El Paso, Tx.’s Scientific chiropractor Dr. Alexander Jimenez looks at a case study of a rugby player who got more than he wanted to tackle.
Table of Contents
The Player & Mechanism Of Injury
A 115kg rugby union player who plays as a hooker is presented by this case study. During a competitive game he went in to execute a tackle with a bent knee, and the player being tackled fell onto him. As he went to get up off the floor that he felt popping sensation and a severe pain in the knee and he was unable to straighten the knee. He was not able get to a position to come off the field or to straighten it and immediately fell to the floor with the knee locked in 30 degrees of flexion. He was stretchered off the field and taken immediately to the medical room where he had been administered some powerful painkilling medications (Entonox). At the time his knee was far too painful to test properly; however, the attempted examination by the physician discovered that the knee was not able to be unlocked, a gross swelling had already begun but the joint play on anterior draw (Lachman’s test) felt normal.
It was felt that due to the discomfort, the rapid and the inability to unlock the knee, the diagnosis was that the player had sustained an meniscus rupture or had endured a tibial plateau fracture.
The player underwent an MRI of the injured knee the next day. The report was as follows:
Findings
There has been an acute tear of the meniscus with flipping of the posterior horn fragment to the anterior part of the lateral tibiofemoral compartment.
- No injuries are seen inside the joint compartment.
- The ACL is undamaged.
- The PCL, medial and lateral collateral ligaments are intact.
- The corner structures are intact.
- No meniscal tear is seen.
- No injuries are observed in the medial tibio
- There is fibrillation to the medial patellar facet cartilage at the level of the patella equator.
- No injuries are seen within the trochlea.
- No signs of subluxation is observed.
- Patellar tendon and the quadriceps expansion appear within normal limits.
Impression
- Acute tear of the lateral meniscus with flipping of the posterior meniscal fragment into the anterior lateral tibiofemoral joint compartment.
The player was treated surgically with a repair and the flap was success- fully relocated and sutured into position. He was discharged wearing a motion-limiting brace (0-60 degrees originally). The rehab program is explained below. He returned to play with operative and had no difficulties.
Anatomy Of The Meniscus
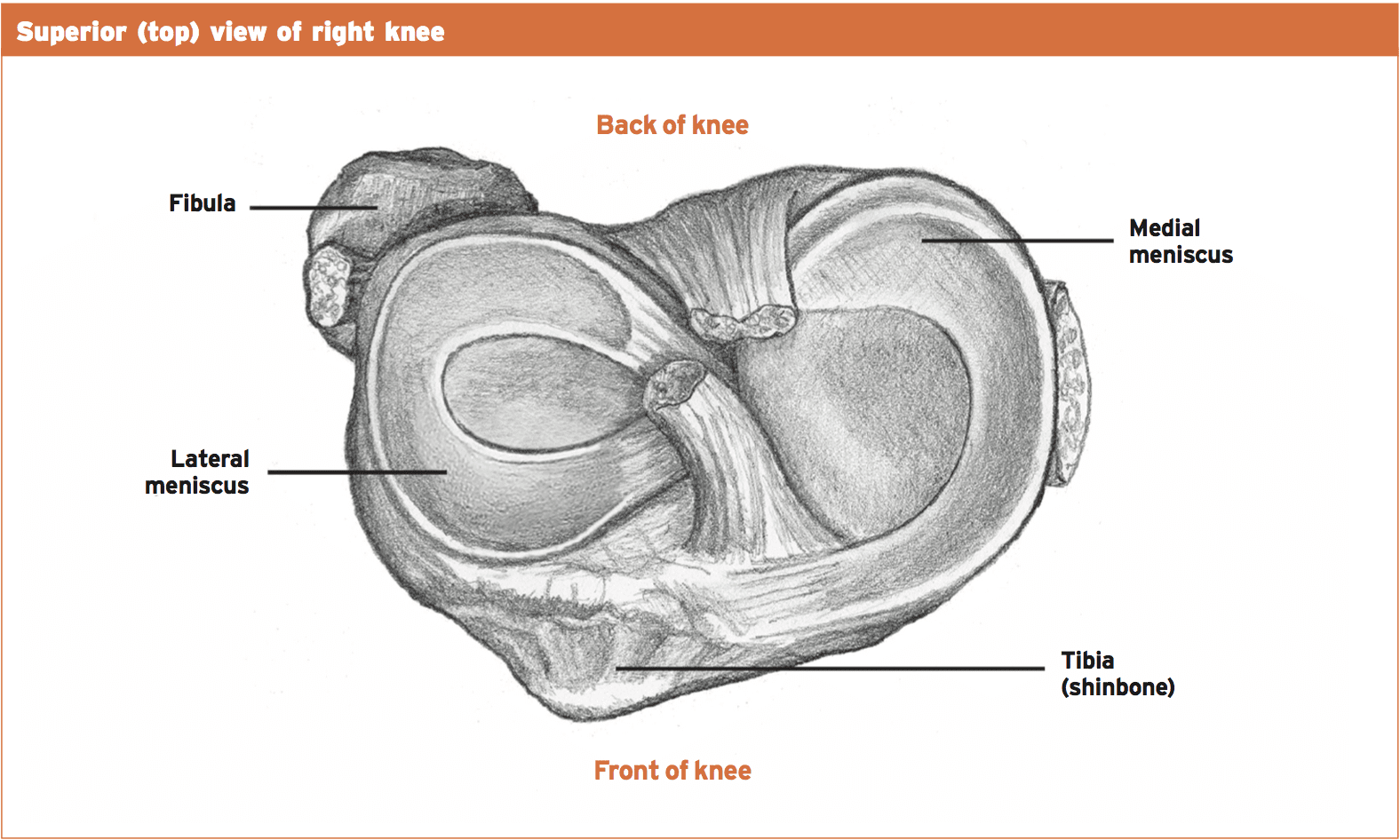
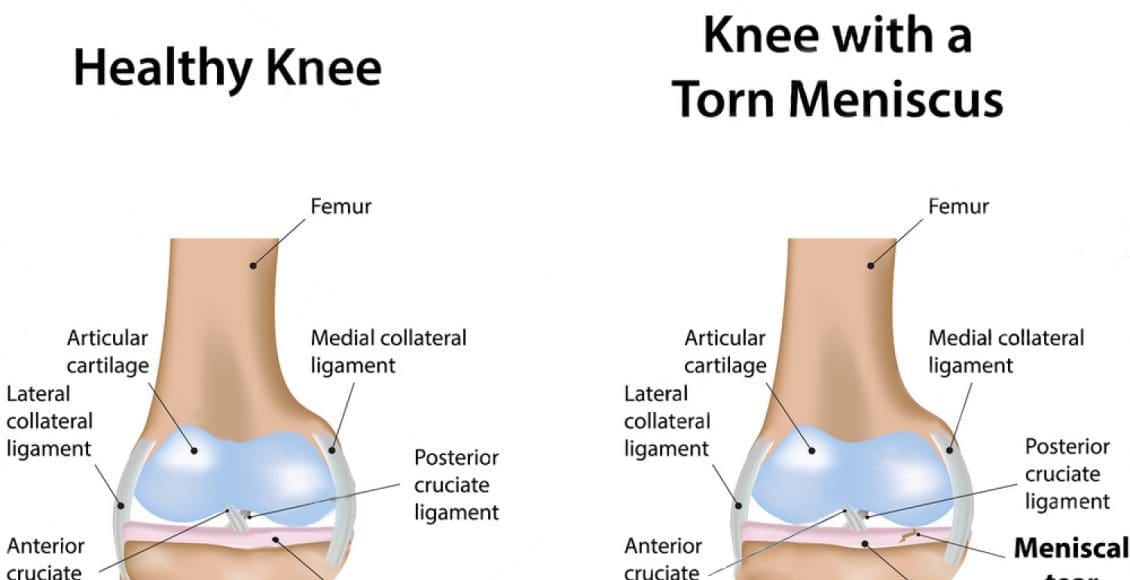
The plateaus are attached to by the two meniscus and the congruency of the tibia enhances . The meniscus are made from a fibrocartilage and they are wedge-shaped. The two meniscus are ‘C’-shaped being the lateral more curved and more crescent-shaped. The meniscus attach to the tibial plateau in the anterior and posterior horns through the intercondylar eminence. They are attached at the periphery with ligaments.
Uniquely the medial collateral ligament which restricts the freedom of the meniscus is attached to by the medial meniscus. The lateral meniscus is attached to the femur via two specific ligaments (ligaments of Wrisberg and Humphreys).
The unique blood supply to the meniscus determines its healing capability in the event of injury. The peripheral portion of the meniscus (between 10-30%) receives a direct blood supply and this is known as the red-red zone of the meniscus. Terminal loops are sent by the small blood vessels to the center material of the meniscus and this is termed the red-white zone of the meniscus. The part that is remaining only receives nourishment and this is called the zone that is white-white.
The meniscus have a range of significant functions that are biomechanical. They function as a shock absorber (they can absorb as much as 45-70% of weight-bearing load) as well as a spacer between the femur and tibia to prevent any connection between the two bones, they offer a degree of knee stability, and also have a proprioceptive function. The joint surfaces are also lubricated by their existence in the knee. This is evident in knees which have had meniscus removal — they show onset arthritic changes as the bones no longer have a cushioning effect.
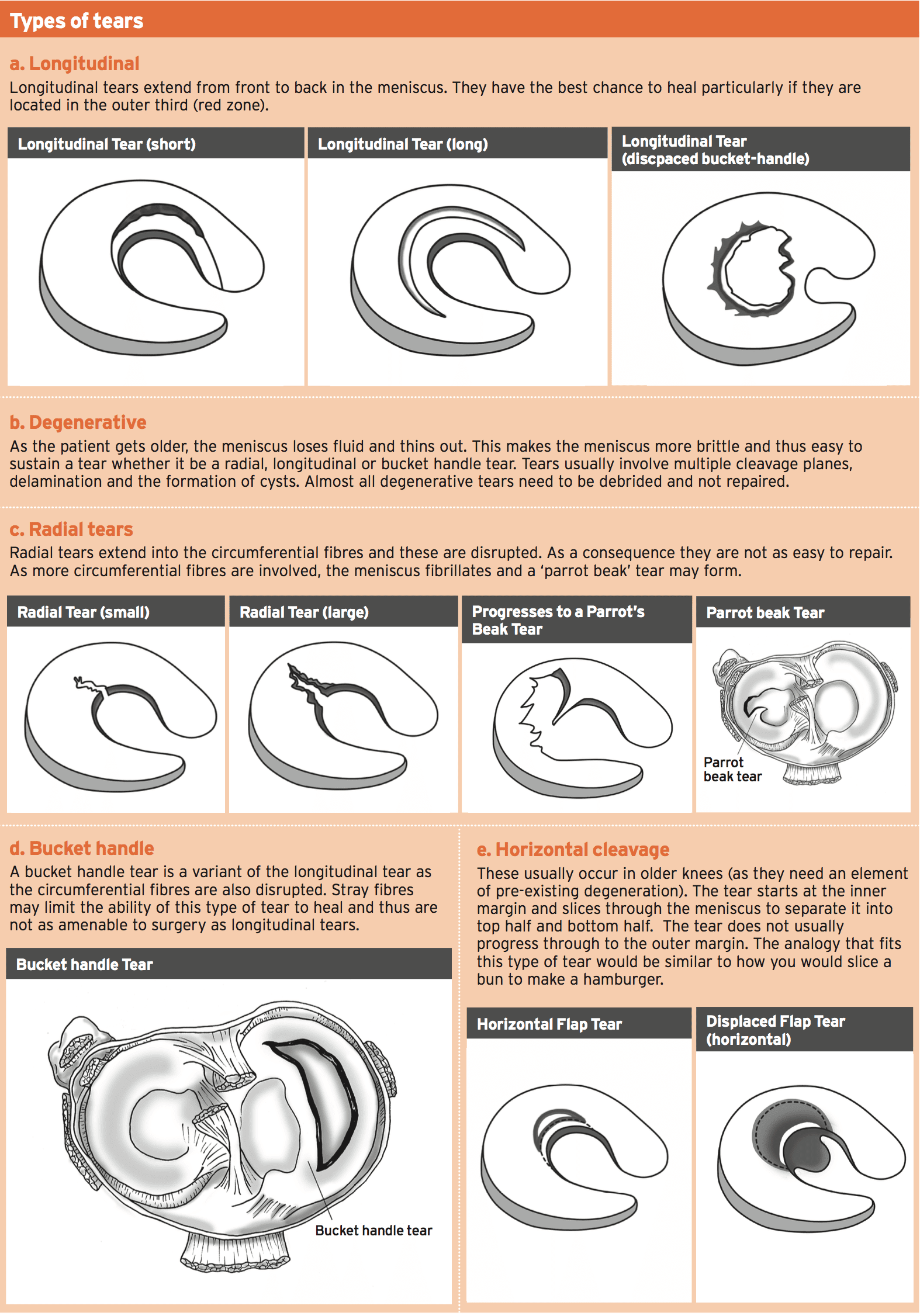
Throughout knee flexion the femoral condyles slide and load the posterior horn of the meniscus. The knee also internally rotates with knee flexion and a shear effect is imparted by this across the meniscus the medial meniscus nonetheless, the meniscus translates by double the space of the medial meniscus in a front-to-back direction during knee flexion. These two features that are biomechanical make the meniscus more susceptible to injury in flexion and rotation.
Forces Acting On The Knee
Meniscal tears in the knee occur when the knee is flexed and concurrently and the condyle loads the meniscus the knee rotates along with a shear force is applied to the meniscus. If the meniscus collagen’s ability to withstand this shear is exceeded by this shear force, a tear will result. This happens in the athletic knee. This sometimes happens typically in cutting and step- ping actions or landing and twisting simultaneously. The athletic activities most likely to make this shear effect on the knee are NFL, soccer, rugby, volleyball, netball and tennis.
In an older degenerated knee, the fluid content of the meniscus is reduced due to age-related changes to the meniscus and cartilage structures. It’s much easier to damage the meniscus with in a knee with a meniscus that is degenerated.
 Clinical Features Of Meniscal Tears
Clinical Features Of Meniscal Tears
Subjective
The individual usually remembers the specific mechanism of injury as being a step or cutting maneuver that induces knee flexion and then adds spinning (netball, basketball, volleyball, soccer, touch rugby), or they might be tackled and the knee is forced into rotation (rugby, NFL). Furthermore, the patient may be caught in a deep squat posture and tries to bounce out of that position (‘bum to ground’ squats) or they may fall and slide with their knee flexed (MMA, martial arts, extreme sports). As the latter occurs, the foot may be caught on the floor as the knee is flexed and a rotational force may be applied to the knee.
The level of pain experienced can vary depending on the kind of tear and if concomitant injuries like collateral ligaments and ligaments are involved. Some tiny tears might be painless and pose as a sore knee afterwards. This might be more prevalent with older degenerated knees. Some individuals may experience a definitive popping sensation as the tears acutely or tearing sensation.
More severe injuries such as bucket handle the meniscus may be displaced by tears . These may spontaneously unlock using a sensation.
Objective
An torn meniscus’ typical features are:
- joint effusion. This will be detected during examination on a standard fluctuation test;
- joint line tenderness. This is more prevalent with meniscus tears;
- Pain on loaded flexion — duck and squats walks;
- restricted flexion and/or extension (in anterior horn tears). This may be pain- limited and/or restricted by a block (because of the torn meniscal flap). ;
- McMurray’s test (passive flexion/rotation) may be positive in an acute tear; however, the rate of false negatives can be very high. A McMurray’s may replicate a clunk or click in the knee.
Management
Whether surgery is not needed by a meniscus or not depends upon a number of key variables:
- The zone — red zone tears cure well whereas zone tears don’t heal;
- Type of tear bucket handle tears will probably cause locking of the knee so need surgery. Tears that are slightly painful but not locked may do well with conservative management;
- Demand of the sportsman — a young footballer will require as meniscus as possible, therefore surgical repair would be indicated.
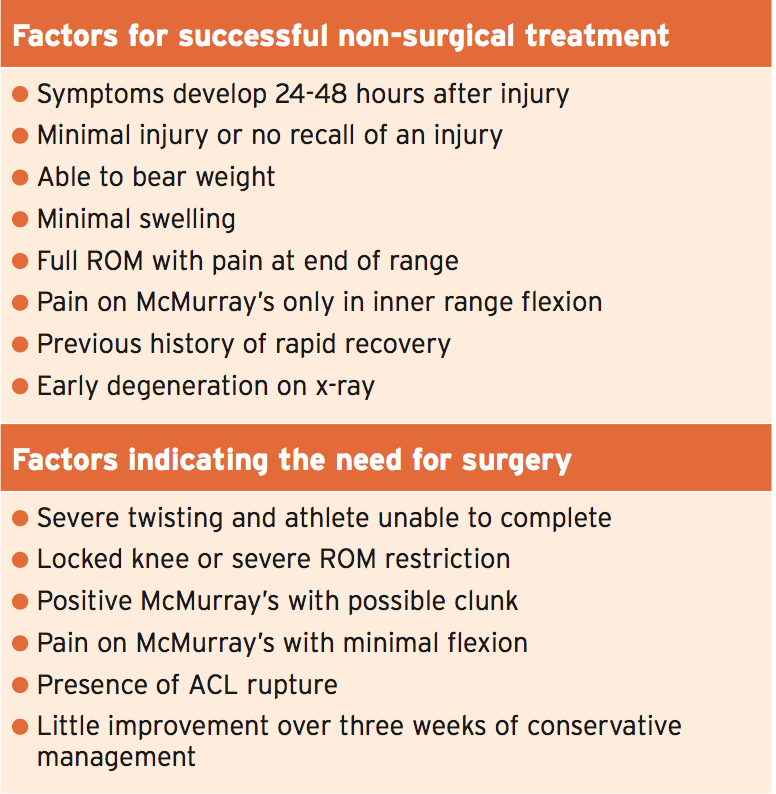
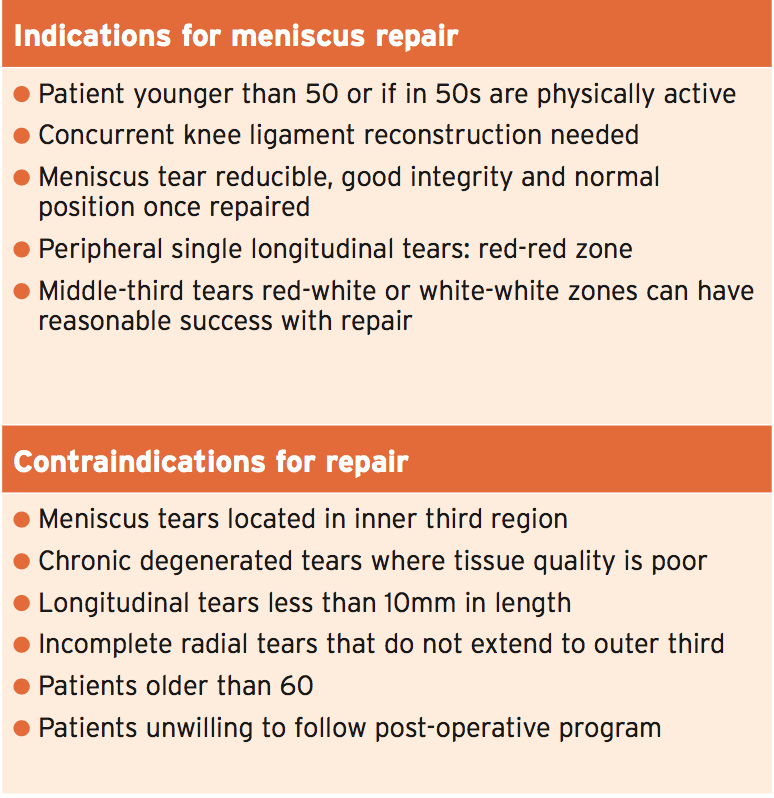
Brukner and Khan (2012) have offered a number of criteria which might help in determining surgical versus nonsurgical treatment.
Furthermore, Noyes et al (2012) provide additional advice on whether the tear should be repaired or removed.
In the case study presented, the player had an inability to compete and an episode of twisting, had a locked knee with his McMurray’s and severe pain was unable to be analyzed as a result of pain. So surgery was the only option, the MRI confirmed the severity of the tear and displacement.
Surgery
The purpose of surgery is to preserve as much of the meniscus as possible. In athletes, the current preference is by repairing the tear with sutures preserve the meniscus. In knees and crush that is severe type accidents will the meniscus be eliminated. Unfortunately not all meniscus tears can be repaired, especially if damage has occurred.
Long-term follow-up of meniscus injuries that are debrided versus mended reveal that in debrided meniscus, the chance of early onset osteoarthritis is much higher due to the reduction in surface of the meniscus.
Variations exist in the sort of repairs that a surgeon may perform. It is generally accepted that sutures are prefer- able as perpendicular runs to the circumferential fibers of the meniscus to horizontal sutures.
The timeframe for rehabilitation will differ based on the location and extent of the tear. Tears of the meniscus which are repaired will require more than lateral tears.
Monitoring of the knee is required as remaining meniscus and the articular cartilage take the time to adapt to load increases. Monitoring of signs such as knee and effusion stiffness will alert the clinician that the knee is not able to accommodate to loads that are applied.
Although not discussed in this bit, more and more evidence is showing that meniscus transplantation can be successful in the management of meniscus.
Post-Surgical Rehabilitation
The player’s post-surgical rehabilitation is presented as a color-coded chart below. The purpose of the chart is that it represents a visual reference point for the player to refer to. It progresses through different stages or different ‘danger zones’. Black represents the high-risk stage then it passes through red, orange, yellow, green and finally white when there is minimal risk.
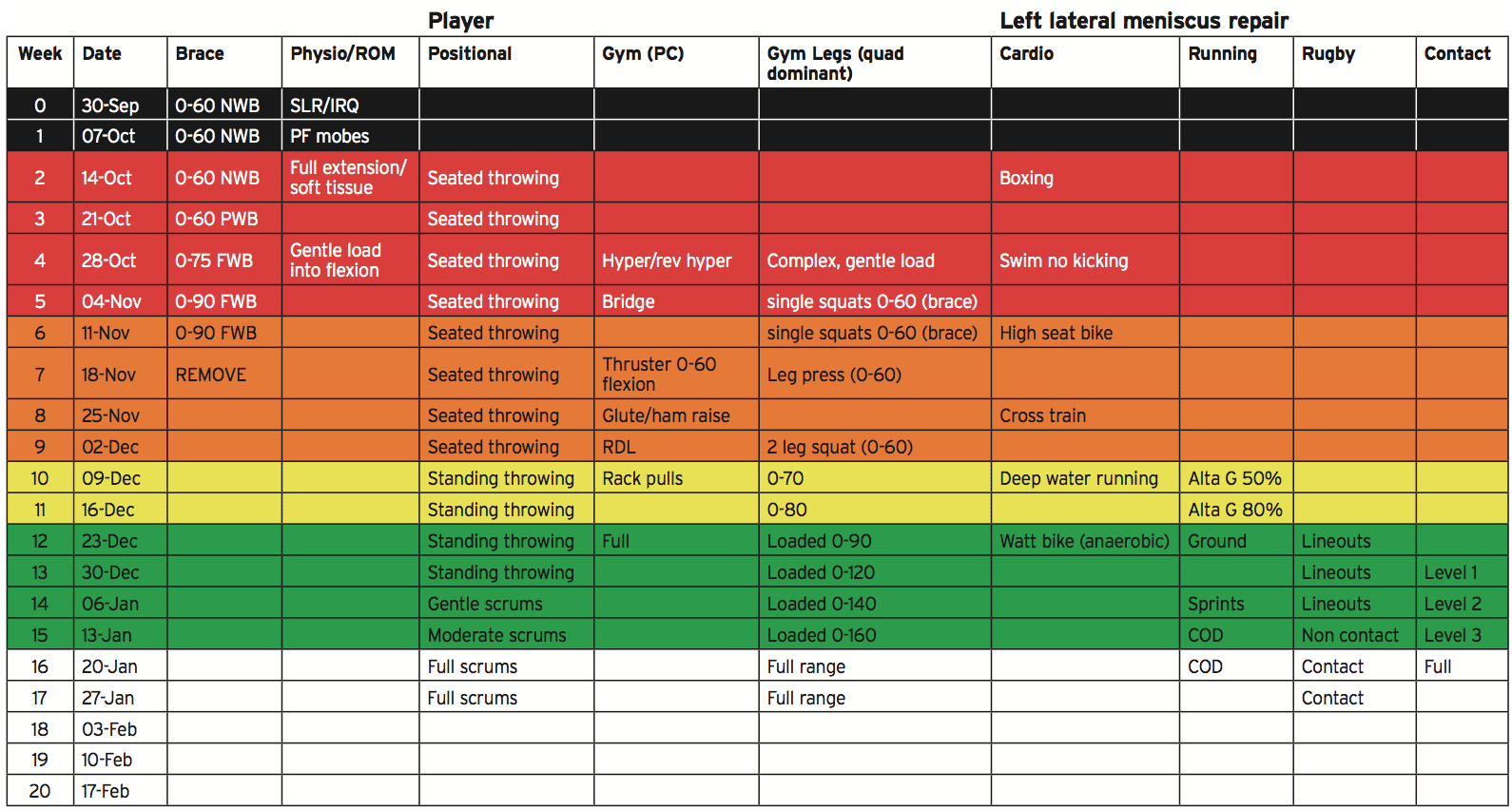 The key features of the attached rehabilitation program are as follows:
The key features of the attached rehabilitation program are as follows:
Weight bearing status
1. The surgeon initially wanted the player non-weight bearing as the lateral meniscus had sustained a significant delamination off the tibial plateau.
2. Partial weight-bearing on crutches started at four weeks post-op and progressed over the two weeks until he was full weight-bearing at week six post- op. The player continued to use crutches in full weight-bearing when outdoors for safety up to seven weeks post-op.
Range of movement
1. Due to the extensive nature of involvement of the lateral meniscus, the surgeon wanted the player motion-limited for the first four weeks from 0-60 degrees. He was concerned that flexion past 60 degrees would create excessive compressive effect on the posterior horn of the meniscus.
2. From week four the brace was opened up to 75 degrees and then in week 5 to 90 degrees.
3. The brace was removed at seven weeks post-op.
Physiotherapy/manual therapy
1. Range of allowable movement (0-60) was maintained with:
- patellofemoral mobilizations
- passive and active knee flexion/extension
- soft tissue massage to calves, popliteus, hamstrings and ITB.
Exercise therapy
1. The player was initially started on simple inner range quads in supine (0-20 degrees), straight leg raise and active knee flexion/extension in motion limiting brace in sitting on bed.
2. A muscle stimulator (Compex) was used to maintain quads (disuse atrophy mode).
3. Hip exercises were also started focusing on hip abduction (side lie) and extension (prone).
4. From week 4 post-op he started using a muscle stimulator in single leg squat position in brace.
5. From week 6 he was performing muscle hypetrophy mode muscle stim squats on single leg from 0-60 degrees.
6. He started leg press (0-60) at week 7.
7. He started two-legged squats (0-60) at week 9 and the range was increased 10-20 degrees per week over weeks 10-15. He was performing full squats (0-110 degrees – parallel thigh) by 15 weeks post-op.
8. He squatted 180kg for six reps at 15 weeks post-surgery (his PB was 210kg for six reps).
Posterior chain
1. The player started loaded hyperextension and reverse hyperextension exercises from week 4.
2. He started bridging in brace from week 5.
3. He started performing hip thruster in brace from week 6.
4. More high demand hip-dominant exercises were then added weekly.
Cardio/cross train
1. Seated boxing was started at week 2 post-op.
2. Swimming with no kicking was started at week 4 post-op (enough time to allow full suture healing).
3. High seat bike was started at week 6 to limit knee flexion to 0-60.
4. Cross trainer was started at week 8.
5. Deep water running was introduced at week 10 (this required more than 60 degrees of knee flexion hence why it was delayed until week 10).
6. Alta G (anti-gravity treadmill running) at 50% bodyweight was introduced at week 10 and this went to 80% week 11.
7. Hard anaerobic efforts on Watt bike were introduced from week 12.
Running
1. Alta G running started at week 10 although this was low-level intensity – 8-10 kph.
2. The surgeon reviewed the player at 12 weeks post-op and allowed the player to commence ground running.
3. The player ran every second day and the volume was gradually increased each session.
4. Over three weeks the player ran on 13 occasions. The distance was gradually increased from 500m to 6km over the 13 sessions. A player of his position would cover 6-8 km a game so the bottom end of the distance expectation was chosen.
5. Speed elements were gradually introduced over the 13 sessions; however, top speed was delayed until the second last session.
6. The player ran a standard 1.2km field shuttle fitness test at week 13 post-op. His pre-injury best was 5.04mins and his first attempt post-injury was 5.15, which was well within 90% of his best effort.
7. He started change of direction at 15Â weeks post-op and quickly progressed through the stages.
8. He also started non-contact skills work at 15 weeks post-op.
Skills/rugby
1. As a line out forward he is required to throw the ball into the line out; this skill element was maintained early on by incorporating seated (on Swiss ball) throwing from week 4.
2. He started standing throwing at week 10 post-op.
3. Solitary machine scrums started at week 14, five-man scrums at week 15 and full scrums in weeks 16 and 17.
4. Non-contact skills started at 15 weeks post-op.
5. Progressive contact training was started at week 13 and quickly progressed over four weeks.
Criteria For Returning To Play
The accepted criteria for return to play following surgery are:
1. No effusion;
2. Full range of movement;
3. Normal quadriceps bulk and strength;
4. Equal proprioception left to right (as measured with a star excursion balance test – SEBT);
5. Full completion of training for two weeks;
6. Strength levels within 90% of pre- injury levels; and
7. Field conditioning tests within 90% of pre-injury levels.
Conclusion
This case study presents a instance of a flipped bucket handle tear of a meniscus in an elite level rugby player. A mechanism of injury resulted in an irreducible locked knee and the posterior horn of the meniscus flipping itself in the anterior compartment of the knee and detaching from the attachment, leading to acute pain.
Successful surgery allowed for preservation and a full recovery of the lateral meniscus with no loss of meniscal substance. The mature of the injury resulted in a protracted rehabilitation period nonetheless, the player involved was able to successfully return to play after surgery.
References
1. Brukner et al (2012) Clinical Sports Medicine (4th edition). McGraw-Hill Australia. NSW.
2. Noyes et al (2012) Meniscus repair and transplantation: a comprehensive update. Journal of Orthopedic and Sports Physical Therapy. 42(3): 274-290.
3. Brindle et al (2001) The meniscus: review of basic principles with application to surgery and rehabilitation. Journal of Athletic Training. 36(2); 160-169.
4. Rath E and Richmond JC (2000) The menisci: basic science and advances in treatment. Br J of Sports Medicine. 34: 252-257.
5. McDermott I (2011) Meniscal tears, repairs and replacement: their relevance to osteoarthritis of the knee. Br J of Sports Medicine. 45: 292-297.
Post Disclaimer
Professional Scope of Practice *
The information herein on "The Meniscus: A Scientific Perspective" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card


 Clinical Features Of Meniscal Tears
Clinical Features Of Meniscal Tears

 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.