For individuals experiencing pelvic pain, it could be a disorder of the pudendal nerve known as pudendal neuropathy or neuralgia that leads to chronic pain. The condition can be caused by pudendal nerve entrapment, where the nerve becomes compressed or damaged. Can knowing the symptoms help healthcare providers correctly diagnose the condition and develop an effective treatment plan?
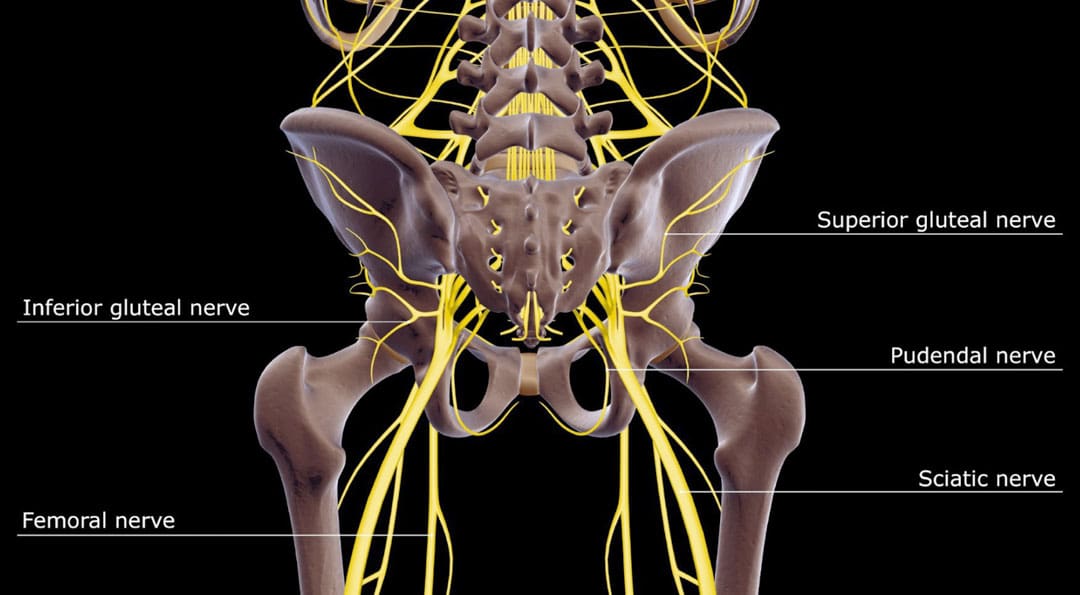
Table of Contents
Pudendal Neuropathy
The pudendal nerve is the main nerve that serves the perineum, which is the area between the anus and the genitalia – the scrotum in men and the vulva in women. The pudendal nerve runs through the gluteus muscles/buttocks and into the perineum. It carries sensory information from the external genitalia and the skin around the anus and perineum and transmits motor/movement signals to various pelvic muscles. (Origoni, M. et al., 2014) Pudendal neuralgia, also referred to as pudendal neuropathy, is a disorder of the pudendal nerve that can lead to chronic pelvic pain.
Causes
Chronic pelvic pain from pudendal neuropathy can be caused by any of the following (Kaur J. et al., 2024)
- Excessive sitting on hard surfaces, chairs, bicycle seats, etc. Bicyclists tend to develop pudendal nerve entrapment.
- Trauma to the buttocks or pelvis.
- Childbirth.
- Diabetic neuropathy.
- Bony formations that push against the pudendal nerve.
- Thickening of ligaments around the pudendal nerve.
Symptoms
Pudendal nerve pain can be described as stabbing, cramping, burning, numbness, or pins and needles and can present (Kaur J. et al., 2024)
- In the perineum.
- In the anal region.
- In men, pain in the scrotum or penis.
- In women, pain in the labia or vulva.
- During intercourse.
- When urinating.
- During a bowel movement.
- When sitting and goes away after standing up.
Because the symptoms are often hard to distinguish, pudendal neuropathy can often be hard to differentiate from other types of chronic pelvic pain.
Cyclist’s Syndrome
Prolonged sitting on a bicycle seat can cause pelvic nerve compression, which can lead to chronic pelvic pain. The frequency of pudendal neuropathy (chronic pelvic pain caused by entrapment or compression of the pudendal nerve) is often referred to as Cyclist’s Syndrome. Sitting on certain bicycle seats for long periods places significant pressure on the pudendal nerve. The pressure can cause swelling around the nerve, which causes pain and, over time, can lead to nerve trauma. Nerve compression and swelling can cause pain described as burning, stinging, or pins and needles. (Durante, J. A., and Macintyre, I. G. 2010) For individuals with pudendal neuropathy caused by bicycling, symptoms can appear after prolonged biking and sometimes months or years later.
Cyclist’s Syndrome Prevention
A review of studies provided the following recommendations for preventing Cyclist’s Syndrome (Chiaramonte, R., Pavone, P., Vecchio, M. 2021)
Rest
- Take breaks at least 20–30 seconds after each 20 minutes of riding.
- While riding, change positions frequently.
- Stand up to pedal periodically.
- Take time off between riding sessions and races to rest and relax the pelvic nerves. 3–10 day breaks can help in recovery. (Durante, J. A., and Macintyre, I. G. 2010)
- If pelvic pain symptoms are barely starting to develop, rest and see a healthcare provider or specialist for an examination.
Seat
- Use a soft, wide seat with a short nose.
- Have the seat level or tilted slightly forward.
- Seats with cutout holes place more pressure on the perineum.
- If numbness or pain is present, try a seat without holes.
Bike Fitting
- Adjust the seat height so the knee is slightly bent at the bottom of the pedal stroke.
- The body’s weight should rest on the sitting bones/ischial tuberosities.
- Keeping the handlebar height below the seat can reduce pressure.
- The Triathlon bike’s extreme-forward position should be avoided.
- A more upright posture is better.
- Mountain bikes have been associated with an increased risk of erectile dysfunction than road bikes.
Shorts
- Wear padded bike shorts.
Treatments
A healthcare provider may use a combination of treatments.
- The neuropathy can be treated with rest if the cause is excessive sitting or cycling.
- Pelvic floor physical therapy can help relax and lengthen the muscles.
- Physical rehabilitation programs, including stretches and targeted exercises, can release nerve entrapment.
- Chiropractic adjustments can realign the spine and pelvis.
- The active release technique/ART involves applying pressure to muscles in the area while stretching and tensing. (Chiaramonte, R., Pavone, P., Vecchio, M. 2021)
- Nerve blocks may help relieve pain caused by nerve entrapment. (Kaur J. et al., 2024)
- Certain muscle relaxers, antidepressants, and anticonvulsants may be prescribed, sometimes in combination.
- Nerve decompression surgery may be recommended if all conservative therapies have been exhausted. (Durante, J. A., and Macintyre, I. G. 2010)
Injury Medical Chiropractic and Functional Medicine Clinic care plans and clinical services are specialized and focused on injuries and the complete recovery process. Our areas of practice include Wellness and nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, severe sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, and Functional Medicine Treatments. If the individual requires other treatment, they will be referred to a clinic or physician best suited for their condition, as Dr. Jimenez has teamed with the top surgeons, clinical specialists, medical researchers, therapists, trainers, and premiere rehabilitation providers.
Pregnancy and Sciatica
References
Origoni, M., Leone Roberti Maggiore, U., Salvatore, S., & Candiani, M. (2014). Neurobiological mechanisms of pelvic pain. BioMed research international, 2014, 903848. https://doi.org/10.1155/2014/903848
Kaur, J., Leslie, S. W., & Singh, P. (2024). Pudendal Nerve Entrapment Syndrome. In StatPearls. https://www.ncbi.nlm.nih.gov/pubmed/31334992
Durante, J. A., & Macintyre, I. G. (2010). Pudendal nerve entrapment in an Ironman athlete: a case report. The Journal of the Canadian Chiropractic Association, 54(4), 276–281.
Chiaramonte, R., Pavone, P., & Vecchio, M. (2021). Diagnosis, Rehabilitation and Preventive Strategies for Pudendal Neuropathy in Cyclists, A Systematic Review. Journal of functional morphology and kinesiology, 6(2), 42. https://doi.org/10.3390/jfmk6020042
Post Disclaimer
Professional Scope of Practice *
The information herein on "Exploring Pudendal Neuropathy: The Impact on Pelvic Health" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.