R. Functional organization of thalamocortical relays. Journal of Neurophysiology. 1996;76(3):1367. [PubMed]
6. Willis W, Westlund K. Neuroanatomy of the pain system and of the pathways that modulate pain. Journal of Clinical Neurophysiology. 1997;14(1):2. [PubMed]
7. Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron. 2007;55(3):377–391. [PubMed]
8. Melzack R. From the gate to the neuromatrix. Pain. 1999;82:S121–S126. [PubMed]
9. Petrenko AB, Yamakura T, Baba H, Shimoji K. The role of N-methyl-D-aspartate (NMDA) receptors in pain: a review. Anesthesia & Analgesia. 2003;97(4):1108. [PubMed]
10. JM B. The neurobiology of pain. The Lancet. 1999;353(9164):1610–1615. [PubMed]
11. Yaksh TL. Pharmacology of spinal adrenergic systems which modulate spinal nociceptive processing. Pharmacology Biochemistry and Behavior. 1985;22(5):845–858. [PubMed]
12. Voisin DL, Guy N, Chalus M, Dallel R. Nociceptive stimulation activates locus coeruleus neurones projecting to the somatosensory thalamus in the rat. The Journal of Physiology. 2005;566(3):929–937. [PMC free article] [PubMed]
13. Yaksh TL. Opioid receptor systems and the endorphins: a review of their spinal organization. Journal of neurosurgery. 1987;67(2):157–176. [PubMed]
14. Basbaum AI, Fields HL. Endogenous pain control systems: brainstem spinal pathways and endorphin circuitry. Annual Review of Neuroscience. 1984;7(1):309–338. [PubMed]
15. Jasmin L, Rabkin SD, Granato A, et al. Analgesia and hyperalgesia from GABA-mediated modulation of the cerebral cortex. Nature. 2003;424(6946):316–320. [PubMed]
16. Heinricher M, Tavares I, Leith J, Lumb B. Descending control of nociception: Specificity, recruitment and plasticity. Brain research reviews. 2009;60(1):214–225. [PMC free article] [PubMed]
17. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(699):971–979. others. [PubMed]
18. Reynolds DV. Surgery in the rat during electrical analgesia induced by focal brain stimulation. Science. 1969;164(3878):444. [PubMed]
19. Carlson JD, Maire JJ, Martenson ME, Heinricher MM. Sensitization of pain-modulating neurons in the rostral ventromedial medulla after peripheral nerve injury. The Journal of Neuroscience. 2007;27(48):13222. [PubMed]
20. Desimone R, Duncan J. Neural mechanisms of selective visual attention. Annu Rev Neurosci. 1995;18:193–222. [PubMed]
21. Corbetta M, Shulman GL. Control of goal-directed and stimulus-driven attention in the brain. Nature Reviews: Neuroscience. 2002;3:201–215. [PubMed]
22. Friedman RS, F\örster J. Implicit affective cues and attentional tuning: An integrative review. Psychological bulletin. 2010;136(5):875. [PMC free article] [PubMed]
23. Lang PJ, Bradley MM. Emotion and the motivational brain. Biol Psychol. 2011;84:437–50. [PMC free article] [PubMed]
24. Legrain V, Perchet C, GarcÃa-Larrea L. Involuntary orienting of attention to nociceptive events: neural and behavioral signatures. Journal of neurophysiology. 2009;102(4):2423. [PubMed]
25. Eccleston C, Crombez G. Pain demands attention: A cognitive–affective model of the interruptive function of pain. Psychological Bulletin. 1999;125(3):356. [PubMed]
26. Quevedo AS, Coghill RC. Attentional modulation of spatial integration of pain: evidence for dynamic spatial tuning. The Journal of Neuroscience. 2007;27(43):11635–11640. [PubMed]
27. Terkelsen AJ, Andersen OK, MU00F8lgaard H, Hansen J, Jensen T. Mental stress inhibits pain perception and heart rate variability but not a nociceptive withdrawal reflex. Acta physiologica scandinavica. 2004;180(4):405–414. [PubMed]
28. Wiech K, Ploner M, Tracey I. Neurocognitive aspects of pain perception. Trends in Cognitive Sciences. 2008;12(8):306–313. [PubMed]
29. Schoth DE, Nunes VD, Liossi C. Attentional bias towards pain-related information in chronic pain; a meta-analysis of visual-probe investigations. Clinical Psychology Review. 2011 [PubMed]
30. Hollins M, Harper D, Gallagher S, et al. Perceived intensity and unpleasantness of cutaneous and auditory stimuli: An evaluation of the generalized hypervigilance hypothesis. PAIN. 2009;141(3):215–221. [PMC free article] [PubMed]
31. Rollman GB. Perspectives on hypervigilance. PAIN. 2009;141(3):183–184. [PubMed]
32. Rainville P, Carrier B, Hofbauer RK, Bushnell MC, Duncan GH. Dissociation of sensory and affective dimensions of pain using hypnotic modulation. Pain. 1999;82:159–71. [PubMed]
33. Rainville P, Duncan GH, Price DD, Carrier B, Bushnell MC. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science. 1997;277:968–71. [PubMed]
34. Price DD. Central neural mechanisms that interrelate sensory and affective dimensions of pain. Mol Interv. 2002;2(6):392–403. [PubMed]
35. Ochsner KN, Gross JJ. The cognitive control of emotion. Trends in Cognitive Science. 2005;9:242–9. [PubMed]
36. Kalisch R. The functional neuroanatomy of reappraisal: time matters. Neurosci Biobehav Rev. 2009;33:1215–26. [PubMed]
37. Haythornthwaite JA, Menefee LA, Heinberg LJ, Clark MR. Pain coping strategies predict perceived control over pain. Pain. 1998;77(1):33–39. [PubMed]
38. Garland EL, Gaylord SA, Palsson O, et al. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. Journal of Behavioral Medicine. 2011:1–12. [PMC free article] [PubMed]
39. Severeijns R, Vlaeyen JWS, van den Hout MA, Weber WEJ. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. The Clinical journal of pain. 2001;17(2):165. [PubMed]
40. Picavet HSJ, Vlaeyen JWS, Schouten JSAG. Pain Catastrophizing and Kinesiophobia: Predictors of Chronic Low Back Pain. American Journal of Epidemiology. 2002;156(11):1028–1034. [PubMed]
41. Tousignant-Laflamme Y, Marchand S. Sex differences in cardiac and autonomic response to clinical and experimental pain in LBP patients. European Journal of Pain. 2006;10(7):603–614. [PubMed]
42. Flor H, Turk DC, Birbaumer N. Assessment of stress-related psychophysiological reactions in chronic back pain patients. Journal of Consulting and Clinical Psychology. 1985;53(3):354–364. Journal of Consulting and Clinical Psychology. [PubMed]
43. Lundberg U, Dohns IE, Melin B, et al. Psychophysiological stress responses, muscle tension, and neck and shoulder pain among supermarket cashiers. Journal of Occupational Health Psychology. 1999;4(3):245–255. Journal of Occupational Health Psychology. [PubMed]
44. Rainville P, Bao QVH, Chrétien P. Pain-related emotions modulate experimental pain perception and autonomic responses. Pain. 2005;118(3):306–318. [PubMed]
45. Cannon WB. Organization of physiological homeostasis. Physiology Review. 1929;9
46. Benarroch EE. Pain-autonomic interactions. Neurological Sciences. 2006;27(S2):s130–s133. [PubMed]
47. Sommer C, Kress M. Recent findings on how proinflammatory cytokines cause pain: peripheral mechanisms in inflammatory and neuropathic hyperalgesia. Neuroscience Letters. 2004;361(1–3):184–187. [PubMed]
48. Chapman CR, Tuckett RP, Song CW. Pain and stress in a systems perspective: reciprocal neural, endocrine, and immune interactions. The Journal of Pain. 2008;9(2):122–145. [PMC free article] [PubMed]
49. Craig AD. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol. 2003;13:500–5. [PubMed]
50. Wiech K, Tracey I. The influence of negative emotions on pain: behavioral effects and neural mechanisms. Neuroimage. 2009;47:987–94. [PubMed]
51. de Wied M, Verbaten MN. Affective pictures processing, attention, and pain tolerance. Pain. 2001;90(1-2):163–172. [PubMed]
52. Kirwilliam SS, Derbyshire SWG. Increased bias to report heat or pain following emotional priming of pain-related fear. PAIN. 2008;137(1):60–65. [PubMed]
53. Bogaerts K, Janssens T, De Peuter S, Van Diest I, Van den Bergh O. Negative affective pictures can elicit physical symptoms in high habitual symptom reporters. Psychology & Health. 2009;25(6):685–698. [PubMed]
54. Panerai AE. Pain emotion and homeostasis. Neurological Sciences. 2011;32(S1):27–29. [PubMed]
55. Strigo IA, Simmons AN, Matthews SC, Craig AD (Bud), Paulus MP. Increased Affective Bias Revealed Using Experimental Graded Heat Stimuli in Young Depressed Adults: Evidence of “Emotional Allodynia.†Psychosomatic Medicine. 2008;70(3):338–344. [PMC free article] [PubMed]
56. Keogh E, Ellery D, Hunt C, Hannent I. Selective attentional bias for pain-related stimuli amongst pain fearful individuals. Pain. 2001;91:91–100. [PubMed]
57. Arnsten AFT. Stress signalling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience. 2009;10(6):410–422. [PMC free article] [PubMed]
58. Lawrence JM, Hoeft F, Sheau KE, Mackey SC. Strategy-dependent Dissociation of the Neural Correlates Involved in Pain Modulation. Anesthesiology. 2011;115(4):844–851. [PMC free article] [PubMed]
59. Keefe FJ, Wilkins RH, Cook WA. Direct observation of pain behavior in low back pain patients during physical examination. Pain. 1984;20(1):59–68. [PubMed]
60. Hadjistavropoulos T, Craig KD, Fuchs-Lacelle S. Social influences and the communication of pain. Pain: psychological perspectives. 2004:87–112.
61. Turk DC, Flor H. Pain> pain behaviors: the utility and limitations of the pain behavior construct. Pain. 1987;31(3):277–295. [PubMed]
62. Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332. [PubMed]
63. Linton SJ, Buer N, Vlaeyen J, Hellsing AL. Are fear-avoidance beliefs related to the inception of an episode of back pain? A prospective study. Psychology and Health. 2000;14(6):1051–1059. [PubMed]
64. Buer N, Linton SJ. Fear-avoidance beliefs and catastrophizing: occurrence and risk factor in back pain and ADL in the general population. Pain. 2002;99(3):485–491. [PubMed]
65. Klenerman L, Slade P, Stanley I, et al. The prediction of chronicity in patients with an acute attack of low back pain in a general practice setting. Spine. 1995;20(4):478. [PubMed]
66. Crombez G, Vlaeyen JWS, Heuts PHTG, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80(1-2):329–339. [PubMed]
67. Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. [PubMed]
68. Vlaeyen JWS, Kole-Snijders AMJ, Boeren RGB, Van Eek H. Fear of movement/(re) injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62(3):363–372. [PubMed]
69. Waddell G. Biopsychosocial analysis of low back pain. Baillière’s clinical rheumatology. 1992;6(3):523. others. [PubMed]
70. Hoffman BM, Papas RK, Chatkoff DK, Kerns RD. Meta-analysis of psychological interventions for chronic low back pain. Health psychology. 2007;26(1):1. [PubMed]
71. Waddell G, McCulloch J, Kummel E, Venner RM. Nonorganic physical signs in low-back pain. Spine. 1980;5(2):117–125. [PubMed]
72. Waddell G. Low back pain: a twentieth century health care enigma. Spine. 1996;21(24):2820. [PubMed]
Additional Topics: Back Pain
Back pain is one of the most prevalent causes for disability and missed days at work worldwide. As a matter of fact, back pain has been attributed as the second most common reason for doctor office visits, outnumbered only by upper-respiratory infections. Approximately 80 percent of the population will experience some type of back pain at least once throughout their life. The spine is a complex structure made up of bones, joints, ligaments and muscles, among other soft tissues. Because of this, injuries and/or aggravated conditions, such as herniated discs, can eventually lead to symptoms of back pain. Sports injuries or automobile accident injuries are often the most frequent cause of back pain, however, sometimes the simplest of movements can have painful results. Fortunately, alternative treatment options, such as chiropractic care, can help ease back pain through the use of spinal adjustments and manual manipulations, ultimately improving pain relief.

EXTRA IMPORTANT TOPIC: Lower Back Pain Management
MORE TOPICS: EXTRA EXTRA: Chronic Pain Care Center
Post Disclaimer
Professional Scope of Practice *
The information herein on "How the Nervous System Processes Chronic Pain" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card






 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.