Functional Medicine: Glossary
 Allostasis: The process of achieving stability, or homeostasis, through physiological or behavioral change. This can be carried out by means of alteration in HPATG axis hormones, the autonomic nervous system, cytokines, or a number of other systems, and is generally adaptive in the short term. It is essential in order to maintain internal viability amid changing conditions.
Allostasis: The process of achieving stability, or homeostasis, through physiological or behavioral change. This can be carried out by means of alteration in HPATG axis hormones, the autonomic nervous system, cytokines, or a number of other systems, and is generally adaptive in the short term. It is essential in order to maintain internal viability amid changing conditions.
Antecedents: Factors that predispose to acute or chronic illness. For a person who is ill, antecedents form the illness diathesis. From the perspective of prevention, they are risk factors. Examples of genetic antecedents include the breast cancer risk genes BRCA1 and BRCA2.
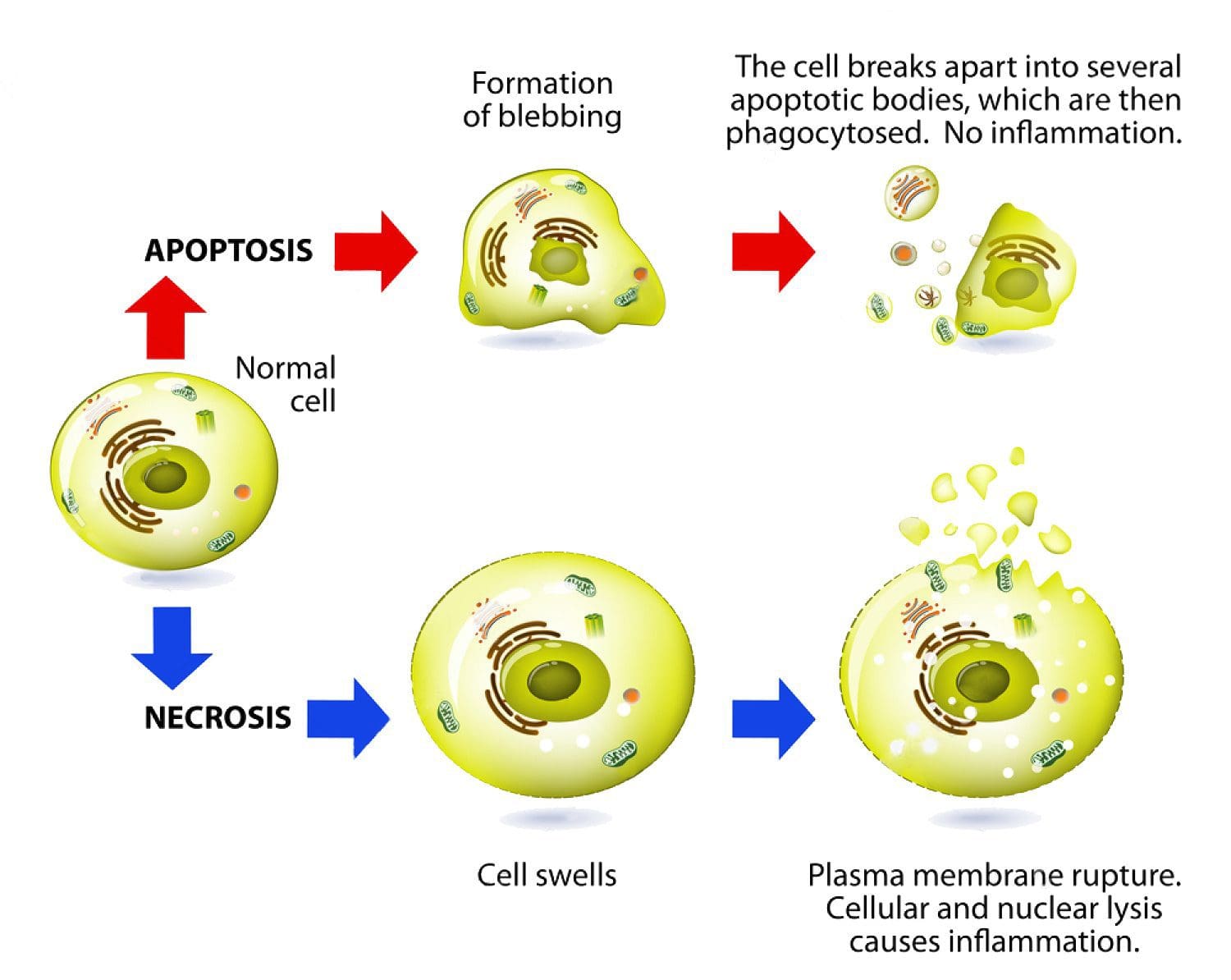
Apoptosis: Programmed cell death. As a normal part of growth and development, cells that are superfluous or that become damaged activate a cascade of intracellular processes leading to their own demise. In cancer cells, DNA damage may inactivate the apoptosis cascade, allowing mutated cells to survive and proliferate.
Biochemical individuality: Each individual has a unique physiological and biochemical composition, based upon the interactions of his or her individual genetic make-up with lifestyle and environment—i.e., the continuous exposure to inputs (diet, experiences, nutrients, beliefs, activity, toxins, medications, etc.) that influence our genes. It is this combination of factors that accounts for the endless variety of phenotypic responses seen every day by clinicians. The unique makeup of each individual requires personalized levels of nutrition and a lifestyle adapted to that individual’s needs in order to achieve optimal health. The consequences of not meeting the specific needs of the individual are expressed, over time, as degenerative disease.Â
Bioidentical Hormone Therapy: Giving exogenous hormones that are identical in structure to the endogenous hormones.Â
Biomarker: A substance used as an indicator of a biological state. Such characteristics are objectively measured and evaluated as indicators of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention. Cancer biomarkers include prostate specific antigen (PSA) and carcinoembryonic antigen (CEA).
Biotransformation: The chemical modification(s) of a compound made by an organism. Compounds modified in the body include, but are not limited to, nutrients, amino acids, toxins, heavy metals, and drugs. Biotransformation also renders nonpolar compounds polar so that they are excreted, not reabsorbed in renal tubules.
Cancer: A group of diseases characterized by uncontrolled growth and spread of abnormal cells, which, if not controlled, can result in death. Cancer is caused by both external factors (tobacco, infectious organisms, chemicals, and radiation) and internal factors (inherited mutations, hormones, immune conditions, and mutations that occur from metabolism), two or more of which may act together or in sequence to initiate or promote carcinogenesis. Ten or more years often pass between exposure to external factors and detectable cancer.
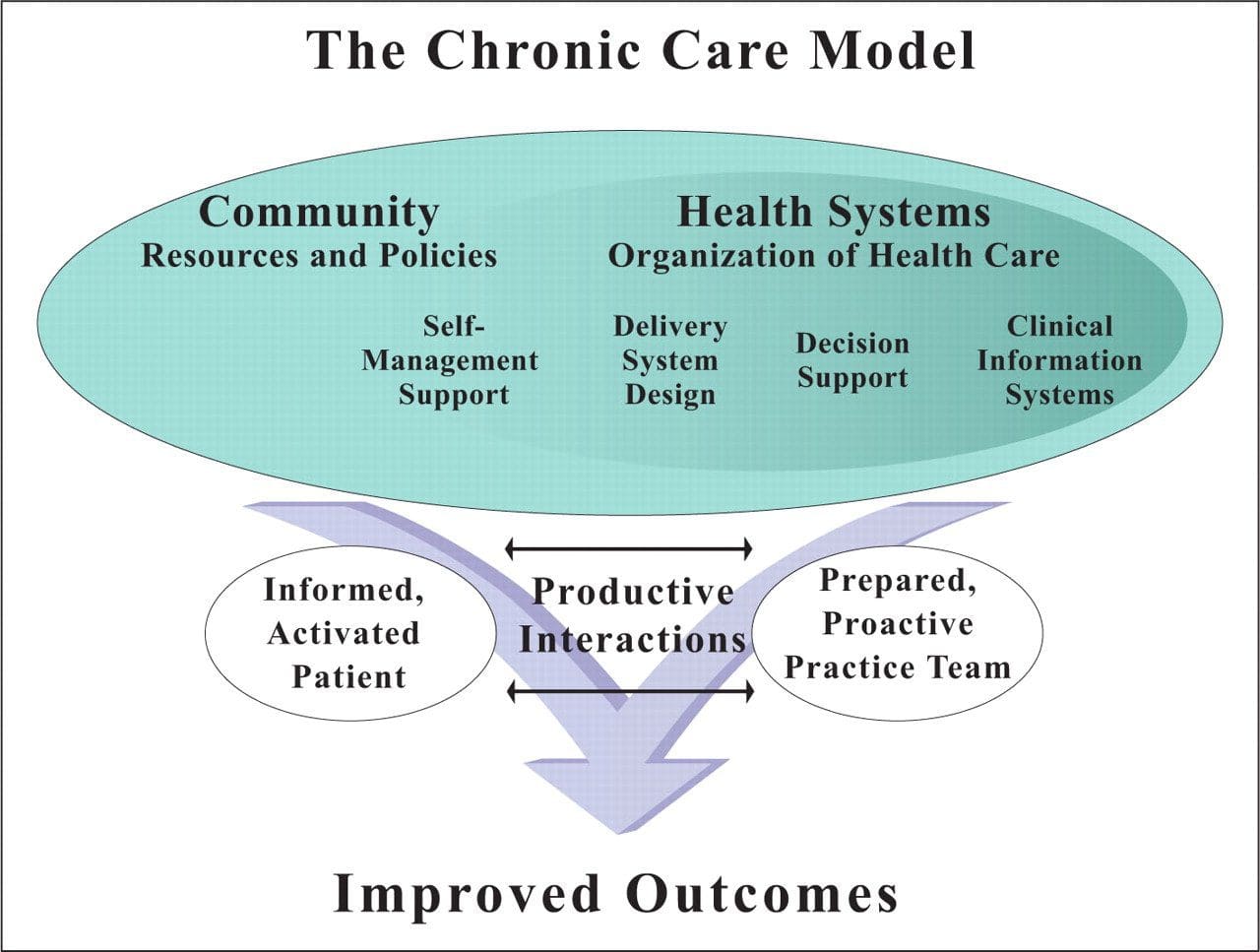 Chronic Care Model: Developed by Wagner and colleagues, the primary focus of this model is to include the essential elements of a healthcare system that encourage high-quality chronic disease care. Such elements include the community, the health system, self-management support, delivery system design, decision support and clinical information systems. It is a response to powerful evidence that patients with chronic conditions often do not obtain the care they need, and that the healthcare system is not currently structured to facilitate such care.Â
Chronic Care Model: Developed by Wagner and colleagues, the primary focus of this model is to include the essential elements of a healthcare system that encourage high-quality chronic disease care. Such elements include the community, the health system, self-management support, delivery system design, decision support and clinical information systems. It is a response to powerful evidence that patients with chronic conditions often do not obtain the care they need, and that the healthcare system is not currently structured to facilitate such care.Â
 Complementary and Alternative Medicine (CAM): A group of diverse medical and healthcare systems, practices, and products that are not presently considered to be part of conventional, mainstream medicine. The list of what is considered to be CAM changes frequently, as therapies demonstrated to be safe and effective are adopted by conventional practitioners, and as new approaches to health care emerge. Complementary medicine is used with conventional medicine, not as a substitute for it. Alternative medicine is used in place of conventional medicine. Functional medicine is neither complementary nor alternative medicine; it is an approach to medicine that focuses on identifying and ameliorating the underlying causes of disease; it can be used by all practitioners with a Western medical science background and is compatible with both conventional and CAM methods.Â
Complementary and Alternative Medicine (CAM): A group of diverse medical and healthcare systems, practices, and products that are not presently considered to be part of conventional, mainstream medicine. The list of what is considered to be CAM changes frequently, as therapies demonstrated to be safe and effective are adopted by conventional practitioners, and as new approaches to health care emerge. Complementary medicine is used with conventional medicine, not as a substitute for it. Alternative medicine is used in place of conventional medicine. Functional medicine is neither complementary nor alternative medicine; it is an approach to medicine that focuses on identifying and ameliorating the underlying causes of disease; it can be used by all practitioners with a Western medical science background and is compatible with both conventional and CAM methods.Â
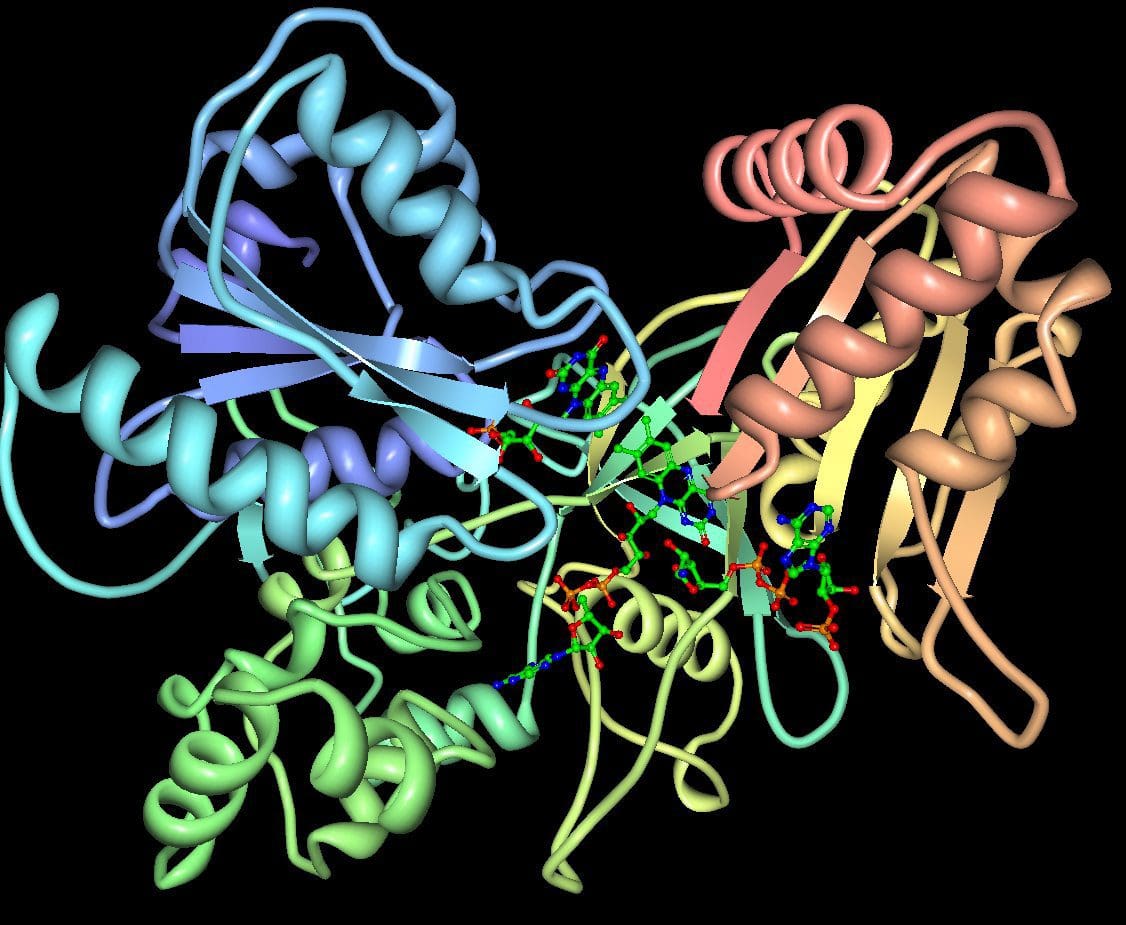 Cytochromes P450 (CYP 450): A large and diverse group of enzymes, most of which function to catalyze the oxidation of organic substances. They are located either in the inner membrane of mitochondria or in the endoplasmic reticulum of cells ans play a critical role in the detoxification of endogenous and exogenous toxins. The substrates of CYP enzymes include metabolic intermediates such as lipids, steroidal hormones, and xenobiotic substances such as drugs.
Cytochromes P450 (CYP 450): A large and diverse group of enzymes, most of which function to catalyze the oxidation of organic substances. They are located either in the inner membrane of mitochondria or in the endoplasmic reticulum of cells ans play a critical role in the detoxification of endogenous and exogenous toxins. The substrates of CYP enzymes include metabolic intermediates such as lipids, steroidal hormones, and xenobiotic substances such as drugs.
DIGIN: A heuristic mnemonic for assessment of gastrointestinal dysfunction. Thorough assessment of the GI tract should include investigation of the following:
- Digestion/Absorption – Problems with the digestive process including ingestion, chemical digestion, mechanical digestion, absorption, and/or assimilation
- Intestinal Permeability – Permeability of the intestinal barrier: is the epithelium allowing in larger particles in a paracellular manner, making the gut barrier “leaky�
- Gut Microbiota/Dysbiosis – Changes in composition of the gut flora including balance and interaction of commensal species (See: Dysbiosis)
- Inflammation/Immune – Inflammation and immune activity in the GI tract
- Nervous System – Enteric nervous system function, which controls motility, blood flow, uptake of nutrients, secretion, and immunological and inflammatory processes in the gut.
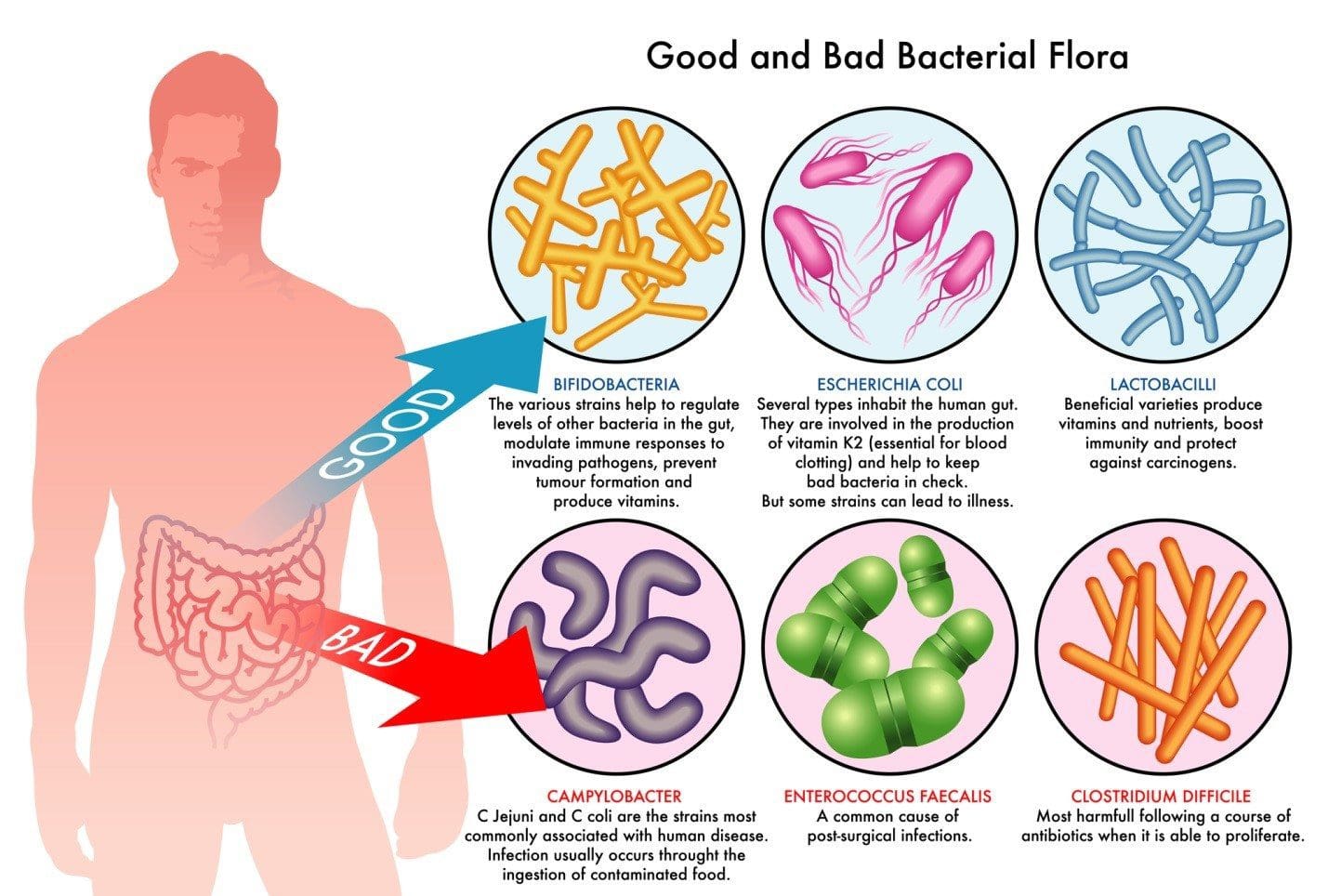 Dysbiosis: A condition that occurs when the normal symbiosis between gut flora and the host is disturbed and organisms of low intrinsic virulence, which normally coexist peacefully with the host, may promote illness. It is distinct from gastrointestinal infection, in which a highly virulent organism gains access to the gastrointestinal tract and infects the host.Â
Dysbiosis: A condition that occurs when the normal symbiosis between gut flora and the host is disturbed and organisms of low intrinsic virulence, which normally coexist peacefully with the host, may promote illness. It is distinct from gastrointestinal infection, in which a highly virulent organism gains access to the gastrointestinal tract and infects the host.Â
Functional Medicine: A systems-based, science-driven approach to individualized medicine that addresses the underlying causes of disease, using a systems-oriented approach and engaging both patient and practitioner in a therapeutic partnership. It reflects a personalized lifestyle medicine approach and utilizes the Functional Medicine Matrix to organize the patient’s story and determine appropriate interventions for the prevention and treatment of chronic diseases.
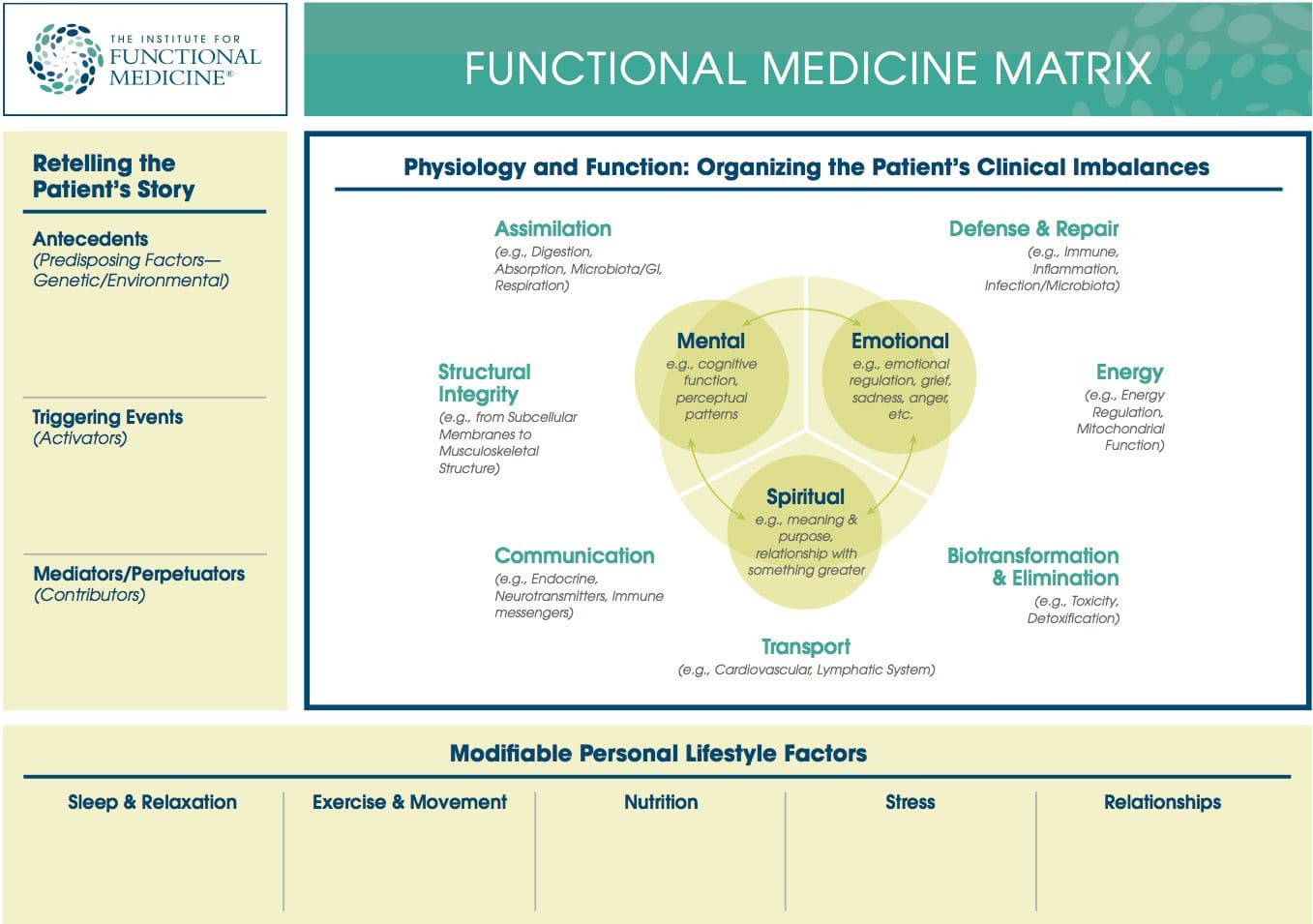 Functional Medicine Matrix: The graphic representation of the functional medicine approach, displaying the seven organizing physiological systems, the patient’s known antecedents, triggers, and mediators, and the personalized lifestyle factors that promote health. Practitioners can use the matrix to help organize their thoughts and observations about the patient’s health and decide how to focus therapeutic and preventive strategies.
Functional Medicine Matrix: The graphic representation of the functional medicine approach, displaying the seven organizing physiological systems, the patient’s known antecedents, triggers, and mediators, and the personalized lifestyle factors that promote health. Practitioners can use the matrix to help organize their thoughts and observations about the patient’s health and decide how to focus therapeutic and preventive strategies.
Cytokines: Immunoregulatory proteins (such as interleukin, tumor necrosis factor, and interferon). They may act locally or systemically and tend to have both immunomodulatory and other effects on cellular processes in the body. Cytokines have been used in the treatment of certain cancers.Â
Genomics: The study of the whole genome of organisms, including interactions between loci and alleles within the genome. Research on single genes does not fall into the definition of genomics unless the aim of this functional information analysis is to elucidate the gene’s effect on the entire genome network. Genomics may also be defined as the study of all the genes of a cell, or tissue, at the DNA (genotype), mRNA (transcriptome), or protein (proteome) levels.Â
GO-TO-IT: A heuristic mnemonic for the processes involved in the clinical practice of functional medicine:
- Gather oneself and be mindful in preparing to see each patient; gather information through intake forms, questionnaires, the initial consultation, physical exam, and objective data. A detailed functional medicine history that is appropriate to age, gender, and nature of presenting problems is taken.
- Organize the subjective and objective details from the patient’s story within the functional medicine paradigm. Position the patient’s presenting signs and symptoms, along with the details of the case history, on the timeline and Functional Medicine Matrix.
- Tell the story back to the patient in your own words to ensure accuracy and understanding. The re-telling of the patient’s story is a dialogue about the case highlights—including the antecedents, triggers, and mediators identified in the history and correlating them to the timeline and matrix. The patient is asked to correct and amplify the story, engendering a context of true partnership.
- Order and then prioritize the patient’s information:
- Acknowledge patient’s goals
- Address modifiable lifestyle factors
- Sidney Baker’s too much/not enough model: what are the insufficiencies/excesses?
- Identify clinical imbalances or disruptions in the organizing physiological systems of the matrix
- Initiate further functional assessment and intervention based upon the above work:
- Perform further assessment
- Referral to adjunctive care:
- Nutritional professionals
- Lifestyle educators
- Other healthcare providers
- Specialists
- Initiate therapy
- Track assessments, note the effectiveness of the therapeutic approach, and identify clinical outcomes at each visit—in partnership with the patient.
Heuristic: A strategy used for problem solving, learning, and discovery that is experience-based, not algorithmic. When an exhaustive search is impractical, heuristic methods may be used to speed up the process of finding a satisfactory solution. A heuristic is sometimes referred to as a rule of thumb.
Homeostasis and Homeodynamics: The former term describes the tendency of living things to maintain physiological parameters within a narrow range usually considered normal in order to maintain optimal function. Under this definition, disease can be defined as a departure from the homeostatic state. The latter term describes the tendency of homeostatic set points to change throughout an organism’s lifespan, and thus describes how departures from a homeostatic norm can be adaptive (e.g., fever) or pathological, depending on the context.
Integrative Medicine: Medicine that combines treatments from conventional medicine and those from Complementary and Alternative Medicine (CAM) for which there is some high-quality evidence of safety and effectiveness. In a broader sense, it is healing-oriented medicine that takes into account the whole person (body, mind, and spirit), including all aspects of lifestyle, and makes use of all appropriate therapies, both conventional and alternative. The field is more than 10 years old and it is the only one of the emerging models to explicitly encompass the integration of therapeutics that, until recently, were the sole purview of complementary and alternative medicine. Note: functional medicine is different from integrative medicine because functional medicine emphasizes the evaluation of underlying causes of health and dysfunction and organizes assessment and treatment using the Functional Medicine Matrix, the timeline, and GOTOIT.
 Lifestyle Medicine: The use of lifestyle interventions such as nutrition, physical activity, stress reduction, and rest to lower the risk for the approximately 70% of modern health problems that are lifestyle-related chronic diseases (such as obesity and type 2 diabetes), or for the treatment and management of disease if such conditions are already present. It is an essential component of the treatment of most chronic diseases and has been incorporated in many national disease management guidelines.
Lifestyle Medicine: The use of lifestyle interventions such as nutrition, physical activity, stress reduction, and rest to lower the risk for the approximately 70% of modern health problems that are lifestyle-related chronic diseases (such as obesity and type 2 diabetes), or for the treatment and management of disease if such conditions are already present. It is an essential component of the treatment of most chronic diseases and has been incorporated in many national disease management guidelines.
Long Latency Disease: Disease that becomes manifest at a time remote from the initial exposure to disease triggers, or that requires continued exposure to triggers and mediators over an extended period of time to manifest frank pathology. Examples include heart disease, cancer, and osteoporosis.Â
Mediators: Intermediaries that contribute to the continued manifestations of disease. Mediators do not cause disease; instead, they underlie the host response to triggers. Examples include biochemical factors (e.g., cytokines and leukotrienes) as well as psychosocial ones (e.g., reinforcement for staying ill).Â
Metabolomics (or metabonomics): “The study of metabolic responses to drugs, environmental changes and diseases. Metabonomics is an extension of genomics (concerned with DNA) and proteomics (concerned with proteins). Following on the heels of genomics and proteomics, metabonomics may lead to more efficient drug discovery and individualized patient treatment with drugs, among other things.†(From MedicineNet.com)Â
Nutrigenomics (or nutritional genomics): The study of how different foods may interact with specific genes to increase the risk of common chronic diseases such as type 2 diabetes, obesity, heart disease, stroke, and certain cancers. It can also be described as the study of the influence of genetic variation on nutrition by correlating gene expression or single-nucleotide polymorphisms with a nutrient’s absorption, metabolism, elimination, or biological effects. Nutrigenomics also seeks to provide a molecular understanding of how common chemicals in the diet affect health by altering the expression of genes and the structure of an individual’s genome. The ultimate aim of nutrigenomics is to develop rational means to optimize nutrition for the patient’s genotype.Â
Organ Reserve: The difference between the maximal function of a vital organ and the level of function required to maintain an individual’s daily life. In other words, it is the “reserve power†of a particular organ, above and beyond what is required in a healthy individual. It can also be thought of as the degrees of freedom available in the body organs to perform their functions and maintain health. Decline in the organ reserve occurs under stress, during sickness, and as we age.Â
Organ System Diagnosis: In the allopathic medical model, it is common to give a collection of symptoms a name based on dysfunction in an organ system, then to cite the named disease as the cause of the symptoms the patient is experiencing. This bit of circular logic avoids any discussion of the systemic or underlying causes of dysfunction and also treats all people with “disease X†the same, despite the fact that two people with the same collection of symptoms may have completely different underlying physiological causes for the symptoms they display.Â
Organizing Physiological Systems: To assist clinicians in understanding and applying the complexity of functional medicine, IFM has organized and adapted a set of seven interrelated biological systems that underlie all physiology. Imbalances in these systems or core clinical imbalances are the underlying cause of disease and dysfunction.
- Assimilation (e.g., Digestion, Absorption, Microbiota/GI, Respiration)
- Defense and Repair (e.g., Immune, Inflammation, Infection/Microbiota)
- Energy (e.g., Energy Regulation, Mitochondrial Function)
- Biotransformation and Elimination (e.g., Toxicity, Detoxification)
- Transport (e.g., Circulation, Lymphatic Flow)
- Communication (e.g., Endocrine, Neurotransmitters, Immune messengers)
- Structural Integrity (e.g., from Subcellular Membranes to Musculoskeletal Structure)Â
Using this construct, it becomes much clearer that one disease/condition may have multiple causes (i.e., multiple clinical imbalances), just as one fundamental imbalance may be at the root of many seemingly disparate conditions.Â
Oxidation-Reduction (also called Redox): Paired chemical reactions that occur in balance with each other within the body of a healthy individual. These reactions involve the transfer of electrons (or the distribution of electron sharing) and thus require both a donor and acceptor. When this physiological parameter is out of balance, a net accumulation of donors or acceptors can lead to deleterious cellular oxidation phenomena (lipid peroxidation, free radical formation).Â
Oxidative Stress: Oxidative stress occurs when there is an imbalance between the production of damaging reactive oxygen species and an individual’s antioxidant capacity to detoxify the reactive intermediates or to repair the resulting damage. Disturbances in the normal redox state of tissues can cause toxic effects through the production of peroxides and free radicals that damage all components of the cell, including proteins, lipids, and DNA. Oxidative stress is implicated in the etiology of several chronic diseases including atherosclerosis, Parkinson’s disease, Alzheimer’s disease, and chronic fatigue syndrome.Â
Personalized Lifestyle Factors: The modifiable lifestyle factors that appear along the bottom of the Functional Medicine Matrix. Clinicians and their patients can partner to develop an individualized plan for addressing these issues. Health-promoting lifestyle factors include:
- Sleep and Relaxation – Getting adequate sleep and meaningful relaxation time in one’s life
- Exercise and Movement – Participating in physical activity that is appropriate for age and health
- Nutrition and Hydration – Eating a diet that is appropriate for age, genetic background, and environment, as well as maintaining adequate hydration
- Stress and Resilience – Reducing stress levels and managing existing stress
- Relationships and Networks – Developing and maintaining healthy relationships and social networks while reducing the impact of noxious relationships
Personalized (Individualized) Medicine: Personalized medicine can be described as the effort to define and strengthen the art of individualizing health care by integrating the interpretation of patient data (medical history, family history, signs, and symptoms) with emerging “–omic†technologies—nutritional genomics, pharmacogenomics, proteomics, and metabolomics. It is also defined as medicine that treats each patient as a unique individual and takes into account the totality of personal history, family history, environment and lifestyle, physical presentation, genetic background, and mind/body/spirit. Interventions are tailored to each patient and adjusted based on the patient’s individualized response.Â
Precipitating Event: Similar to a trigger—a trigger, however, only provokes illness as long as the person is exposed to it (or for a short while afterward), while a precipitating event initiates a change in health status that persists long after the exposure ends
Prospective Medicine (aka: 4-P Medicine): A relatively new concept introduced in 2003, prospective medicine is a descriptive rather than a prescriptive term, encompassing “personalized, predictive, preventive, and participatory medicine.†Snyderman argues persuasively that a comprehensive system of care would address not only new technologies (e.g., identification of biomarkers, use of electronic and personalized health records), but also delivery systems, reimbursement mechanisms, and the needs of a variety of stakeholders (government, consumers, employers, insurers, and academic medicine). Prospective medicine does not claim to stake out new scientific or clinical territory; instead, it focuses on creating an innovative synthesis of technologies and models—particularly personalized medicine (the “-omicsâ€) and systems biology—in order to “determine the risk for individuals to develop specific diseases, detect the disease’s earliest onset, and prevent or intervene early enough to provide maximum benefit.Â
Proteomics: The large-scale study of proteins, particularly their structures and functions, how they’re modified, when and where they’re expressed, how they’re involved in metabolic pathways, and how they interact with one another. The proteome is the entire complement of proteins, including the modifications made to a particular set of proteins, produced by an organism or system. This will vary with time and distinct requirements, or stresses, that a cell or organism undergoes. As a result, proteomics is much more complicated than genomics: an organism’s genome is more or less constant, while the proteome differs from cell to cell and from time to time.Â
PURE: A heuristic mnemonic for assessment and treatment of toxicity-related disorders. Steps to consider when assessing and treating patients with toxic exposures include:
- Pattern Recognition – Recognize common patterns of toxicity signs and symptoms, including those associated with neurodevelopmental toxicity, immunotoxicity, mitochondrial toxicity, and endocrine toxicity
- Undersupported/Overexposed – Examine the patient’s environment and lifestyle to determine what might be lacking and what there might be too much of
- Reduce Toxin Exposure – Design a strategy for the patient to avoid continued toxin exposure
- Ensure a Safe Detox – Support the patient during detoxification by ensuring adequate nutrients to aid in the detoxification and biotransformation process and by recommending lifestyle changes that increase the safety and efficacy of detox programs.Â
PTSD: A heuristic for general treatment of hormone-related disorders. Factors to be considered include:
- Production – Production/synthesis and secretion of the hormone
- What are the building blocks of thyroid hormone and cortisol?
- What affects the secretion of insulin?
- What are the building blocks of serotonin?
- What affects synthesis-inflammation of the gland (as in autoimmune thyroiditis)?
- Transport – Transport/conversion/distribution/ interaction with other hormones
- Do the levels of insulin impact the levels of E or T?
- Does a hormone’s transport from its gland of origin to the target gland impact its effectiveness or toxicity?
- Can we influence the level of free hormone?
- Is the hormone transformed (T4 to T3 or RT3) and can we modulate that?
- Sensitivity – Cellular sensitivity to the hormone signal
- Are there nutritional or dietary factors that influence the cellular response to insulin, thyroid hormones, estrogens, etc.?
- Detoxification – Detoxification/excretion of the hormone. For example:
- How is estradiol metabolized in the process of biotransformation?
- Can we alter it?
- What can we do to affect the binding to and excretion of estrogens?
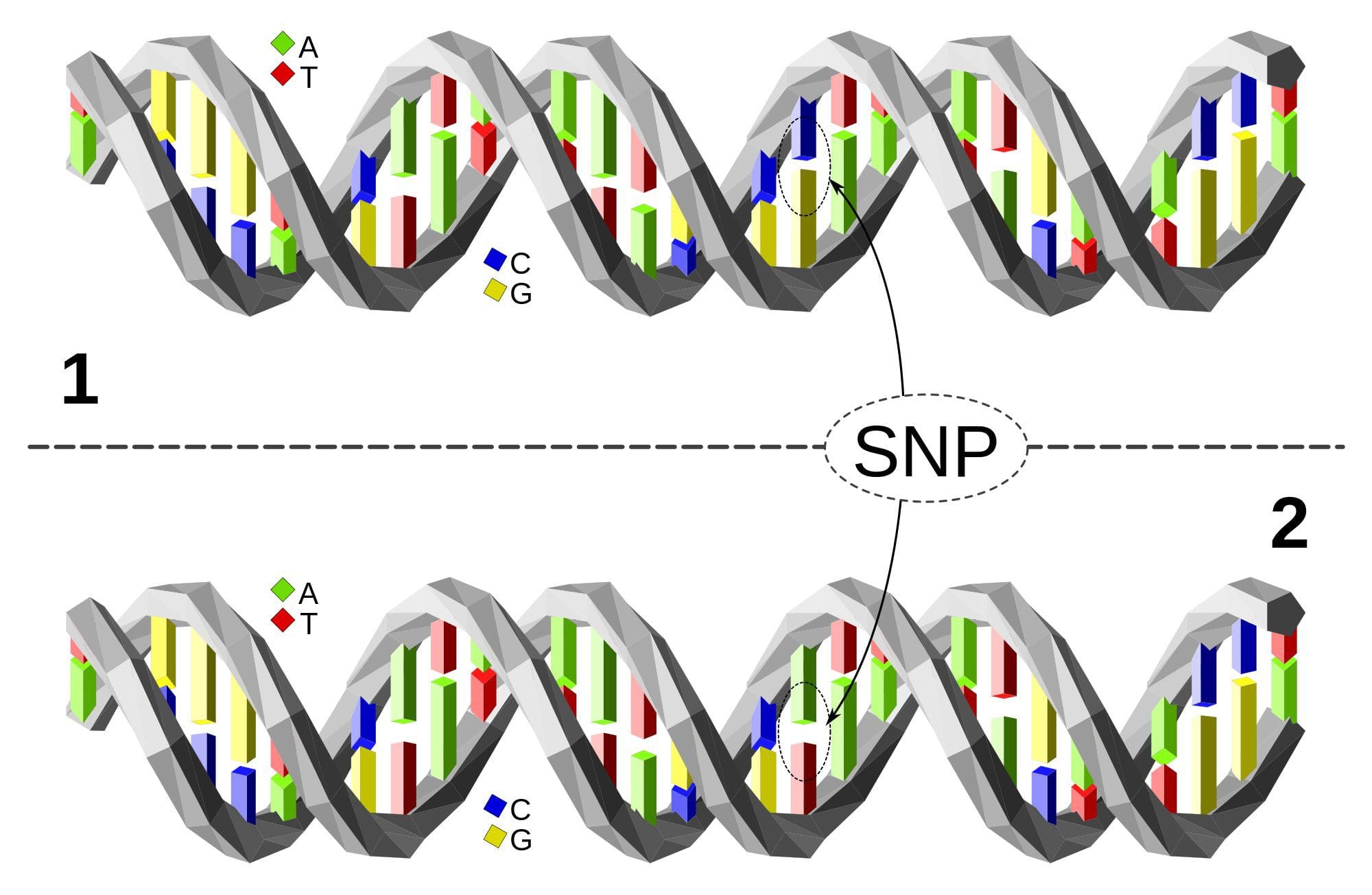 Single Nucleotide Polymorphism or SNP (pronounced “snipâ€) is a DNA sequence variation occurring when a single nucleotide—A, T, C, or G—in the genome differs between members of a species or between paired chromosomes in an individual. Almost all common SNPs have only two alleles. These genetic variations underlie differences in our susceptibility to, or protection from, several diseases. Variations in the DNA sequences of humans can affect how humans develop diseases. For example, a single base difference in the genes coding for apolipoprotein E is associated with a higher risk for Alzheimer’s disease. SNPs are also manifestations of genetic variations in the severity of illness, the way our body responds to treatments, and the individual response to pathogens, chemicals, drugs, vaccines, and other agents. They are thought to be key factors in applying the concept of personalized medicine.
Single Nucleotide Polymorphism or SNP (pronounced “snipâ€) is a DNA sequence variation occurring when a single nucleotide—A, T, C, or G—in the genome differs between members of a species or between paired chromosomes in an individual. Almost all common SNPs have only two alleles. These genetic variations underlie differences in our susceptibility to, or protection from, several diseases. Variations in the DNA sequences of humans can affect how humans develop diseases. For example, a single base difference in the genes coding for apolipoprotein E is associated with a higher risk for Alzheimer’s disease. SNPs are also manifestations of genetic variations in the severity of illness, the way our body responds to treatments, and the individual response to pathogens, chemicals, drugs, vaccines, and other agents. They are thought to be key factors in applying the concept of personalized medicine.
Relative Risk: A measure of the strength of the relationship between risk factors and a condition. For example, one could compare the risk of developing cancer in persons with a certain exposure or trait to the risk in persons who do not have this characteristic. Male smokers are about 23 times more likely to develop lung cancer than nonsmokers, so their relative risk is 23. Most relative risks are not this large. For example, women who have a first-degree relative (mother, sister, or daughter) with a history of breast cancer have about twice the risk of developing breast cancer compared to women who do not have this family history.Â
Systems Biology: Although there is not yet a universally recognized definition of systems biology, the National Institute of General Medical Services (NIGMS) at NIH provides the following explanation: “A field that seeks to study the relationships and interactions between various parts of a biological system (metabolic pathways, organelles, cells, and organisms) and to integrate this information to understand how biological systems function.â€
The 5Rs: A heuristic mnemonic for the five-step process used to normalize gastrointestinal function that is a core element of functional medicine:
- Remove – Removing the source of the imbalance (e.g., pathogens, allergic foods) is the critical first step.
- Replace – Next replace any factors that are missing (e.g., HCL, digestive enzymes)
- Reinoculate – Repopulate the gut with symbiotic bacteria (e.g., lactobacilli, bifidobacteria)
- Repair – Heal damaged gut membranes using, for example, glutamine, fiber, and butyrate
- Rebalance – Modify attitude, diet, and lifestyle of the patient to promote a healthier way of living
Three Legs of the Stool: A framework for practicing functional medicine that includes three parts:
- Retelling the patient’s story with ATMs (antecedents, triggers, and mediators): The clinician collects information from the patient through extensive interaction, then reflects the problem back to the patient in terms of antecedents, triggers, and mediators
- Organizing the clinical imbalances: The clinician organizes the clinical imbalances in the organizing physiological systems and lists them on the Functional Medicine Matrix.
- Personalized lifestyle factors: The clinician assesses each patient’s environment and lifestyle, and partners with patients to help them develop, adopt, and maintain appropriate personalized health-promoting behaviors.Â
Timeline: A tool that allows clinicians to visualize a patient’s story chronologically by organizing important life events and health issues from pre-conception to the present.
 Triage Theory: Linus Pauling Award winner Bruce Ames’ theory that DNA damage and late onset disease are consequences of a “triage allocation mechanism†developed during evolution to cope with periods of micronutrient shortage. When micronutrients (vitamins and minerals) are scarce, they are consumed for short-term survival at the expense of long-term survival. In 2009, Children’s Hospital and Research Center Oakland concluded that triage theory explains how diseases associated with aging like cancer, heart disease, and dementia (and the pace of aging itself) may be unintended consequences of mechanisms developed during evolution to protect against episodic vitamin/mineral shortages.
Triage Theory: Linus Pauling Award winner Bruce Ames’ theory that DNA damage and late onset disease are consequences of a “triage allocation mechanism†developed during evolution to cope with periods of micronutrient shortage. When micronutrients (vitamins and minerals) are scarce, they are consumed for short-term survival at the expense of long-term survival. In 2009, Children’s Hospital and Research Center Oakland concluded that triage theory explains how diseases associated with aging like cancer, heart disease, and dementia (and the pace of aging itself) may be unintended consequences of mechanisms developed during evolution to protect against episodic vitamin/mineral shortages.
Triggers: Triggers are discrete entities or events that provoke disease or its symptoms (e.g., microbes). Triggers are usually insufficient in and of themselves for disease formation, however, because the health of the host and the vigor of its response to a trigger are essential elements.
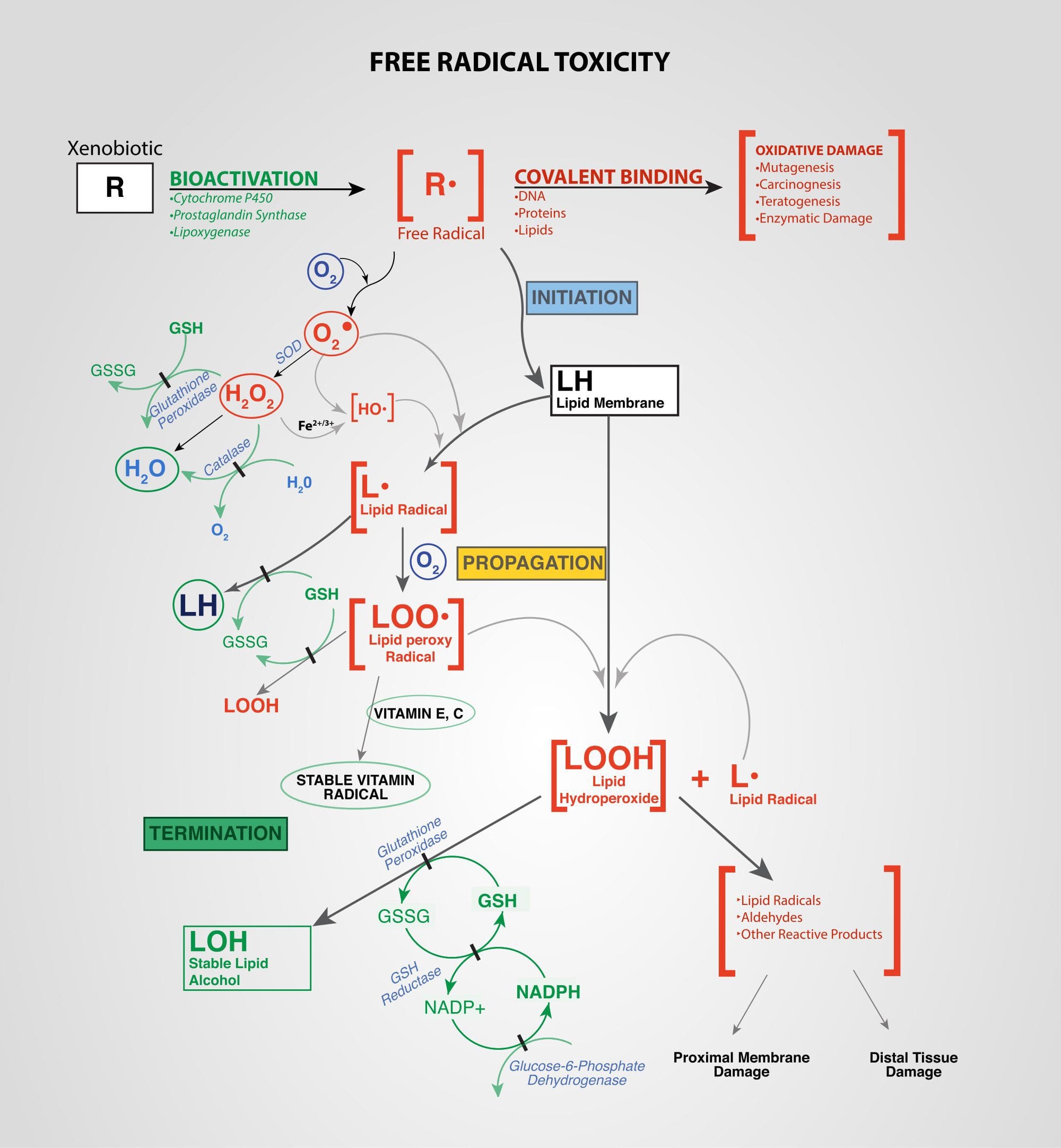 Xenobiotics: Chemicals found in an organism that are not normally produced by or expected to be present in that organism. This may also include substances present in much higher concentrations than usual. The term xenobiotics is often applied to pollutants such as dioxins and polychlorinated biphenyls, because xenobiotics are understood as substances foreign to an entire biological system, i.e. artificial substances that did not exist in nature before their synthesis by humans. Exposure to several types of xenobiotics has been implicated in cancer risk.
Xenobiotics: Chemicals found in an organism that are not normally produced by or expected to be present in that organism. This may also include substances present in much higher concentrations than usual. The term xenobiotics is often applied to pollutants such as dioxins and polychlorinated biphenyls, because xenobiotics are understood as substances foreign to an entire biological system, i.e. artificial substances that did not exist in nature before their synthesis by humans. Exposure to several types of xenobiotics has been implicated in cancer risk.
Functional Medicine: A Healthier You
Post Disclaimer
Professional Scope of Practice *
The information herein on "Functional Medicine: Consolidated Glossary" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.