Claudication is muscle pain that presents when the body is active and stops when the body is at rest, also known as intermittent claudication. Individuals typically report dull aching, cramping, tingling, and/or numbness. Vascular claudication is caused by circulatory problems like poor blood circulation and peripheral artery disease. Still, spinal conditions can also cause neurogenic claudication caused by problems with the spine and nervous system.
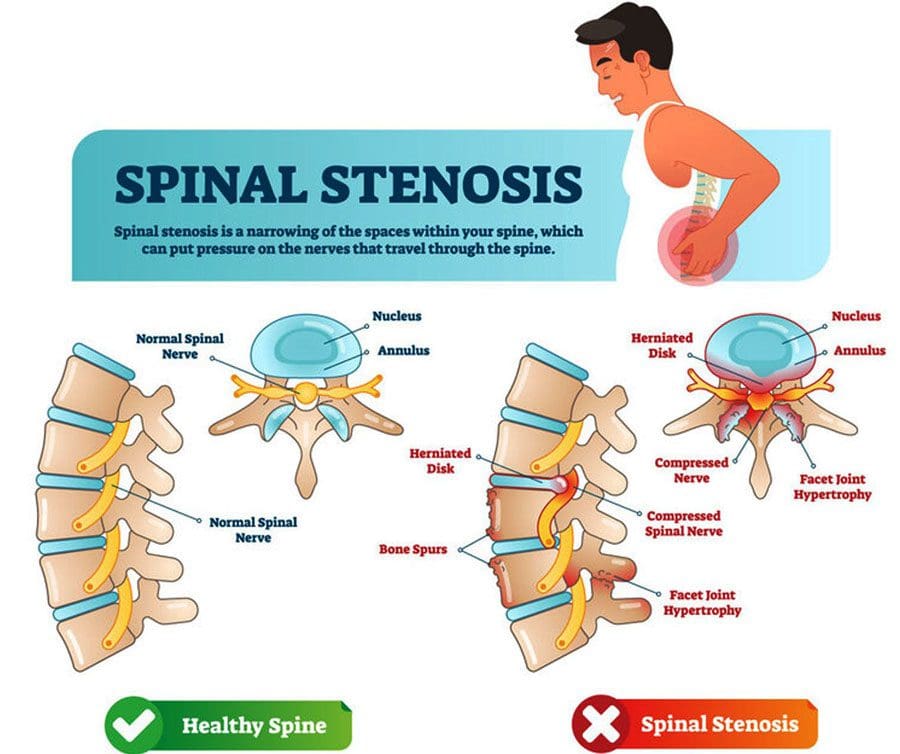
Table of Contents
Neurogenic Claudication
Sciatica is the usual suspect when thigh, hip, buttock, calf, or total leg pain or other sensations are present; however, it could be spinal stenosis with neurogenic claudication. Spinal stenosis is sometimes called pseudo claudication, a narrowing of the space around the low back, which can put pressure on the spinal cord directly and compress the blood vessels around the spine, cutting off oxygen-carrying blood. Pain can start in the lower back and circulate down the legs and cause weakness, tingling, or numbness in the legs and feet. The most common areas of spinal compression include:
- The central spinal canal
- The lateral recess
- The foramen are the openings on the sides of the spine where nerves exit and connect to the peripheral nervous system.
The narrowing can occur in any of these areas, with the most common cause being lumbar spinal stenosis brought on by lumbar degenerative disease.
Symptoms
The most common symptoms of neurogenic claudication include:
- Pain in the lower extremities, including the buttocks, thighs, and calf, only manifests with activities like walking or standing around.
- Pain that shows up equally on both sides.
- There is no pain when sitting or not walking around.
- Radiculopathy or nerve pain that radiates down an affected limb. Sciatica is a typical example.
However, the symptoms of claudication and radiculopathy are different.
- Claudication will be felt all along the length of the nerve.
- Radiculopathy pain is more localized to the buttock, thighs, and calves and can get worse with activity and is generally present even when at rest.
Treatment
Non-surgical treatment of neurogenic claudication includes medication to help control pain, chiropractic manual therapy, non-surgical spinal decompression, physical rehabilitation therapy, and steroid shots to reduce inflammation. A doctor will recommend stretching, strengthening exercises, and types of activities to help improve the body’s ability to support itself. This could include swimming, walking, and stationary cycling. However, conservative treatment might not be an option for individuals with more severe cases. If conservative treatment options don’t work, surgery could be recommended. A healthcare provider can help explain treatment options. Successful outcomes have been seen in cases that are diagnosed and treated early.
Non-Surgical Spinal Decompression Chiropractor
References
Colak, Ahmet, et al. “A less invasive surgical approach in the lumbar lateral recess stenosis: a direct approach to the medial wall of the pedicle.” The European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society vol. 17,12 (2008): 1745-51. doi:10.1007/s00586-008-0801-z
Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. [Updated 2022 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/
Cleveland Clinic. (2021) “Claudication.” https://my.clevelandclinic.org/health/diseases/21972-claudication
Post Disclaimer
Professional Scope of Practice *
The information herein on "Claudication Muscles and Nerves" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.