These assessment and treatment recommendations represent a synthesis of information derived from personal clinical experience and from the numerous sources which are cited, or are based on the work of researchers, clinicians and therapists who are named (Basmajian 1974, Cailliet 1962, Dvorak & Dvorak 1984, Fryette 1954, Greenman 1989, 1996, Janda 1983, Lewit 1992, 1999, Mennell 1964, Rolf 1977, Williams 1965).
Table of Contents
Clinical Application of Neuromuscular Techniques: Pectoralis Major and Latissimus Dorsi
Assessment of Shortened Pectoralis Major and Latissimus Dorsi
Latissimus and pectoral test (a) Observation is as accurate as most palpation for evidence of pectoralis major shortening. The patient will have a rounded shoulder posture – especially if the clavicular aspect is involved.
Or
The patient lies supine with upper arms on the table, hands resting palm down on the lower abdomen. The practitioner observes from the head and notes whether either shoulder is held in an anterior position in relation to the thoracic cage. If one or both shoulders are forward of the thorax, pectoralis muscles are short (Fig. 4.24).
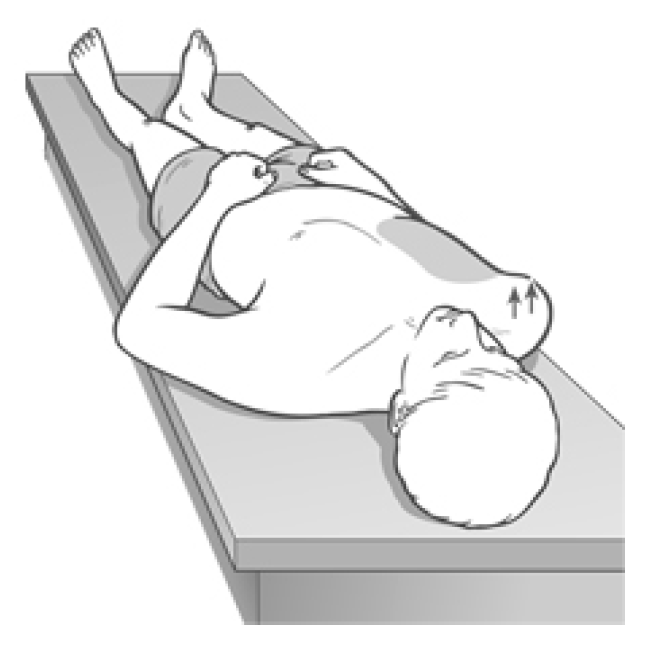
Figure 4.24 Observation assessment in which pectoral shortness on the right is suggested by the inability of the shoulder to rest on the table.
Latissimus and pectoral test (b) The patient lies supine with the head several feet from the top edge of the table, and is asked to rest the arms, extended above the head, on the treatment surface, palms upwards (Fig. 4.25).

Figure 4.25 Assessment of shortness in pectoralis major and latissimus dorsi. Visual assessment is used: if the arm on the tested side is unable to rest along its full length, shortness of pectoralis major is probable; if there is obvious deviation of the elbow laterally, probable latissimus shortening is indicated.
If these muscles are normal, the arms should be able to easily reach the horizontal when directly above the shoulders, and also to be in contact with the surface for almost all of the length of the upper arms, with no arching of the back or twisting of the thorax.
If either arm cannot reach the vertical above the shoulder, but is held laterally, elbow pulled outwards, then latissimus dorsi is probably short on that side. If an arm cannot rest with the dorsum of the upper arm in contact with the table surface without effort, then pectoral fibres are almost certainly short.
Pectoralis major test. Assessment of shortness in pectoralis major (Fig. 4.26) Assessment of the subclavicular portion of pectoralis major involves abduction of the arm to 90° (Lewit 1985b). In this position the tendon of pectoralis major at the sternum should not be found to be unduly tense, even with maximum abduction of the arm, unless the muscle is short.
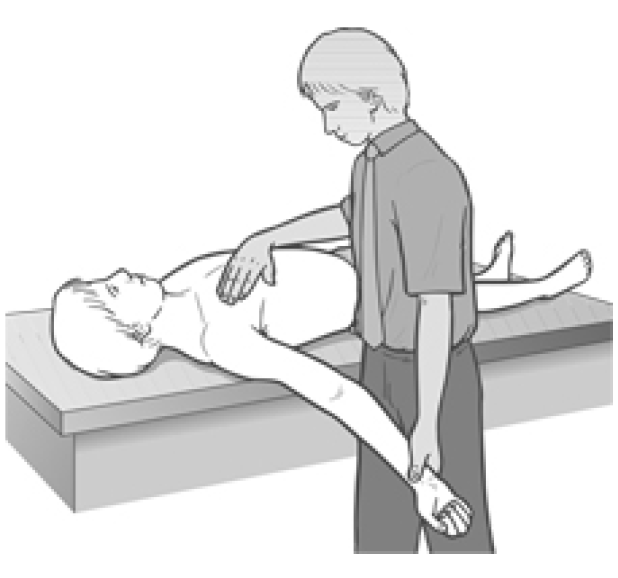
Figure 4.26 Palpation assessment for shortness of subclavicular portion of pectoralis major.
For assessment of sternal attachment the arm is brought into elevation and abduction as the muscle, as well as the tendon on the greater tubercle of the humerus, is palpated. If the sternal fibres have shortened, tautness will be visible and tenderness of the tissues under palpation will be reported.
Pectoralis Major Test: Assessment for Strength of Pectoralis Major
Patient is supine with arm in abduction at the shoulder joint and medially rotated (palm is facing down) with the elbow extended. The practitioner stands at the head and secures the opposite shoulder with one hand to prevent any trunk torsion and contacts the dorsum of the distal humerus, on the tested side, with the other.
The patient attempts to lift the arm and to adduct it across the chest, against resistance, as strength is assessed in the sternal fibres.
Different arm positions can be used to assess clavicular and costal fibres: for example with an angle of abduction/elevation of 135° costal and abdominal fibres will be involved; with abduction/elevation of 45° the clavicular fibres will be assessed. The practitioner should palpate to ensure that the ‘correct’ fibres contract when assessments are being made.
If this postural muscle tests as weak it may be useful to use Norris’s (1999) approach of strengthening it by means of a slowly applied isotonic eccentric (isolytic) contraction, before proceeding to an MET stretching procedure.
MET Treatment of Short Pectoralis Major
Pectoralis major MET method (a) (Fig. 4.27A, B) The patient lies supine with the arm abducted in a direction which produces the most marked evidence of pectoral shortness (assessed by palpation and visual evidence of the particular fibres involved as described in tests above). The more elevated the arm (i.e. the closer to the head), the more focus there will be on costal and abdominal fibres. With a lesser degree of abduction (to around 45°), the focus is more on the clavicular fibres. Between these two extremes lies the position which influences the sternal fibres most directly.

Figure 4.27A MET treatment of pectoral muscle – abdominal attachment. Note that the fibres being treated are those which lie in line with the long axis of the humerus.
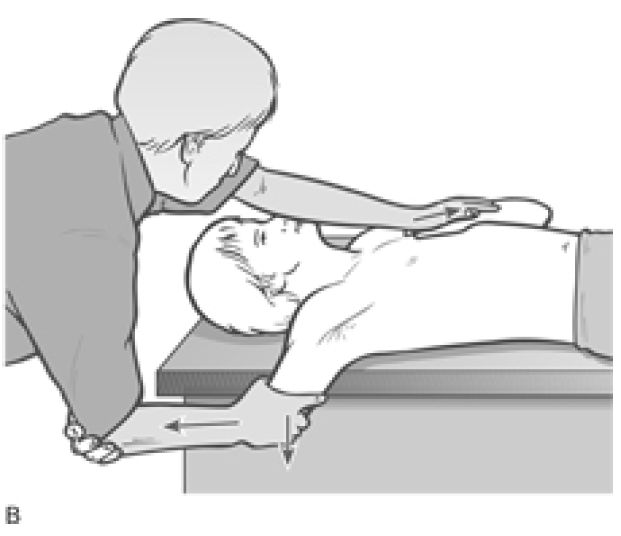
Figure 4.27B An alternative hold for application of MET to pectoral muscle – sternal attachment. Note that the patient needs to be close to the edge of the table in order to allow the arm to be taken towards the floor once the slack has been removed, during the stretching phase after the isometric contraction.
The patient lies as close to the side of the table as possible so that the abducted arm can be brought below the horizontal level in order to apply gravitational pull and passive stretch to the fibres, as appropriate. The practitioner stands on the side to be treated and grasps the humerus.
A useful arm hold, which depends upon the relative size of the patient and the practitioner, involves the practitioner grasping the anterior aspect of the patient’s flexed upper arm just above the elbow, while the patient cups the practitioner’s elbow and holds this contact throughout the procedure (see Fig. 4.27B).
The patient’s hand is placed on the contact (attachments of shortened fibres) area on the thorax so that the hand acts as a ‘cushion’. This is both more physically comfortable and also prevents physical contact with emotionally sensitive areas such as breast tissue. The practitioner’s thenar or hyperthenar eminence is placed over the patient’s ‘cushion’ hand in order to stabilise the area during the contraction and stretch, preventing movement of it.
Commencing with the patient’s arm in a position which takes the affected fibres to just short of their restriction barrier (for a chronic problem), the patient introduces a light contraction (20% of strength) involving adduction against resistance from the practitioner, for 7–10 seconds.
As a rule the long axis of the patient’s upper arm should be in a straight line with the fibres being treated. If a trigger point has previously been identified in pectoralis, the practitioner should ensure – by means of palpation if necessary, or by observation – that the fibres housing the triggers are involved in the contraction.
As the patient exhales following complete relaxation of the area, a stretch through the new barrier is activated by the patient and maintained by the practitioner. Stretch is achieved via the positioning and leverage of the arm as the contact hand on the thorax acts as a stabilising point only.
The stretch needs to be one in which the arm is first pulled away (distracted) from the thorax, with the patient’s assistance (‘ease your arm away from your shoulder’), before the stretch is introduced which involves the humerus being taken below the horizontal (‘ease your arm towards the floor’).
During the stretching phase it is important for the entire thorax to be stabilised. No rolling or twisting of the thorax in the direction of the stretch should be permitted. The stretching procedure should be thought of as having two phases: first the slack being removed by distracting the arm away from the contact/stabilising hand on the thorax; second, movement of the arm towards the floor, initiated by the practitioner bending his knees.
Stretching (after an isometric contraction) should be repeated two or three times in each position. All attachments should be treated, which calls for the use of different arm positions, as discussed above, each with different stabilising (‘cushion’) contacts as the various fibre directions and attachments are isolated.
Pectoralis major MET method (b) (Fig. 4.28) The patient is prone with face in a face hole or cradle. Her right arm is abducted to 90° and the elbow flexed to 90° palm towards the floor, with the upper arm supported by the table. The practitioner stands at waist level, facing cephalad, and places his non-table-side hand palm to palm with the patient’s so that the patient’s forearm is in contact with the ventral surface of the practitioner’s forearm. The practitioner’s table-side hand rests on the patient’s right scapula area, ensuring that no trunk rotation occurs.
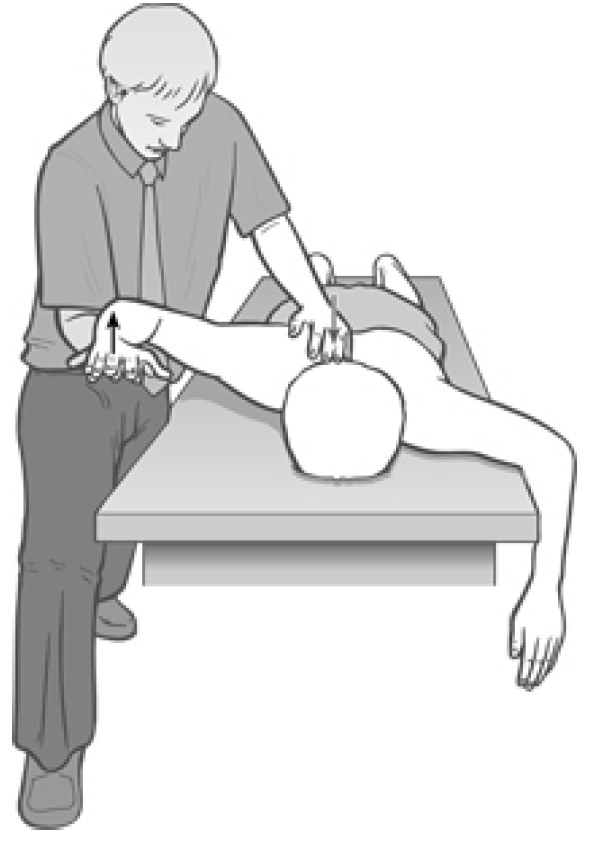
Figure 4.28 MET for pectoralis major in prone position.
The practitioner eases the patient’s arm into extension at the shoulder until he senses the first sign of resistance from pectoralis. It is important when extending the arm in this way to ensure that no trunk rotation occurs and that the anterior surface of the shoulder remains in contact with the table throughout.
The patient is asked, using no more than 20% of strength, to bring her arm towards the floor and across her chest, with the elbow taking the lead in this attempted movement, which is completely resisted by the practitioner. The practitioner ensures that the patient’s arm remains parallel with the floor throughout the isometric contraction.
Following release of the contraction effort, and on an exhalation, the arm is taken into greater extension, with the patient’s assistance, and held at stretch for not less than 20 seconds.
This procedure is repeated two or three times, slackening the muscle slightly from its end-range before each subsequent contraction to reduce discomfort and for ease of application of the contraction.
Variations in pectoralis fibre involvement can be achieved by altering the angle of abduction – with a more superior angle (around 140°) the lower sternal and costal fibres, and with a lesser angle (around 45°) the clavicular fibres will be committed.
Pectoralis major MET method (c) Bilateral MET stretching of pectoralis major (sternocostal aspects) involves having the patient supine, knees and hips flexed, in order to provide stability to the spinal regions, preventing lumbar lordosis. A shallow but firm cushion should be placed between the scapulae, allowing a better excursion of the shoulders during this stretch. The chin should be tucked in and, if more comfortable, a small cushion placed under the neck. Ideally a strap/belt should be used to fix the thorax to the table, but this is not essential.
The practitioner stands at the head of the table and grasps the patient’s elbows or forearms, which are flexed, laterally rotated and held in a position to induce the most taut aspects of the muscles to become prominent.
Starting from such a barrier or short of it (acute/chronic), the patient is asked to contract the muscles by bringing the arms upwards and towards the table for 10 seconds or so during a held breath.
Following the contraction and complete relaxation, the arms are taken to a new or through the restriction barrier, as appropriate, during an exhalation. Repeat as necessary several times more.
Pectoralis major MET method (d) By adopting the same positions – but with the arms of the patient more laterally placed so that they are laterally rotated and in 90° abduction from the shoulder (upper arms are straight out sideways from the shoulder) and there is 90° flexion at the elbows, with the practitioner contacting the area just proximal to the flexed elbows – a more direct stretch of the clavicular insertions of the muscle can be achieved, using all the same contraction and stretch elements as in (b) above.
Latissimus Dorsi Test for Shortness
To screen latissimus dorsi (12), the standing patient is asked to bend forwards and allow the arms to hang freely from the shoulders as she holds a half-bend position, trunk parallel with the floor.
If the arms are hanging other than perpendicular to the floor there is probably some muscular restriction involved, and if this involves latissimus the arms will be held closer to the legs than perpendicular (if they hang markedly forward of such a position then trapezius shortening is probable, see below).
To screen latissimus in this position, one side at a time, the practitioner stands in front of the patient (who remains in this half-bend position) and, stabilising the scapula area with one hand, grasps the arm at elbow level and gently draws the tested side (straight) arm forwards. It should, without undue effort or excessive bind in the tissues being held, allow itself to be taken to a position where the elbow is higher than the level of the back of the head. If this is not possible, then latissimus is short.
MET Treatment of Short Latissimus Dorsi
Short latissimus dorsi MET method (a) The patient lies supine with the feet crossed (the side to be treated crossed under the non-treated side leg at the ankle). The patient is arranged in a light sidebend away from the side to be treated so that the pelvis is towards that side, and the feet and head away from that side. The heels are placed just off the edge of the table, so anchoring the lower extremities.
The patient places her arm on the side to be treated behind her neck, as the practitioner, standing on the side opposite that to be treated, slides his cephalad hand under the patient’s shoulders to grasp the treated side axilla. The patient grasps the practitioner’s cephalad arm at the elbow, making this contact more secure. The patients treated side elbow should point superiorly. The practitioner’s caudad hand is placed on the anterior superior iliac spine on the side being treated.
The patient is instructed to very lightly take the pointed elbow towards the sacrum and also to lightly try to bend backwards and towards the treated side. This should produce a light isometric contraction in latissimus dorsi on the side to be treated. After 7 seconds they are asked to relax completely as the practitioner transfers his body weight from the cephalad leg to the caudad leg, to sidebend the patient. Simultaneously the practitioner stands more erect and leans in a caudad direction.
This effectively lifts the patient’s thorax from the table surface and introduces a stretch into latissimus (especially if the patient has maintained a grasp on the practitioner’s elbow and the practitioner has a firm hold on the patient’s axilla).
This stretch is held for 15–30 seconds allowing a lengthening of shortened musculature in the region. (Note: starting position is as for Fig. 4.22.) Repeat as necessary.
Short latissimus dorsi MET method (b) The patient is side-lying, affected side up. The arm is taken into abduction to the point of resistance, so that it is possible to visualise, or palpate, the insertion of the shortened fibres on the lateral chest wall.
The condition is treated in either the acute or chronic mode of MET, at or short of the barrier, as appropriate.
As shown in Figure 4.29, the practitioner stands near the head of the patient, slightly behind, and holds the upper arm in the chosen position while applying the other hand to stabilise the posterior thorax area, or the pelvic crest, from where the stretch will be made.
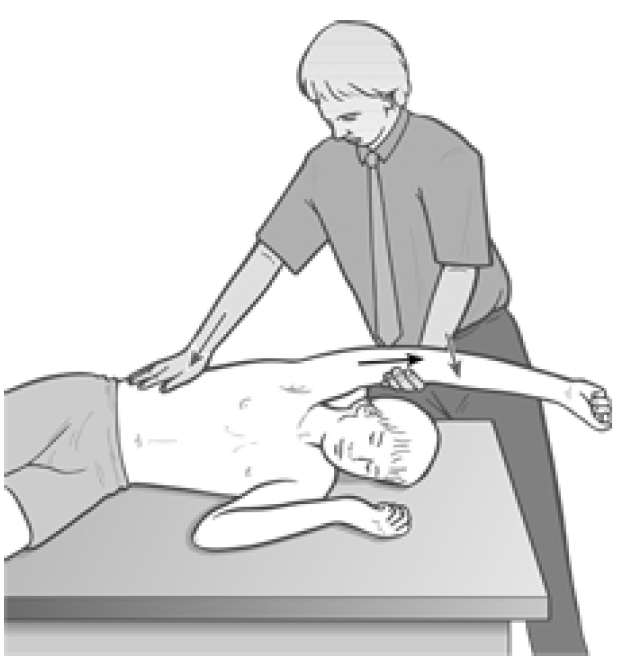
Figure 4.29 Treatment of latissimus dorsi. A variety of different positions are required for the stabilising hand (on the chest wall as well as on the crest of the pelvis) to allow for precise application of stretches of fibres with different attachments, following the sequence of isometric contractions.
A build-up of tension should be palpated under the stabilising hand as the patient introduces an isometric contraction by attempting to bring the arm towards the ceiling, backwards and down (towards their own lower spine) against firm resistance, using only a modest amount of effort (20%) and holding the breath if appropriate (see notes on breathing, Box 4.2).
After 7–10 seconds, both the effort and breath are released and the patient relaxes completely, at which time the practitioner introduces stretch to or through the barrier (acute/chronic), bringing the humerus into greater adduction while applying a stretching/stabilising contact on the trunk (with separate contractions and stretches for each contact) anywhere between the lateral chest wall and the crest of the pelvis.
A downward movement of the humerus, towards the floor, assists the stretch following a separation of the practitioner’s two contact hands to remove all slack. As in the stretch of pectoralis major, there should be two phases – a distraction, taking out the slack, and a movement towards the floor of the practitioner, by flexing the knees – to induce a safe stretch. Repeat as necessary.
Ultimately, it should be possible to achieve complete elevation of the arm without stress or obvious shortness in latissimus fibres so that the upper arm can rest alongside the ear of the supine patient.
Dr. Alex Jimenez offers an additional assessment and treatment of the hip flexors as a part of a referenced clinical application of neuromuscular techniques by Leon Chaitow and Judith Walker DeLany. The scope of our information is limited to chiropractic and spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
By Dr. Alex Jimenez

Additional Topics: Wellness
Overall health and wellness are essential towards maintaining the proper mental and physical balance in the body. From eating a balanced nutrition as well as exercising and participating in physical activities, to sleeping a healthy amount of time on a regular basis, following the best health and wellness tips can ultimately help maintain overall well-being. Eating plenty of fruits and vegetables can go a long way towards helping people become healthy.

WELLNESS TOPIC: EXTRA EXTRA: Managing Workplace Stress
Post Disclaimer
Professional Scope of Practice *
The information herein on "Assessment and Treatment of the Pectoralis Major and Latissimus Dorsi" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.