Table of Contents
Hidden Signs of Traumatic Brain Injury (TBI): How Thorough History-Taking and Integrative Care Catch What Others Miss

Traumatic brain injury (TBI), including concussions, often remains undetected. There might be only internal injuries, not external ones. Instead, the clues are subtle: trouble focusing at work, new irritability with family, a strange change in taste or smell, headaches that won’t quit, or clumsy balance on stairs. Because these signs don’t always appear on a basic exam, TBI can be easy to overlook without a complete history and the right questions (Mayo Clinic, 2021; Hanscom Air Force Base, 2017). Mayo Clinic+1
This article explains how chiropractors and nurse practitioners (NPs) can work together to spot these hidden injuries and guide recovery. You’ll learn common symptom patterns, why they get missed, and how an integrative plan—spine and soft-tissue care, graded exercise, and medical support for sleep, mood, and metabolism—helps protect both the neurological and musculoskeletal systems after TBI (Figueiredo et al., 2024; Riva et al., 2010; Salsbury et al., 2018). MDPI+2PMC+2
We also include a practical list of diagnostic tests and instruments, ordered from the simplest to the most advanced, so patients and families know what to expect and when to escalate care (Mayo Clinic, 2021; Denver Chiropractic, 2018; Jimenez, 2016). Mayo Clinic+2Denver Integrated Spine Center+2
Why a Thorough History Catches Hidden TBIs
A careful interview often reveals what scans can’t. Providers should ask about how the injury occurred, whether there was loss of consciousness, changes in speech, coordination, or alertness, and whether there was head/neck acceleration, such as whiplash (Mayo Clinic, 2021). In mild cases—especially after car crashes—symptoms can take days to appear and may fluctuate, which is why step-by-step questioning matters (BrainLine, 2017; Hanscom Air Force Base, 2017). (Mayo Clinic, 2021; BrainLine, 2017; Hanscom AFB, 2017). Mayo Clinic+2BrainLine+2
What clinicians should ask:
-
Cognition: trouble concentrating, memory slips, slower thinking, word-finding problems (BrainLine, 2017). BrainLine
-
Mood/behavior: irritability, mood swings, anxiety, depression (Hanscom AFB, 2017; BrainLine, 2017). Hanscom Air Force Base+1
-
Senses: changes in taste or smell, light/noise sensitivity, ringing in the ears, blurred vision (Fisher Stark, 2021; BrainLine, 2017). MDPI+1
-
Physical: headaches, fatigue, sleep disturbance, dizziness, coordination or balance issues (Mayo Clinic, 2021; BrainLine, 2017). Mayo Clinic+1
These clusters of symptoms, particularly when accompanied by neck pain or whiplash, should trigger a mild traumatic brain injury (TBI) even if early imaging results are normal. It’s common for patients to blame stress or lack of sleep and never mention these changes unless asked directly (BrainLine, 2017; Fisher Stark, 2021). BrainLine+1
Why TBIs Get Overlooked
-
Symptoms are delayed or vague. People often feel “off” rather than injured. Headaches, mental fog, or sleep changes may be chalked up to stress (BrainLine, 2017; Mayo Clinic, 2021). BrainLine+1
-
Neck injuries muddy the picture. Cervical joint and soft-tissue problems from a crash can worsen headaches, dizziness, and brain fog, making it harder to separate spine-related issues from brain dysfunction (Denver Chiropractic, 2018; Northwest Florida Physicians Group, 2025). Denver Integrated Spine Center+1
-
Quick visits miss the nuance. Without a structured interview, subtle changes in smell, taste, or irritability may never get mentioned (Fisher Stark, 2021; Hanscom AFB, 2017). MDPI+1
Bottom line: A disciplined history and screening save lives and prevent long-term problems.
The Integrative Approach: Chiropractor + Nurse Practitioner
An integrative team pairs a chiropractor’s expertise in spinal/neuromusculoskeletal mechanics and sensorimotor rehab with an NP’s medical oversight of safety, symptoms, sleep, mood, and metabolic factors. Research and real-world programs show value when chiropractic care is included within multidisciplinary systems (Palmer Center for Chiropractic Research, 2022; Salsbury et al., 2018). Palmer College of Chiropractic+1
-
Chiropractic care: protects nerve function by improving joint motion, decreasing nociceptive input, and normalizing sensorimotor control; soft-tissue therapies reduce muscle guarding that feeds headaches and dizziness; tailored exercises target vestibular, ocular, and balance systems (NWHSU, 2022; Denver Chiropractic, 2018; NeuroChiro, n.d.; HML Functional Care, 2025). BioMed Central+3Northwestern Health Sciences University+3Denver Integrated Spine Center+3
-
Nurse practitioner supervision: screens red flags, manages medications and sleep, monitors mood changes, orders/coordinates imaging or specialist referrals, and educates families; nursing interventions help prevent secondary brain injury by close neuromonitoring and systematic protocols (Figueiredo et al., 2024). MDPI
-
Collaborative care — shared goals, clear communication, and patient-centered planning—improves continuity and captures needs that fall between disciplines (Riva et al., 2010). PMC
Dr. Alexander Jimenez’s clinical perspective
Drawing on dual-scope training (DC + APRN), Dr. Jimenez emphasizes thorough intake, cervical spine evaluation, vestibular-ocular screening, graded activity, and coordination with imaging and neuro specialists when indicated. His educational articles also discuss concussion testing and even emerging blood biomarkers that can support diagnosis in select cases (Jimenez, 2023; Jimenez, 2016). El Paso, TX Doctor Of Chiropractic+1
Common Cognitive, Emotional, and Sensory Symptoms to Watch
Cognitive: difficulty concentrating, slower processing, memory problems, word-finding issues (BrainLine, 2017). (BrainLine, 2017). BrainLine
Emotional/behavioral: irritability, mood swings, anxiety, or depression that began after the event (Hanscom AFB, 2017; BrainLine, 2017). Hanscom Air Force Base+1
Sensory: changes in taste or smell, tinnitus, light/noise sensitivity, blurred or double vision (Fisher Stark, 2021; BrainLine, 2017). MDPI+1
Physical/motor: headaches, fatigue, sleep problems, dizziness, balance and coordination issues (Mayo Clinic, 2021; BrainLine, 2017). Mayo Clinic+1
If you recognize several of these together after a hit, jolt, or whiplash, tell your provider and ask for a TBI evaluation.
The Care Plan: How Chiropractic and NP Teams Help After TBI
1) Protect the neck and normalize motion
Cervical joint dysfunction and muscle spasm can worsen headaches, dizziness, and eye strain. Gentle, evidence-informed spinal adjustments and mobilization—within safety guidelines—aim to reduce pain drivers and improve proprioception, helping the brain’s balance and eye-movement systems stabilize (NWHSU, 2022; Denver Chiropractic, 2018). Northwestern Health Sciences University+1
2) Soft-tissue therapies
Myofascial release, trigger-point work, and targeted stretching relieve muscle guarding from whiplash and can reduce tension-type headaches that amplify cognitive fatigue (Calibration Chiropractic + Functional Health, 2024; Pinnacle Health Chiropractic, 2025). Hanscom Air Force Base+1
3) Sensorimotor retraining
Vestibular and oculomotor exercises (e.g., gaze stabilization, saccades, smooth pursuit), balance work, and graded movement retrain brain-body coordination and reduce dizziness or motion sensitivity (NeuroChiro, n.d.; HML Functional Care, 2025; Denver Chiropractic—eye tracking). BrainLine+2BioMed Central+2
4) Graded aerobic activity
Once cleared medically, progressive, sub-symptom threshold cardio can improve recovery and mood. NPs help set safe pacing and check for setbacks such as overexertion, headaches, or sleep disruption (Mayo Clinic—post-concussion care, 2024). Mayo Clinic
5) Sleep, mood, and metabolic support
NPs screen for insomnia, anxiety/depression, and nutrition gaps. They may coordinate cognitive-behavioral strategies, nutrition counseling, and appropriate medications to control headaches, sleep problems, or mood shifts (Figueiredo et al., 2024; Mayo Clinic, 2024). MDPI+1
6) Education and return-to-life planning
Clear instructions—relative rest at first, then stepwise return to work, school, driving, and sports—prevent reinjury and help families support recovery (Mayo Clinic, 2021; BrainLine, 2017). Mayo Clinic+1
Tests and Instruments for TBI: From Simplest to Most Advanced
Below is a practical ladder of tools your team may use. Not every case needs every test. Start simple; escalate based on red flags, symptom severity, and response to care.
-
Structured history & red-flag screen
Focus on the mechanism of injury, loss of consciousness, amnesia, vomiting, seizures, severe/worsening headache, neck pain, focal weakness, and anticoagulant use. This is the foundation of all TBI evaluations (Mayo Clinic, 2021). (All patients) Mayo Clinic -
Neurological examination
Cranial nerves, strength, sensation, coordination, reflexes, and gait. Checks for focal deficits that may require urgent imaging or specialty referral (Mayo Clinic, 2021). (All patients) Mayo Clinic -
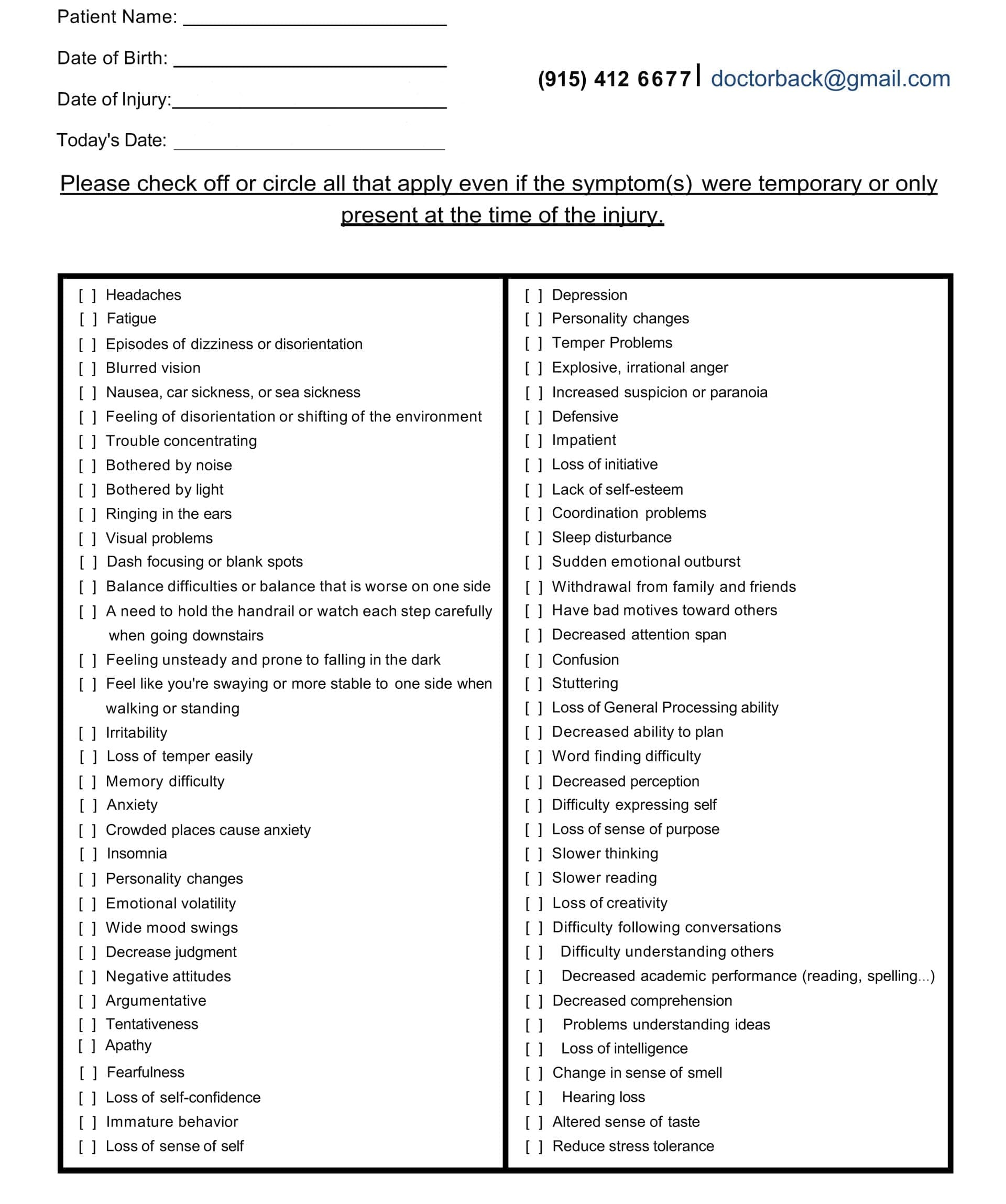
Symptom checklists/inventories
Standardized symptom questionnaires help track headaches, fatigue, sleep problems, and cognitive and sensory complaints over time. They are quick, repeatable, and guide care intensity (BrainLine, 2017). (Most patients) BrainLine -
Cognitive screening
Brief bedside tests (attention, memory, processing speed) identify deficits that need rest, school/work accommodations, or formal neuropsychological testing (Mayo Clinic, 2021). (Common) Mayo Clinic -
Balance and vestibular/ocular screening
Clinical balance checks and oculomotor screens (e.g., pursuit, saccades, vestibulo-ocular reflex) uncover dizziness and motion sensitivity that respond to targeted rehab (NeuroChiro, n.d.; HML Functional Care, 2025). (Common in dizzy/visual cases) BrainLine+1 -
Neuropsychological testing
If cognitive complaints persist or are job-critical, formal testing maps attention, memory, and executive function to guide return-to-work planning (BrainLine, 2017; Mayo Clinic, 2021). (As indicated) BrainLine+1 -
CT scan (acute imaging)
First-line imaging in emergency settings to detect bleeding, skull fracture, or swelling. Negative CT does not rule out concussion (Mayo Clinic, 2021). (Acute red flags) Mayo Clinic -
MRI (subacute/complicated cases)
Used after stabilization or if symptoms persist; can detect contusions and other structural problems missed by CT (Mayo Clinic, 2021). (When symptoms persist/worsen) Mayo Clinic -
Oculomotor/eye-tracking technology
Some clinics use computerized eye-tracking to quantify abnormal saccades or pursuit in post-concussion patients, guiding vision therapy (Denver Chiropractic—Eye-Tracking service). (If visual tracking issues) Denver Integrated Spine Center -
Blood biomarkers (emerging/adjunctive)
Research and early clinical trials explore markers such as GFAP and UCH-L1 to help rule out serious intracranial injury in select contexts; they supplement—not replace—clinical judgment (Jimenez, 2016). (Select emergency pathways) El Paso, TX Doctor Of Chiropractic
Remember: The right test at the right time depends on the story, exam, and red flags—not a one-size-fits-all checklist (Mayo Clinic, 2021). Mayo Clinic
A Sample Integrative Care Pathway
Week 0–1: Assess & Protect
-
Full history and neuro exam; red-flag screening; relative rest and symptom-limited activity; neck safety checks; initial symptom inventory; sleep and headache plan; if indicated, CT/MRI or emergency referral (Mayo Clinic, 2021). Mayo Clinic
Week 1–3: Restore & Retrain
-
Gentle cervical mobilization/adjustments and soft-tissue care; vestibular-ocular and balance exercises; sub-symptom aerobic activity; NP follow-up for sleep, mood, and medication review; education for pacing (NWHSU, 2022; Mayo Clinic, 2024). Northwestern Health Sciences University+1
Week 3–8: Progress & Personalize
-
Gradually advance gaze/balance drills and strength; address lingering neck drivers; consider neuropsychological testing if cognitive issues persist; coordinate workplace or school accommodations (BrainLine, 2017; Riva et al., 2010). BrainLine+1
Beyond 8 weeks: Complex or Persistent Symptoms
-
Re-evaluate; consider specialty referrals (neurology, neuro-ophthalmology, behavioral health); review imaging or additional tests as needed; keep spine/soft-tissue and sensorimotor care focused on functional goals (Figueiredo et al., 2024; Salsbury et al., 2018). MDPI+1
Safety First: When to Seek Urgent Care
Go to the ER or call emergency services for worsening or severe headache, repeated vomiting, seizures, weakness or numbness, slurred speech, significant confusion, unequal pupils, or any rapidly declining symptoms following a head or neck injury (Mayo Clinic, 2021). Mayo Clinic
FAQs
Can a normal CT mean I’m “fine”?
Not always. Concussions are a functional brain injury and often do not show on CT. That’s why symptom-guided care and follow-up are vital (Mayo Clinic, 2021). Mayo Clinic
Do chiropractic adjustments help brain recovery?
Adjustments don’t “treat the brain” directly, but by normalizing joint mechanics and reducing nociceptive load, they can lower headache drivers and improve sensorimotor control—supporting balance, eye-movement work, and graded activity (NWHSU, 2022; NeuroChiro, n.d.; HML Functional Care, 2025). Northwestern Health Sciences University+2BrainLine+2
What does the NP do on this team?
The NP coordinates safety, medications, sleep, mood support, and specialty referrals; nursing interventions have been documented to prevent secondary injury through neuromonitoring and standardized care processes (Figueiredo et al., 2024). MDPI
Key Takeaways
-
Hidden TBIs are common. Subtle cognitive, emotional, sensory, and sleep changes are classic—but easy to miss (BrainLine, 2017; Fisher Stark, 2021). BrainLine+1
-
Thorough history is everything. The right questions uncover patterns, scans may not (Mayo Clinic, 2021; Hanscom AFB, 2017). Mayo Clinic+1
-
Integrative care helps. Combining chiropractic spine/soft-tissue and sensorimotor work with NP-led medical oversight supports the nervous and musculoskeletal systems together (Palmer Center for Chiropractic Research, 2022; Salsbury et al., 2018; Riva et al., 2010). Palmer College of Chiropractic+2BioMed Central+2
-
Testing is stepwise. Start with history, exam, and symptom tools, then escalate to neuropsychological testing, CT/MRI, oculomotor tech, or biomarkers as needed (Mayo Clinic, 2021; Denver Chiropractic, 2018; Jimenez, 2016). Mayo Clinic+2Denver Integrated Spine Center+2
Final Word
TBI is easy to overlook but hard on daily life when missed. The best protection is a complete history, thoughtful questions, and a team that treats your brain and body together. If you or someone you love develops new problems with focus, mood, sleep, balance, headache, or senses after a head/neck event—speak up and ask for a TBI evaluation. Chiropractic and nurse practitioner teams can coordinate safe, stepwise care to help you heal (Mayo Clinic, 2021; Figueiredo et al., 2024; Riva et al., 2010). Mayo Clinic+2MDPI+2
References
-
BrainLine. (2017). TBI 101: Physical symptoms. https://brainline.org/article/tbi-101-physical-symptoms BrainLine
-
Calibration Chiropractic + Functional Health. (2024). How integrative chiropractic care helps with traumatic brain injuries. https://www.calibrationmansfield.com/blog/how-can-integrative-chiropractic-care-help-with-traumatic-brain-injuries.html Hanscom Air Force Base
-
Denver Integrated Spine Center. (2018). Chiropractor after concussion: How chiropractors can help treat mTBI. https://denver-chiropractic.com/mild-traumatic-brain-injury-can-chiropractor-help/ Denver Integrated Spine Center
-
Figueiredo, R., Castro, C., & Fernandes, J. B. (2024). Nursing interventions to prevent secondary injury in critically ill patients with traumatic brain injury: A scoping review. Journal of Clinical Medicine, 13(8), 2396. https://www.mdpi.com/2077-0383/13/8/2396 MDPI
-
Fisher Stark, P.A. (2021). Hidden signs of a serious head injury (traumatic brain injury). https://fisherstark.com/hidden-signs-of-a-serious-head-injury-traumatic-brain-injury/ MDPI
-
Hanscom Air Force Base (U.S. Air Force). (2017). TBI recognition critical to treating invisible wounds. https://www.hanscom.af.mil/News/Article-Display/Article/1126278/tbi-recognition-critical-to-treating-invisible-wounds/ Hanscom Air Force Base
-
HML Functional Care. (2025). How chiropractic neurology supports brain healing. https://hmlfunctionalcare.com/how-chiropractic-neurology-supports-brain-healing/ BioMed Central
-
Jimenez, A. (2016). Blood markers could detect concussion. https://dralexjimenez.com/blood-markers-could-detect-concussion/ El Paso, TX Doctor Of Chiropractic
-
Jimenez, A. (2023). The importance of concussion tests for brain injury evaluation. https://dralexjimenez.com/the-importance-of-concussion-tests-for-brain-injury-evaluation/ El Paso, TX Doctor Of Chiropractic
-
Mayo Clinic. (2021). Traumatic brain injury—Diagnosis & treatment. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/diagnosis-treatment/drc-20378561 Mayo Clinic
-
Mayo Clinic. (2024). Persistent post-concussive symptoms: Diagnosis & treatment. https://www.mayoclinic.org/diseases-conditions/post-concussion-syndrome/diagnosis-treatment/drc-20353357 Mayo Clinic
-
NeuroChiro (Chiropractic neurologist service page). (n.d.). Brain injury services. https://www.neurochiro.com/services/brain-injury/ BrainLine
-
Northwestern Health Sciences University (NWHSU). (2022). Chiropractic and traumatic brain injuries. https://www.nwhealth.edu/news/reis-writes-for-chiropractic-economics-chiropractic-and-traumatic-brain-injuries/ Northwestern Health Sciences University
-
Northwest Florida Physicians Group. (2025). Using chiropractic care to treat traumatic brain injuries. https://www.northwestfloridaphysiciansgroup.com/using-chiropractic-care-to-treat-traumatic-brain-injuries/ BioMed Central
-
Palmer Center for Chiropractic Research. (2022). New study: Integrating chiropractic into multidisciplinary settings adds value. https://www.palmer.edu/palmer-blog/new-study-says-integrating-chiropractic-into-multidisciplinary-settings-adds-value-for-patients-and-providers/ Palmer College of Chiropractic
-
Pinnacle Health Chiropractic. (2025). Six ways chiropractic care supports healing after TBI. https://www.pinnaclehealthchiro.com/blog/six-ways-chiropractic-care-supports-healing-after-tbi/ Invalid URL
-
Riva, J. J., et al. (2010). Chiropractors and collaborative care: An overview illustrated with a case report. https://pmc.ncbi.nlm.nih.gov/articles/PMC2921780/ PMC
-
Salsbury, S., et al. (2018). Be good, communicate, and collaborate: A qualitative analysis of stakeholders in a neurorehabilitation setting. Chiropractic & Manual Therapies. https://chiromt.biomedcentral.com/articles/10.1186/s12998-018-0200-4 BioMed Central
-
Apex Chiropractic. (2022). 3 benefits of chiropractic care following a traumatic brain injury. https://apexchiroco.com/auto-injury/3-benefits-of-chiropractic-care-following-a-traumatic-brain-injury/
-
Calibration Chiropractic + Functional Health. (2024). How integrative chiropractic care helps with TBIs. (duplicate listing above; included). Hanscom Air Force Base
Post Disclaimer
Professional Scope of Practice *
The information herein on "Hidden Signs of Traumatic Brain Injury Explained" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.