The body’s nerves are the communication system that carries messages between the brain and the rest of the body. Some nerves transmit messages from the brain to muscles to make the body move, while others relay pain, pressure, or temperature signals. Tiny fibers bundled inside each nerve carry the messages with an outer layer/sheathing that insulates and protects the nerves. The brachial plexus is a network of nerves that send signals from the spinal cord to the shoulders, arms, and hands. A brachial plexus nerve injury occurs when the nerves are over-stretched, compressed, torn, cut, or ripped from the spinal cord.
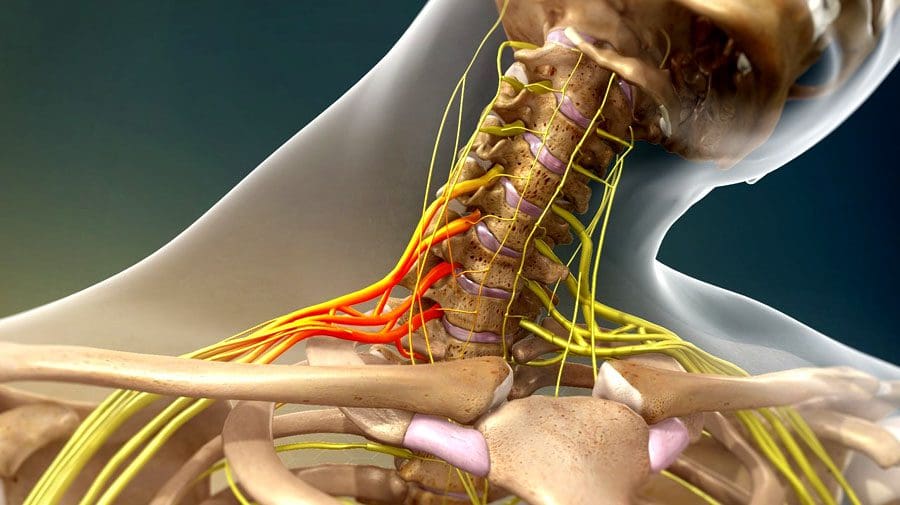
Table of Contents
Brachial Plexus Nerve Injury
The injury involves the head or neck hitting or getting hit and shifting to one side while the shoulder is stretched/pulled in the opposite direction.
- Minor brachial plexus injuries are commonly known as stingers or burners and are common in sports like football, wrestling, hockey, soccer, and basketball.
- Severe brachial plexus injuries can cause arm paralysis and usually result from vehicle or motorcycle accidents.
- Other conditions like inflammation or tumors can affect the brachial plexus.
- Sometimes babies can sustain brachial plexus injuries during birth.
- Pressure and stretching injuries do not physically sever the nerve but can disrupt communication.
- Cutting injuries vary depending on the severity of the cut and because the nerves are in a protective canal that can also be fractured or broken. If the canal remains intact, the nerve fibers could grow back with time.
- However, surgery is necessary to repair the damage if the canal is broken.
- A neuroma/scar tissue can develop if left unrepaired, causing pain.
Symptoms
Signs and symptoms of a brachial plexus nerve injury can vary, depending on the severity and location of the injury. Usually, only one arm is affected.
Minor Injuries
Minor damage comes from over-stretching or mild compression.
- An electric or burning sensation shoots down the arm.
- Numbness and weakness in the arm.
- Neck pain.
- These symptoms usually last for a few seconds or minutes but can linger for days or longer.
Severe Injuries
More severe symptoms result from injuries that impact, tear, or rupture the nerves.
- The most severe injury occurs when the nerve root is torn from the spinal cord.
Symptoms include:
- Intense pain.
- Writhing neck pain.
- Weakness or inability to use specific shoulder, arm, and/or hand muscles.
- Complete lack of movement and feeling in the shoulder, arm, and/or hand.
- Symptoms in both arms.
Complications
With time, most brachial plexus injuries in children and adults heal with minimal long-term damage. But some injuries can cause long-lasting problems that include:
Joint Stiffness
- The joints can stiffen, making movement difficult.
- Healthcare providers often recommend ongoing chiropractic and physical rehabilitation during recovery.
Atrophy
- Nerves regrow slowly and can take some time to completely heal after the injury.
- During that time, lack of use can cause the muscles to break down.
Chronic Pain
- Nerve damage can cause pain signals to be constantly firing.
Numbness
- It can occur in the arm or hand, increasing the risk of worsening the injury or causing new injuries.
Disability
- Recovery from a severe brachial plexus injury depends on age, damage, location, and severity.
- Even with surgery, individuals can experience long-term muscle weakness or paralysis.
Chiropractic Treatment and Rehabilitation
Treatment depends on the severity of the damage. Chiropractic can help realign, rehabilitate, stretch, and strengthen the muscles, nerves, tendons, joints, and ligaments to expedite recovery. For less severe injuries:
- Muscle strengthening and posture exercises help maintain motion.
- Transcutaneous electrical nerve stimulation for pain control.
- Therapeutic massage will stimulate circulation and keep the muscles loose.
For severe injuries:
- Surgery
- Continued chiropractic and physical rehabilitation to maintain thorough circulation, range of motion, and relaxed muscles.
The Brachial Plexus
References
Brucker, J et al. “Brachial plexus birth injury.” The Journal of neuroscience nursing: Journal of the American Association of Neuroscience Nurses vol. 23,6 (1991): 374-80. doi:10.1097/01376517-199112000-00006
Gutkowska, Olga, et al. “Brachial plexus injury after shoulder dislocation: a literature review.” Neurosurgical review vol. 43,2 (2020): 407-423. doi:10.1007/s10143-018-1001-x
Joyner, Benny, et al. “Brachial plexus injury.” Pediatrics in review vol. 27,6 (2006): 238-9. doi:10.1542/pir.27-6-238
Noland, Shelley S et al. “Adult Traumatic Brachial Plexus Injuries.” The Journal of the American Academy of Orthopaedic Surgeons vol. 27,19 (2019): 705-716. doi:10.5435/JAAOS-D-18-00433
Post Disclaimer
Professional Scope of Practice *
The information herein on "Understanding Brachial Plexus Nerve Injury" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.