Table of Contents
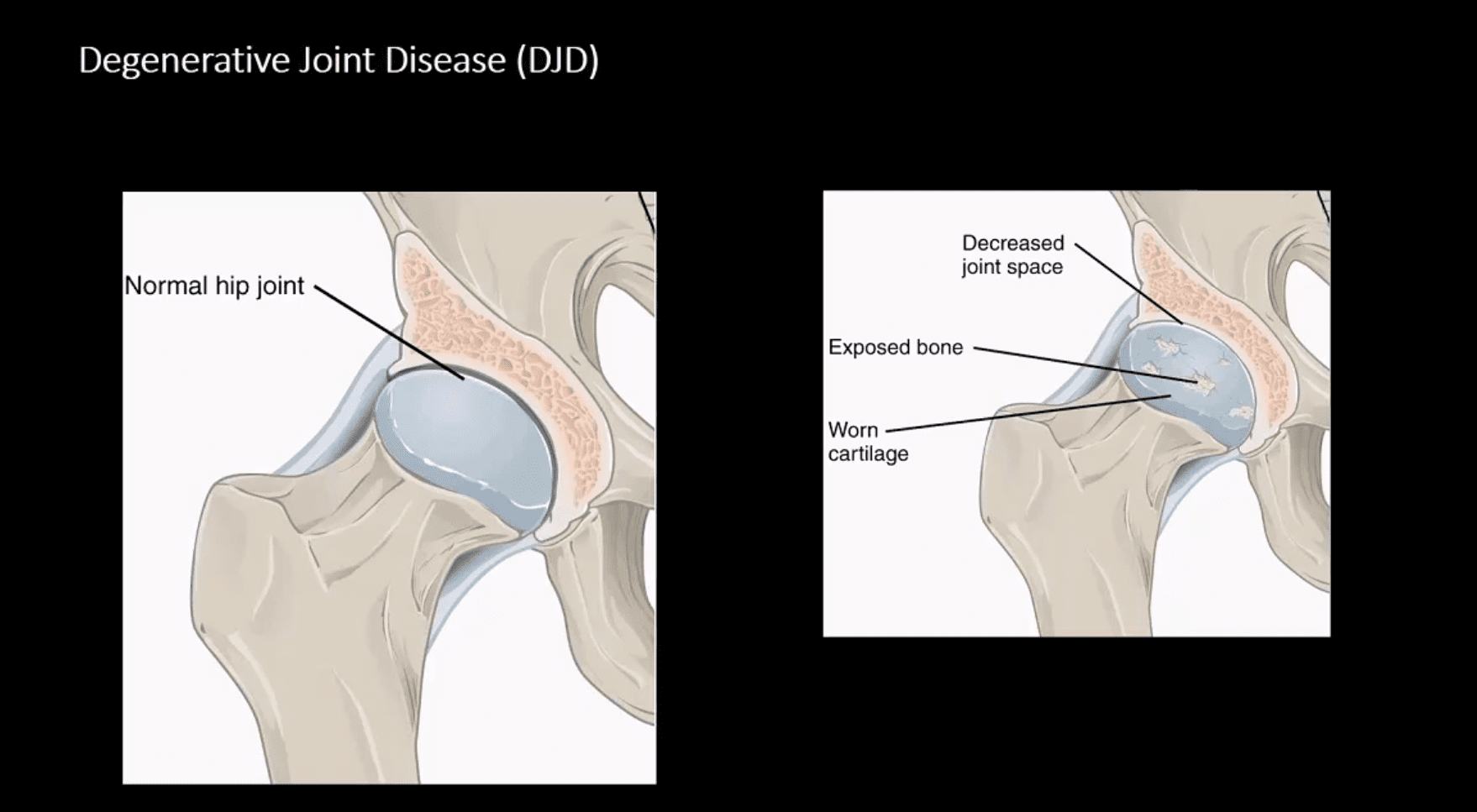
Degenerative Joint Disease (DJD)
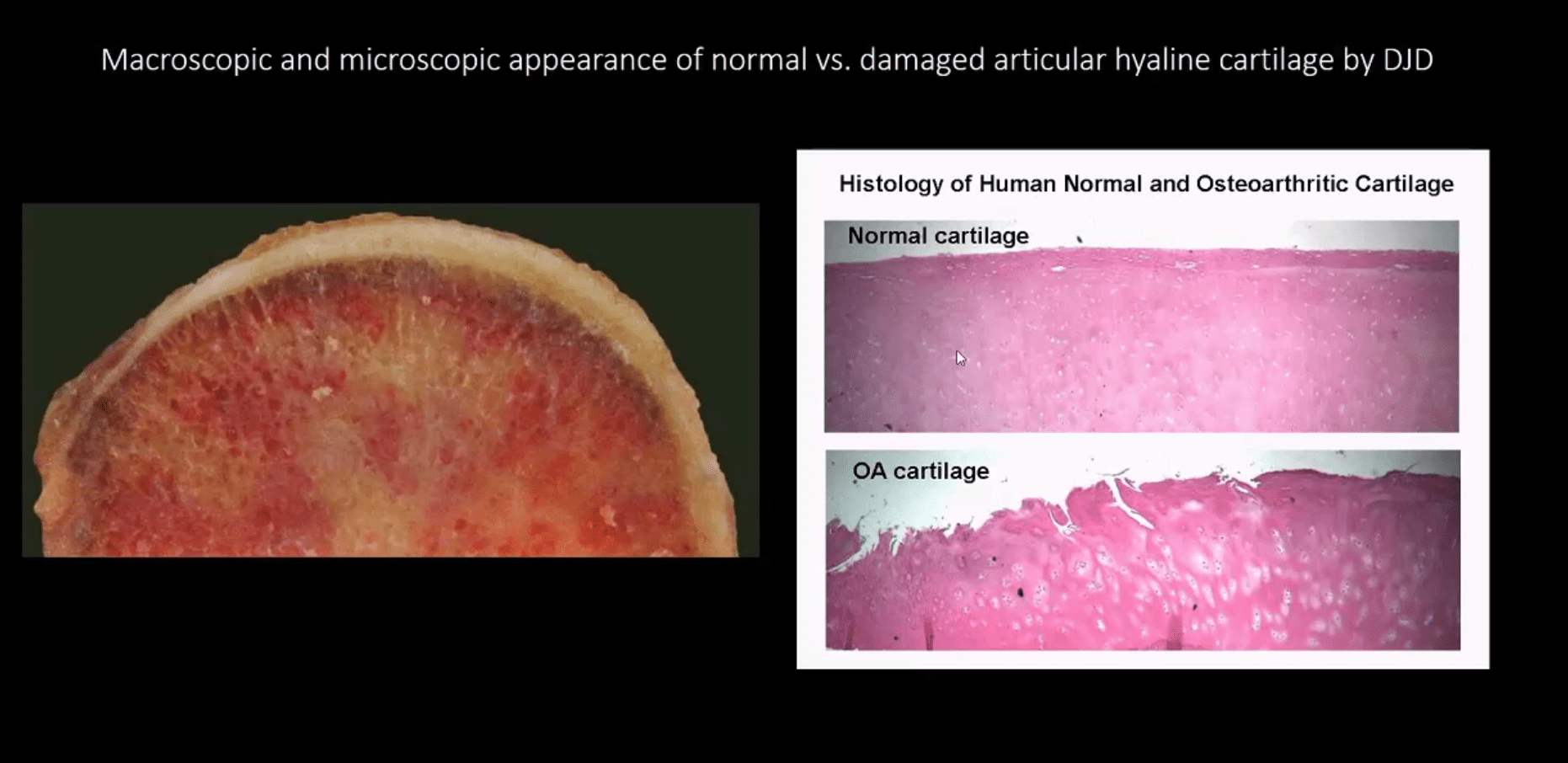
Macroscopic & Microscopic Appearance of Normal vs. Damaged Articular Hyaline Cartilage by DJD
Hip Osteoarthritis (OA) aka Osteoarthrosis
- Symptomatic and potentially disabling DJD
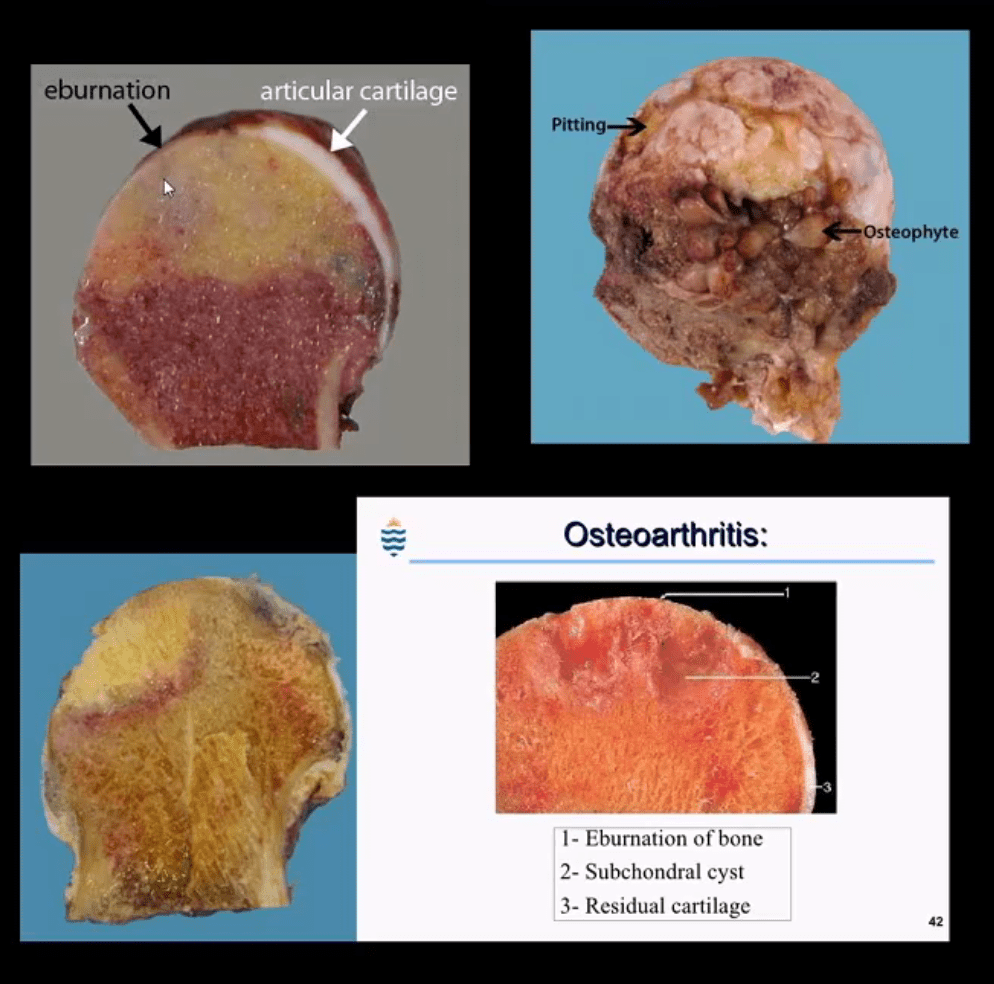
- Progressive damage and loss of the articular cartilage causing denudation and eburnation of articular bone
- Cystic changes, osteophytes and gradual joint destruction
- Develops d/t repeated joint loading and microtrama
- Obesity, metabolic/genetic factors
- Secondary Causes: trauma, FAI syndrome, osteonecrosis, pyrophosphate crystal depostion, previous inflammatory arthritis, Slipped Capital Femoral Epiphysis, Leg-Calves-Perthes disease in children etc.
- Hip OA, 2nd m/c after knee OA. Women>men
- 88-100 symptomatic cases per 100000
Radiography is the Modality of Choice for the Dx and Grading of DJD
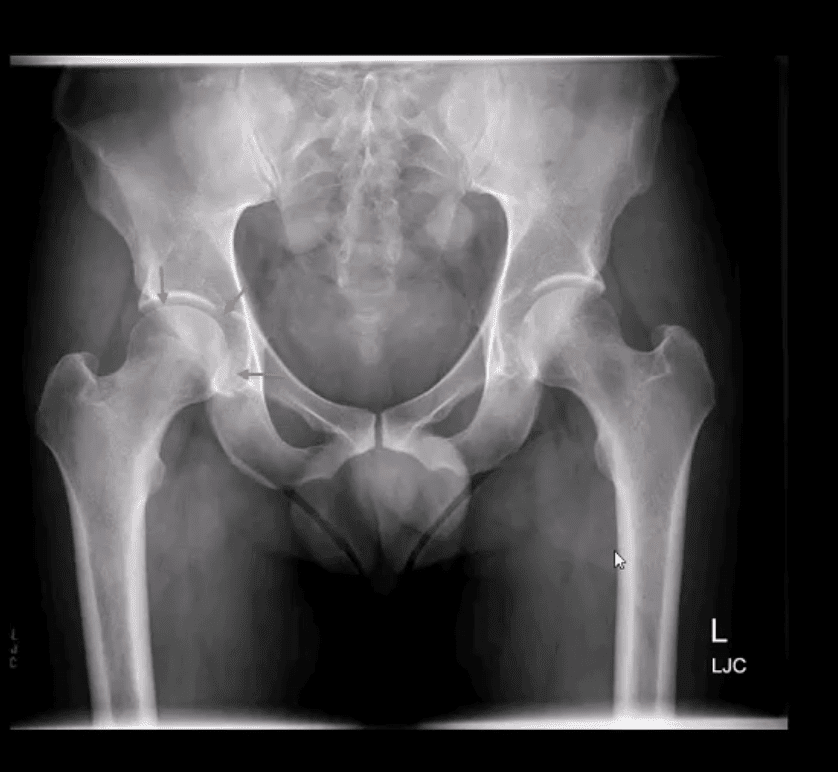
- Special imaging is not required unless other complicating factors exist
- Acetabular-femoral joint is divided into superior, axial and medial compartments/spaces
- Normal joint space at the superior compartment should be 3-4-mm on the AP hip/pelvis view
- Understanding the pattern of hip joint narrowing/migration helps with the DDx of DJD vs. Inflammatory arthritis
- In DJD, m/c hip narrowing is superior-lateral (non-uniform) vs. inflammatory axial (uniform)
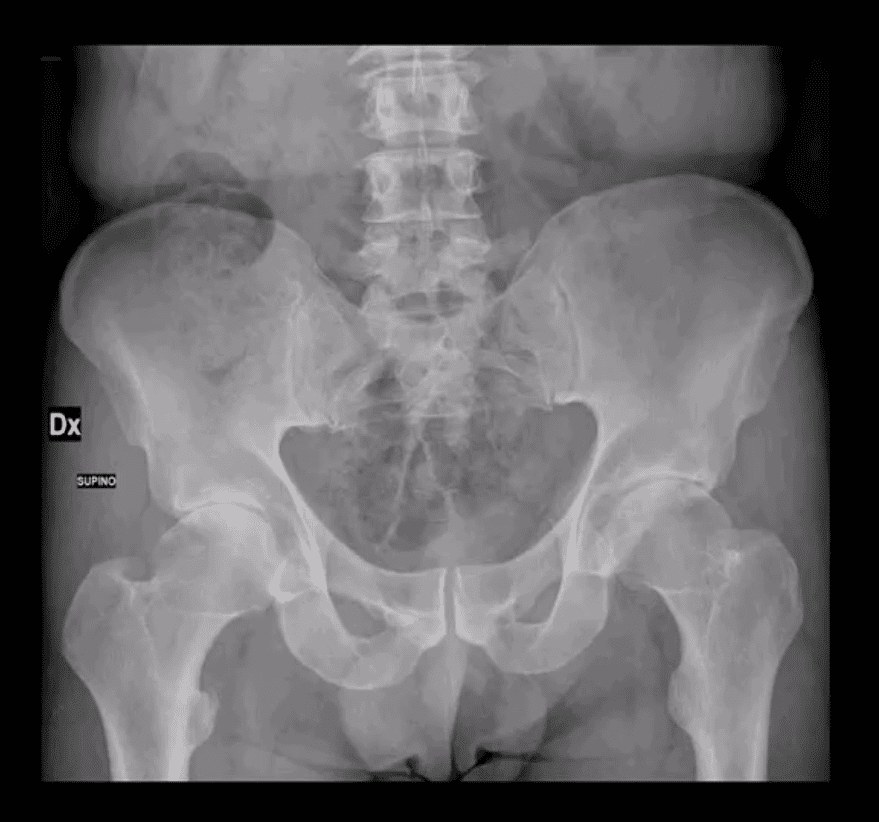
AP Hip Radiograph Demonstrates DJD
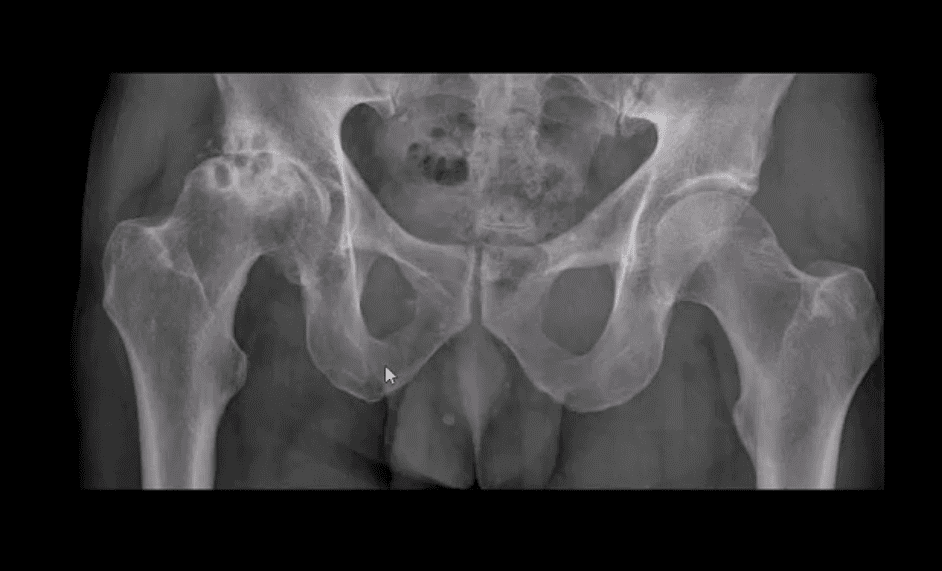
- With
non-uniform loss of joint space (superior migration), large subcortical cysts and subchondral sclerosis - Radiographic features:
- Like with any DJD changes: radiography will reveal L.O.S.S.
- L: loss of joint space (non-uniform or asymmetrical)
- O: osteophytes aka bony proliferation/spurs
- S: Subchondral sclerosis/thickening
- S: Subcortical aka subchondral cysts “geodes”
- Hip migration is m/c superior resulting in a “tilt deformity”
Radiographic Presentation of Hip OA May Vary Depending On Severity
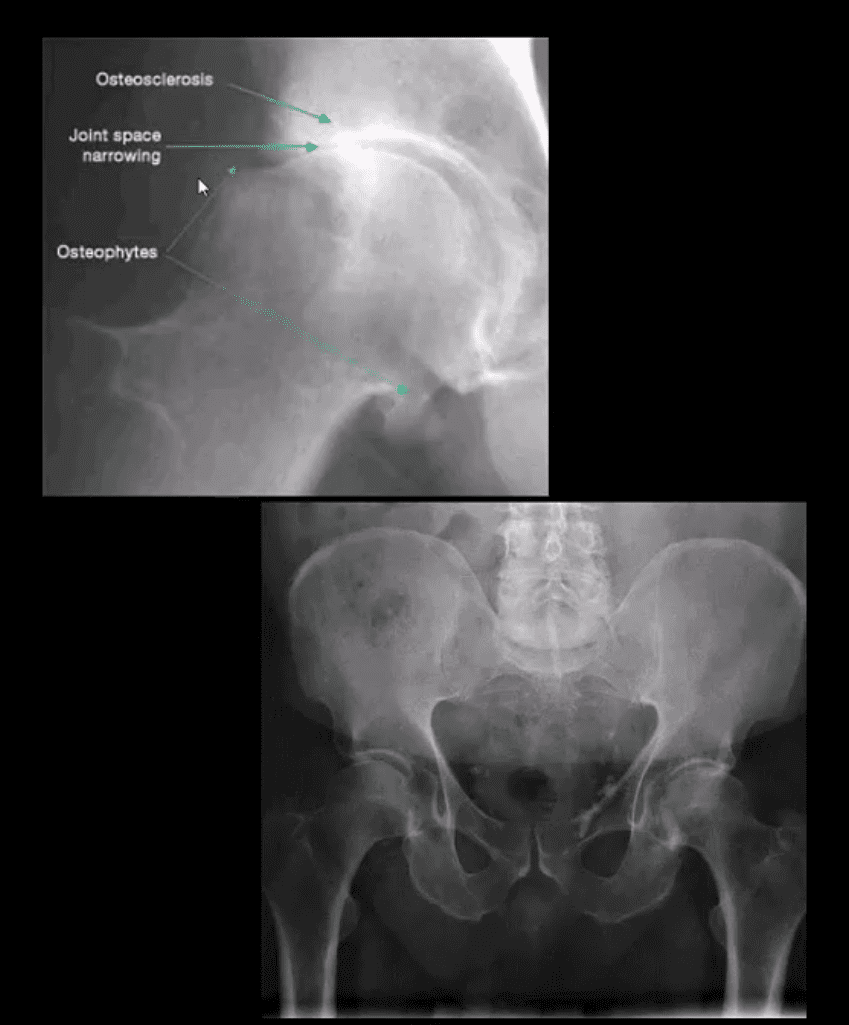
- Mild OA: mild reduction of joint space often w/o marked osteophytes and cystic changes
- During further changes, collar osteophytes may affect femoral head-neck junction with more significant jint space loss and subchondral bone sclerosis (eburnation)
- Cyst formation will often occur along the acetabular and femoral head subarticular/subchondral bone “geodes” and usually filled with joint fluid and some intra-articular gas
- Subchondral cysts may be occasionally very large and DDx from neoplasms or infection or other pahtology
Coronal Reconstructed CT Slices in Bone Window

- Note moderate joint narrowing that appears non-uniform
- Sub-chondral cysts formation (geodes) are noted along the acetabular and femoral head subchondral bone
- Other features include collar osteophytes along head-neck junction
- Dx: DJD of moderate intensity
- Referral to the Orthopedic surgeon will be helpful for this patient
AP Pelvis (below first image), AP Hip Spot (below second image) CT Coronal Slice
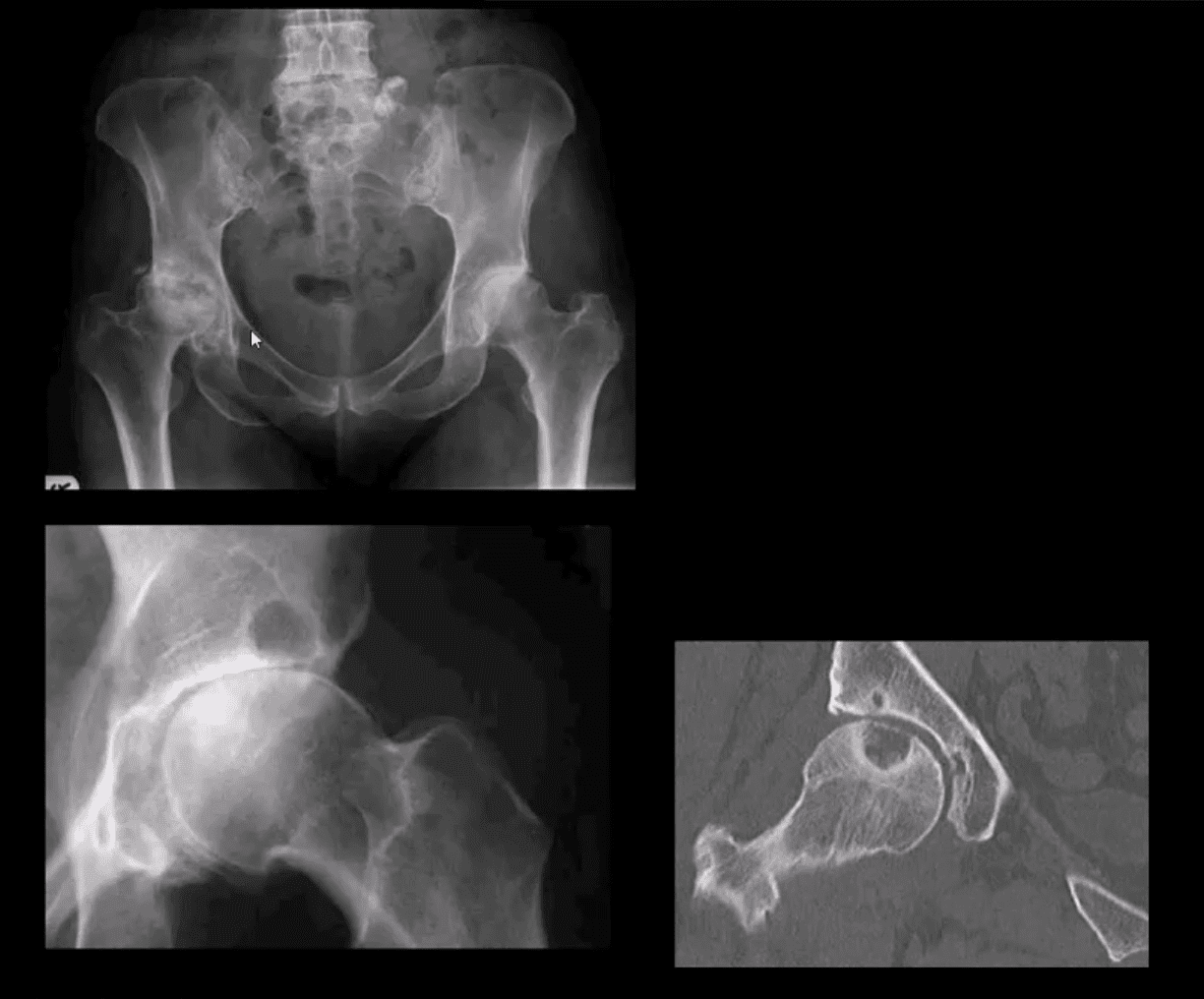
- Note multiple subchondral cysts, sever non-uniform joint narrowing (superior-lateral) and subchondral sclerosis with osteophytes
- Advanced hip arthrosis
Severe DJD, Left Hip
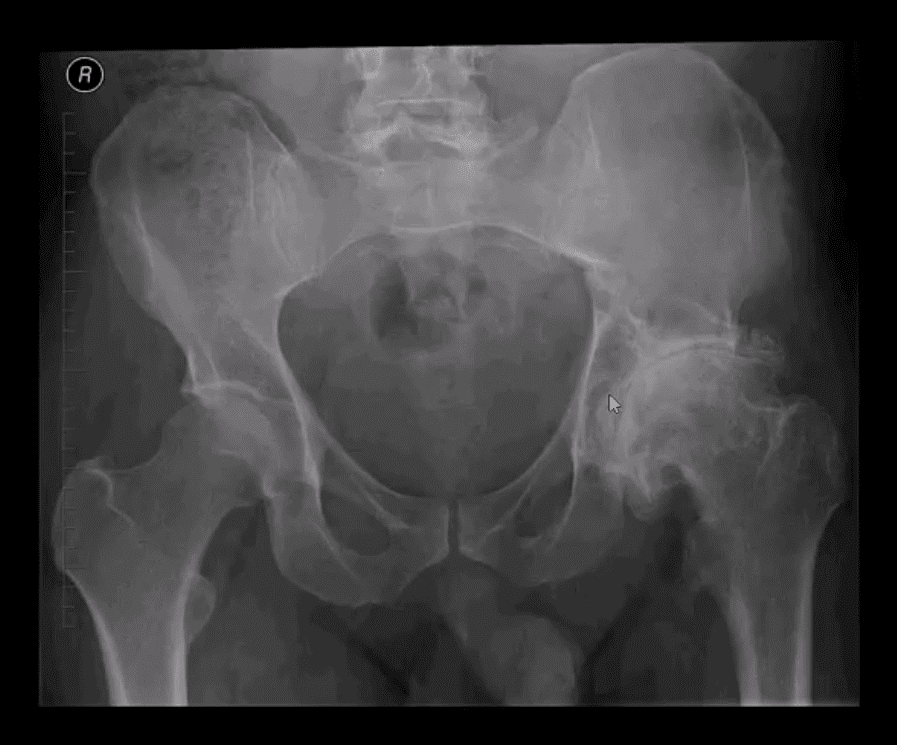
- When reading radiological reports pay particular attention to grading of hip OA
- Most severe (advanced) OA cases require total hip arthroplasty (THA)
- Refer your patients to the Orthopedic surgeon for a consultation
- Most mild cases are good candidate for conservative care
Hip Arthroplasty aka Hip Replacement
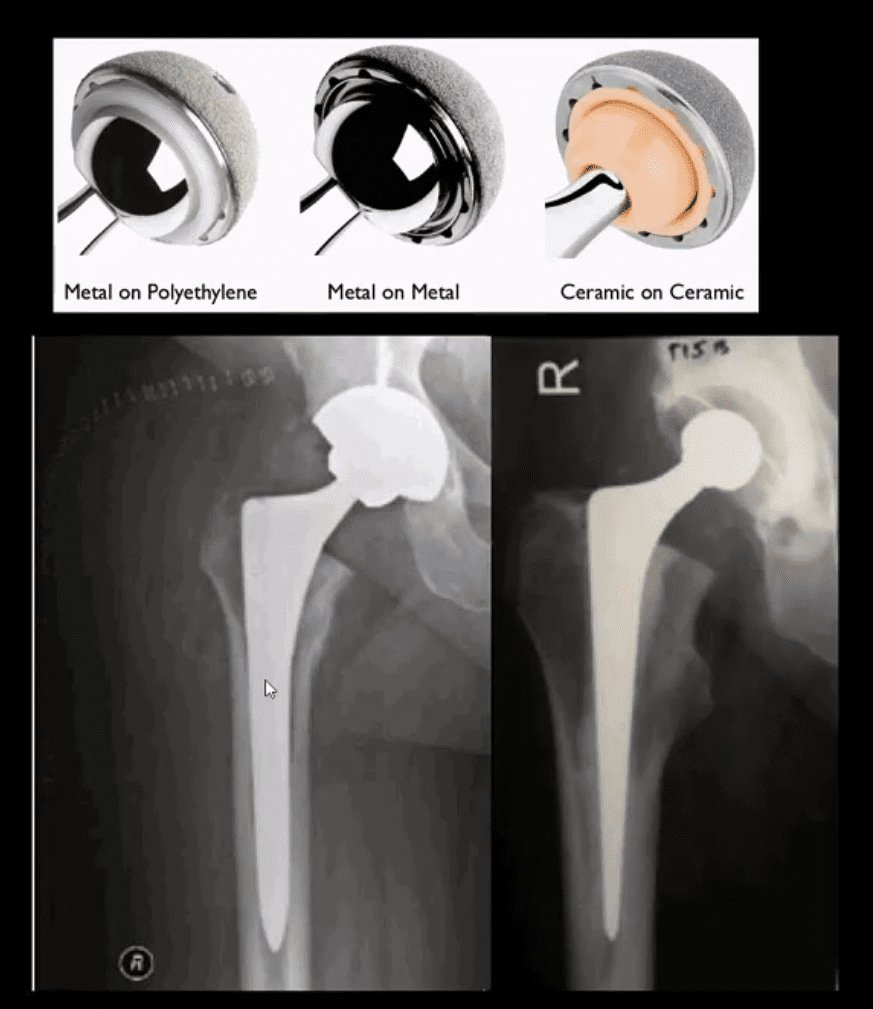
- Can be total or hemiarthroplasty
- THA can be metal on metal, metal on polythelen and ceramic on ceramic
- Hybrid acetabular component with polyethelen and metal backing is also used (above right image)
- THA can be cemented (above right image) and non-cemented (above left image)
- Non-cemented arthroplasty is used on younger patients utilizing porous metallic parts allowing good fusion and bone ingrowth into the prosthesis
Failed THA May Develop
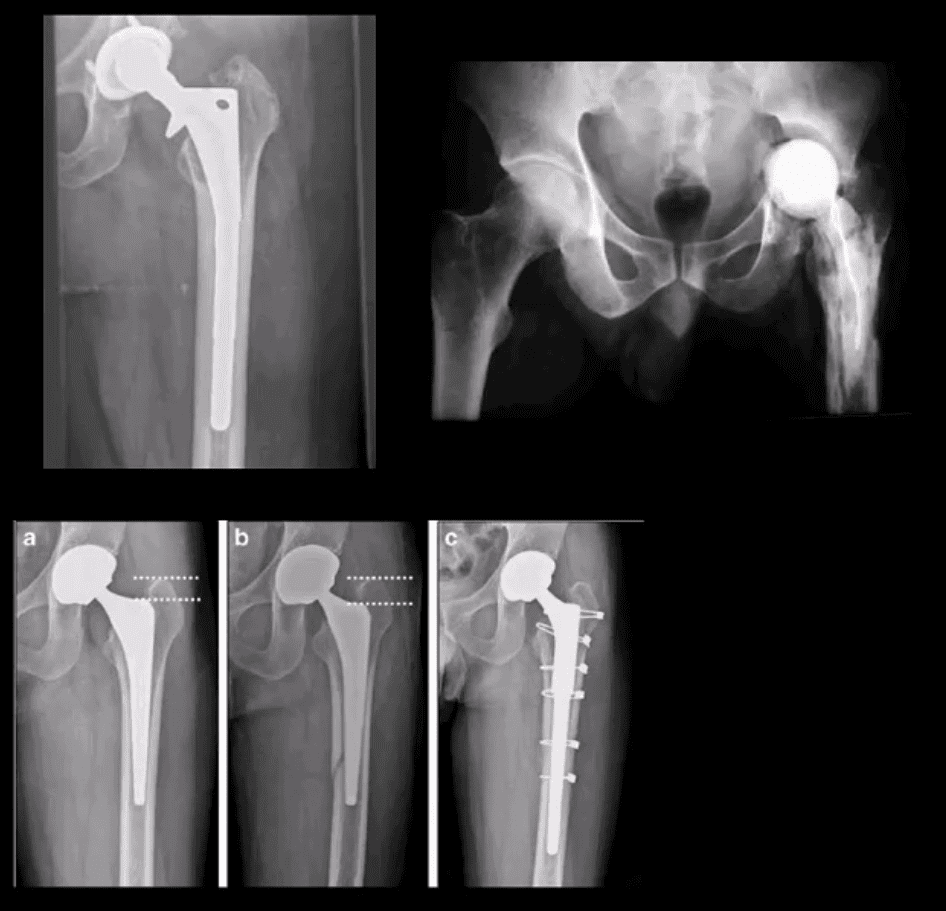
- Most develop within
first year and require revision - Femoral stem may fracture (above left)
- Postsurgical infection (above right)
- Fracture adjacent to prosthesis (stress riser)
- Particle disease
Femoroacetabular Impingement Syndrome
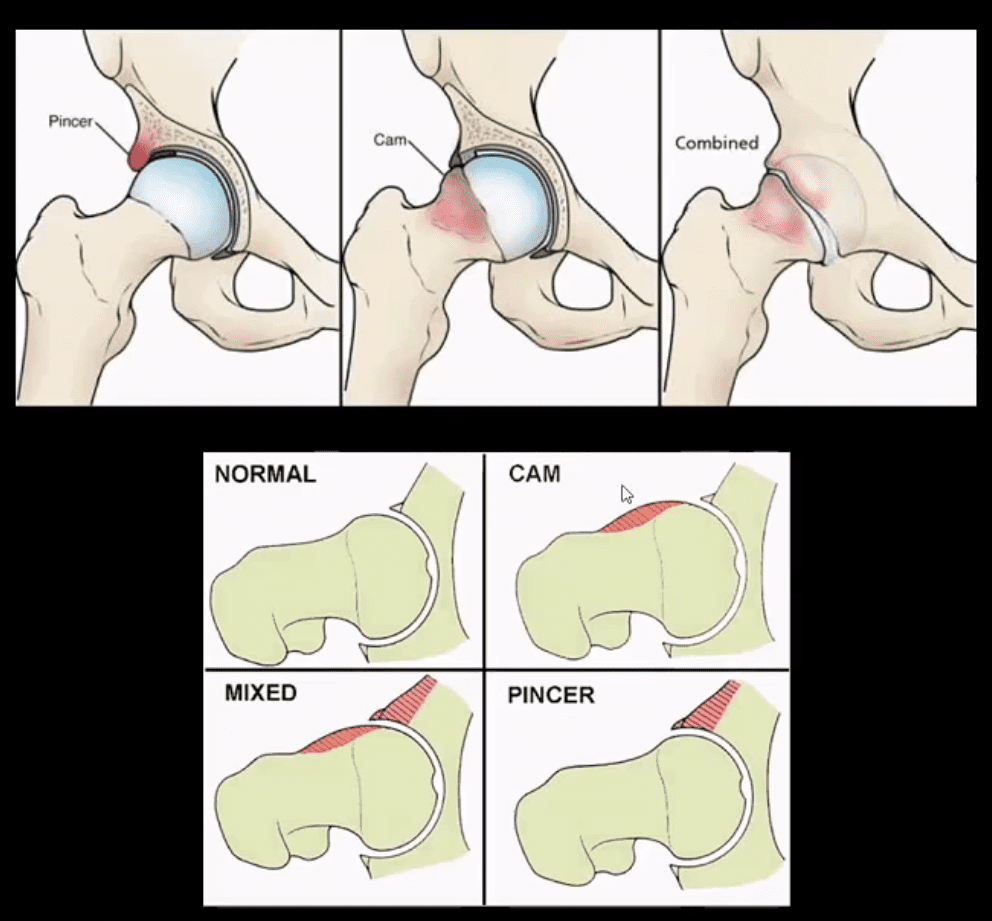
- (FAI): abnormality of normal morphology of the hip leading to eventual cartilage damage and premature DJD
- Clinically: hip/groin pain aggravated by sitting (e.g. hip flexed & externally rotated). Activity related pain on axial loading esp. with hip flexion (e.g. walking uphill)
Pincer type acetabulum: > in middle age women potentially many causes- CAM-type deformity: > in men in 20-50 m/c 30s
- Mixed type (pincer-CAM) is most frequent
- Up until the 90s FAI was not well-recongnised
FAI Syndrome
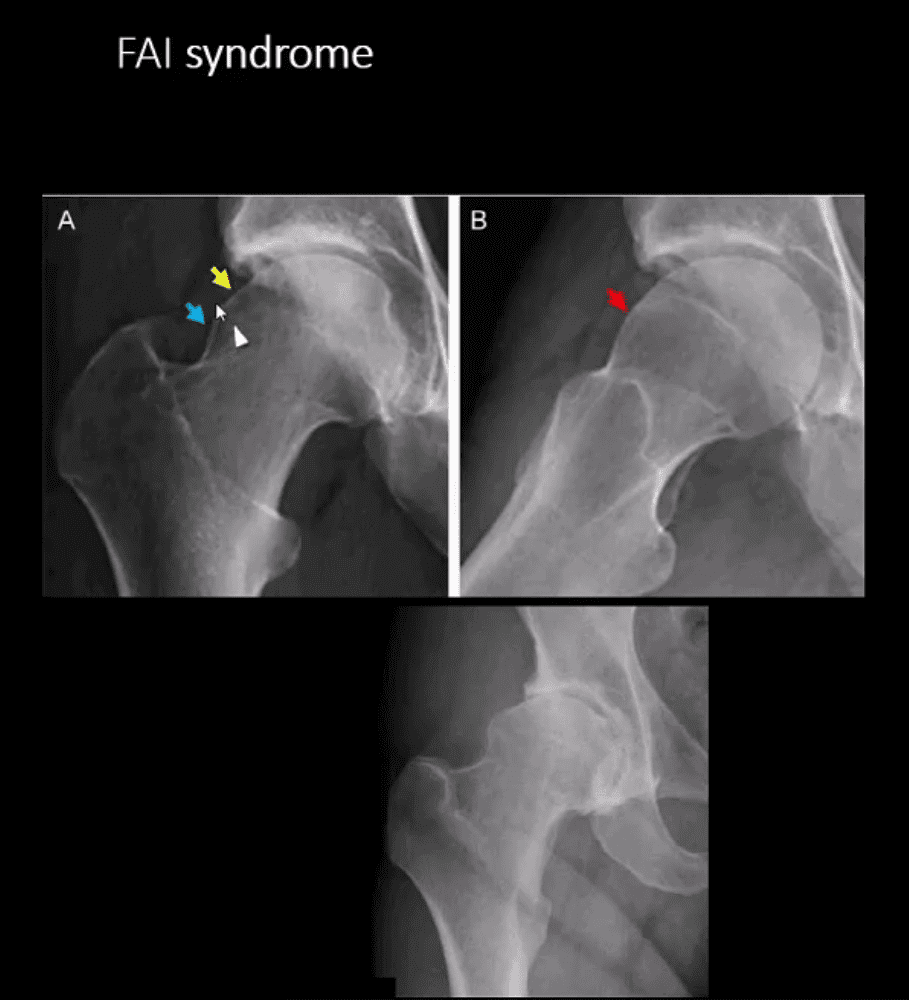
- CAM-type FAI syndrome
- Radiography can be a reliable Dx tool
- X-radiography findings: osseous bump on the lateral aspect of femoral head-neck junction. Pistol-grip deformity. Loss of normal head sphericity. Associated features: os
acetabule , synovial herniation pit (Pit’s pit). Evidence of DJD in advanced cases - MRI and MR arthrography (most accurate Dx of labral tear) can aid the diagnosis of labral tear and other changes of FAI
- Referral to the Orthopedic surgeon is necessary to prevent DJD progression and repair labral abnormalities. Late Dx may lead to irreversible changes of DJD
AP Pelvis: B/L CAM-type FAI syndrome
Pincer-Type FAI with Acetabula Over-Coverage
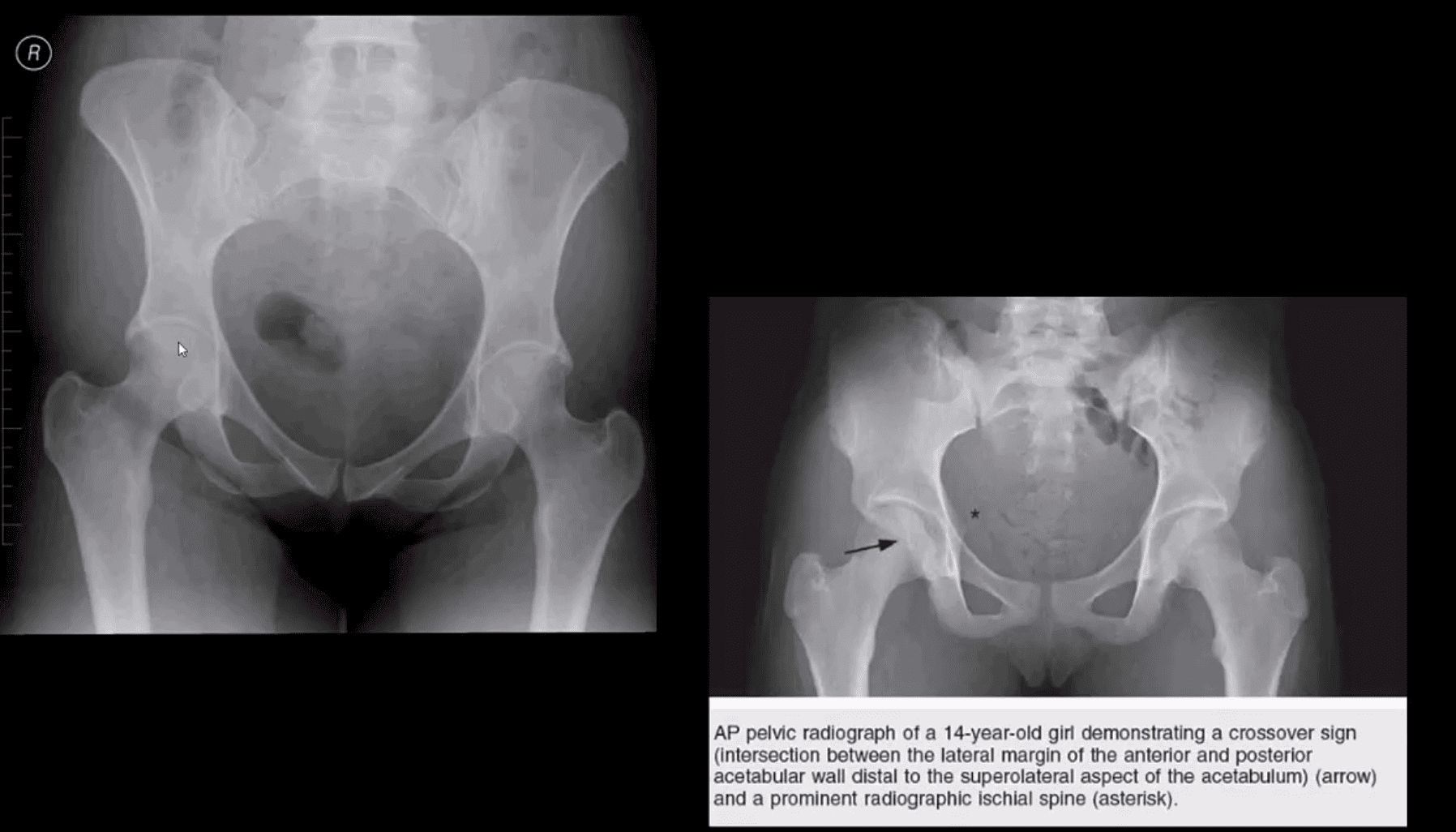
- Key radiographic signs: “Cross-over sign” and abnormal center-edge and Alfa-angle evaluation methods
Dx of FAI
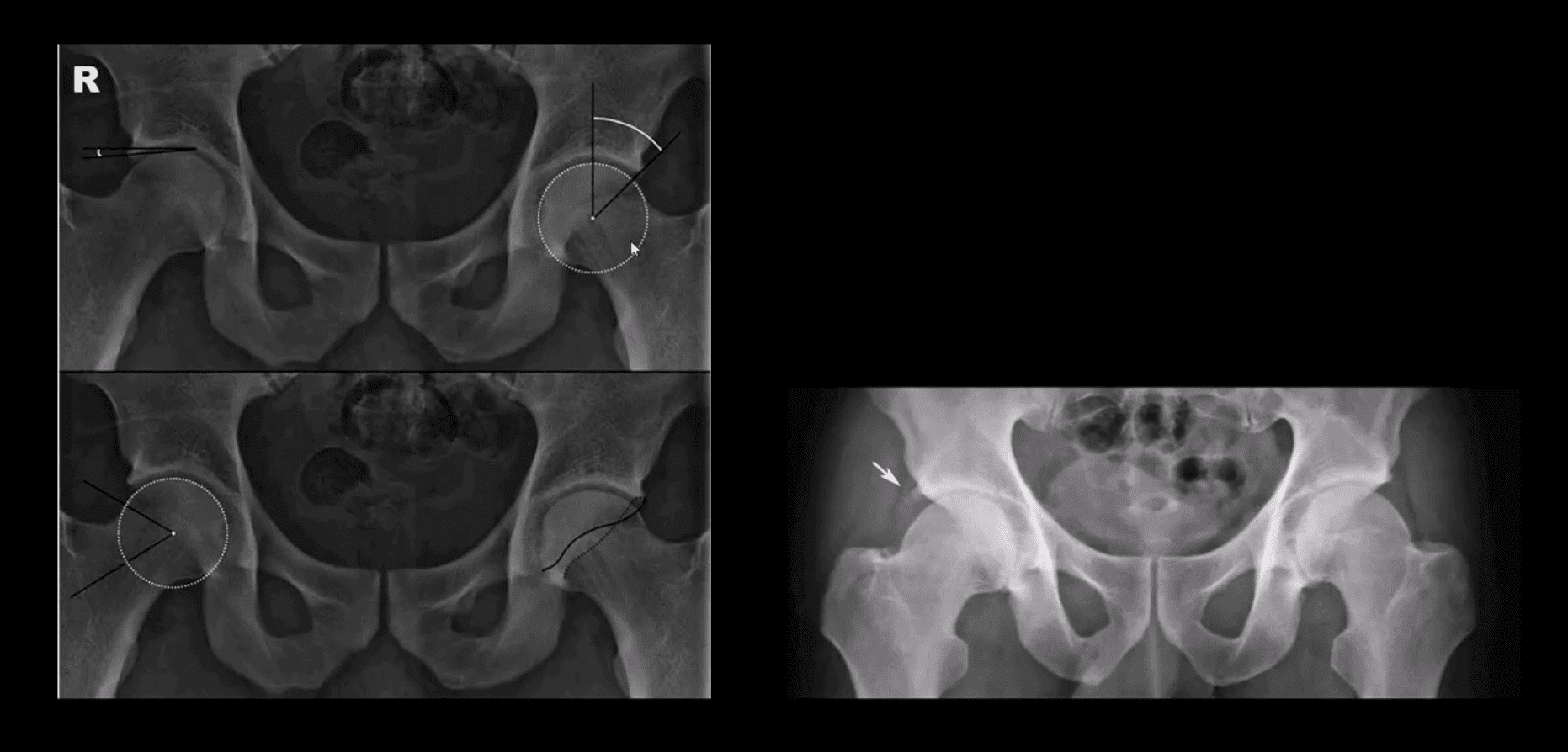
- Center-edge angle (above the first image) and Alfa-angle (above the second image)
- B/L CAM-type FAI with os acetabule (above right image)
MR Arthrography
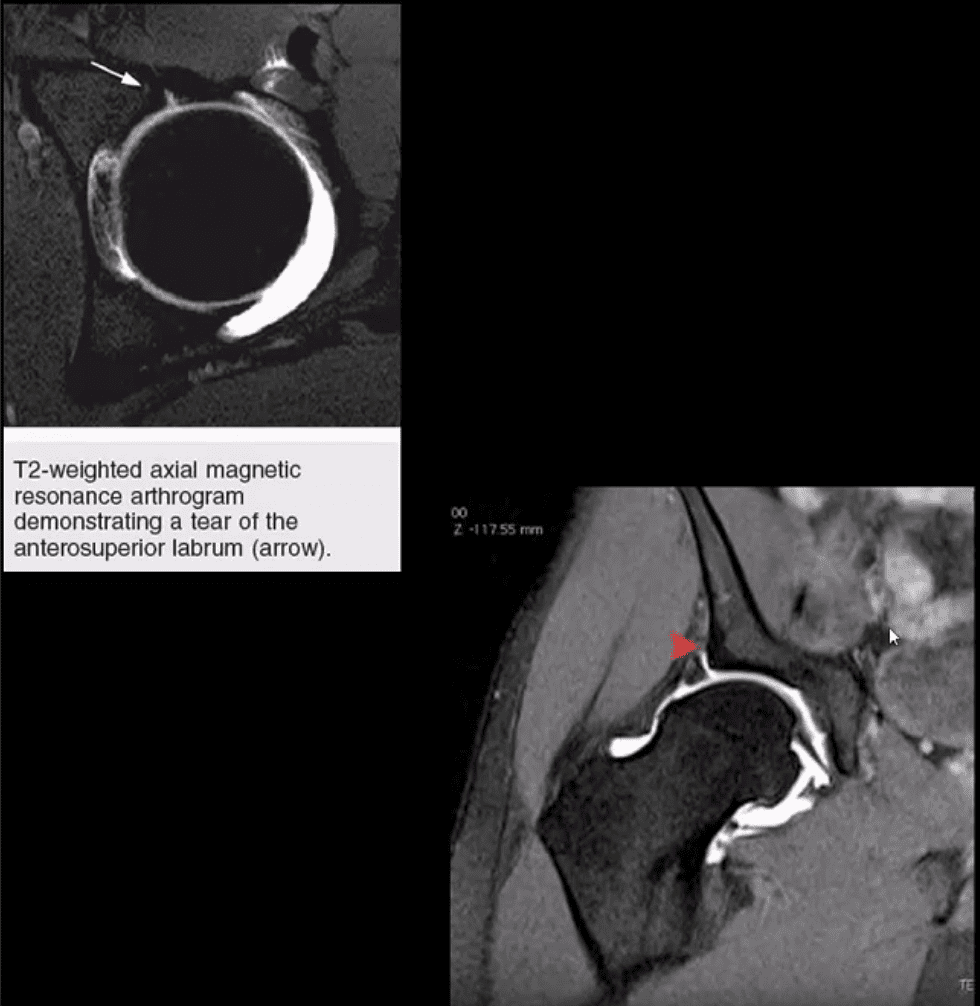
- Labral tear and CAM-type FAI syndrome on axial (above left) and coronal T2 W (above right) MR arthrography
- Note acetabula labral tear. Referral to orthopedic surgeon is required. For more information:
- radiopaedia.org/articles/femoroacetabular-impingment-1
Hip Pelvis Arthritis & Neoplasms
Post Disclaimer
Professional Scope of Practice *
The information herein on "Diagnosis of Hip Complaints: Arthritis & Neoplasms Part I | El Paso, TX." is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Chiropractic Scientist wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.