In the first of this two-part article chiropractor, Dr. Alex Jimenez discusses the progression from acute ankle sprain to chronic and recurrent instability, the relevant anatomy and biomechanics, how chronic instability can be identified in the athlete
Ankle sprains are one of the most common injuries experienced by athletes, and account for a large percentage of lost time from competition(1,2). The frequency of acute ankle sprain is relatively high in the athletic population, with some researchers claiming that injuries to the ankle joint account for 20% of all joint injuries(3). In a comprehensive review, it was found that lateral ankle sprain was the most common ankle injury in 33 out of 43 sports(1). The lateral ligament complex is the most frequently injured ankle structure, with medial ligament (deltoid) injuries and syndesmosis injuries being less prevalent.
The majority of acute ankle injuries recover reasonably quickly with conservative treatment, which incorporates strengthening, ankle mobilisations, balance and proprioception and protective braces and strapping. However, a number of acute ankle sprain sufferers may go on to develop later-stage chronic or recurrent ankle instability. This results in a feeling that the ankle feels vulnerable, episodes of catching and ongoing pain and further episodes of repeat ankle sprains(4). One of the highest risk factors for an ankle injury is in fact a history of previous ankle injury(5). Of further significance is that ankle sprains have a high rate of recurrence (as high as 80% in high-risk sports)(5,6). This suggests that many ankle sprain sufferers will most likely sprain their ankles again, and this may then cascade to late stage chronic ankle instability (CAI).
Table of Contents
Relevant Anatomy & Biomechanics
When the ankle is fully loaded into weight- bearing and dorsiflexion, the articular surfaces and joint congruency are the main stabilisers of the ankle, and prevent the talus from rotating and sliding(7). The ligaments of the ankle do play a role in stability in this position; however they become a lot more crucial in ankle stability as the ankle approaches plantarflexion. In plantarflexion, the talocrural joint is in a loose-packed position and therefore joint congruency and inherent joint stability are reduced. This means the ankle ligaments play a much larger role in ankle stability (and thus are more vulnerable to injury) in this position.
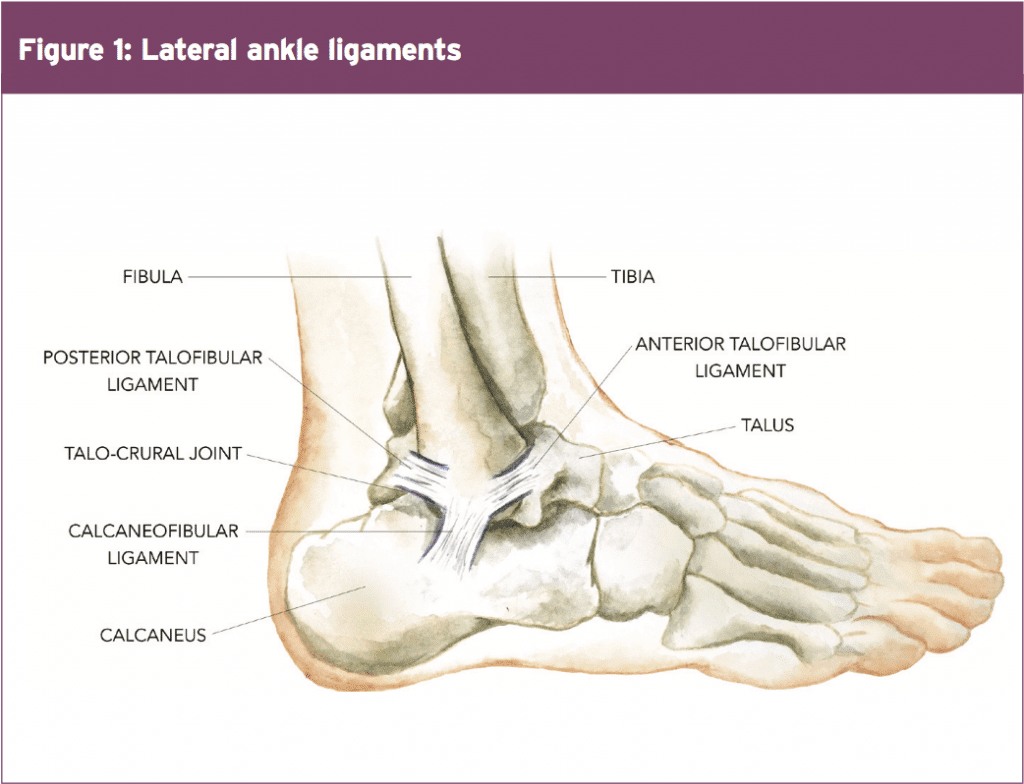
The ligaments of the ankle include the anterior talofibular ligament (ATFL), posterior talofibular ligament (PTFL), calcaneofibular ligament (CFL), and deltoid ligament on the medial side of the ankle (see Figure 1). The ATFL, PTFL, and CFL support the lateral aspect of the ankle, while the deltoid ligament provides medial joint stability. For the purposes of this article the deltoid ligament will not be discussed and the focus will remain on the lateral ankle ligaments, the ATFL, CFL and PTFL.
The ATFL courses from the lateral malleolus anteriorly and medially toward the talus at an angle of approximately 45 degrees from the frontal plane(8). The ATFL is an average of 7.2mm wide and 24.8mm long. Studies have shown that the ATFL prevents anterior displacement of the talus from the mortise, and excessive inversion and internal rotation of the talus on the tibia(7,9). The strain in the ATFL increases as the ankle moves from dorsiflexion into plantar flexion. Furthermore, compared with the PTFL, CFL, anterior inferior tibiofibular ligament, and deltoid ligament, the ATFL demonstrates lower maximal load and energy to failure values under tensile stress. This is the reason why it is the most commonly injured ligament in the classic inversion with or without plantar flexion mechanism.
The CFL courses from the lateral malleolus posteriorly and inferiorly to the lateral aspect of the calcaneus at a mean angle of 133 degrees from the long axis of the fibula(8). The CFL restricts excessive supination of both the talocrural and subtalar joints. Studies have demonstrated that the CFL restricts excessive inversion and internal rotation of the rearfoot, and is most taut when the ankle is dorsiflexed(7). Considering that the CFL is under less strain in plantarflexion, injury to this ligament is not as common. It is more commonly injured if the inversion mechanism occurs in neutral to dorsiflexion positions – hence the CFL runs a distant second as the most-often injured of the lateral ankle ligaments.
The PTFL runs from the lateral malleolus posteriorly to the posterolateral aspect of the talus. The PTFL has broad insertions on both the talus and fibula and provides restraint to both inversion and internal rotation of the loaded talocrural joint(7,8).It is the least commonly sprained of the lateral ankle ligaments as it is only under a strain load when the ankle is in full dorsiflexion; the congruency position where the talus and ankle mortise are closely locked together and hence relatively stable.
Other ligaments such as the syndesmosis ligament, subtalar joint ligaments, bifurcate ligaments and also the supporting tendons may also be injured in the inversion ankle sprains however they will not be discussed in the context of chronic ankle instability.
What Is CAI?
The term chronic ankle instability (CAI) has been interchanged with other names and definitions in the literature such as ‘recurrent ankle instability’ and ‘residual ankle instability’. For the purposes of this article, the term CAI will be used. It has often been assumed that all cases of CAI follow the same sequalae from the original lateral ligament injury, which then progresses to episodes of recurrent giving way and CAI. This leads to the assumption that a consistent relationship between impairments and activity limitations exists. However, it is clear that sufferers of CAI are not a homogenous group but can consist of heterogenous groups of patients all with varying deficiencies and what leads to CAI may be multifactorial(10).
It has been reported that 32-74% of individuals with a previous history of ankle sprain suffer from some type of residual and chronic symptoms, recurrent ankle sprains, and/or perceived instability(11,12). Historically, CAI has been divided into two subgroups; mechanical and functional instability. Mechanical instability relates to the anatomical changes that follow an acute ankle sprain(13, 14). These include factors such as:
- Pathological laxity in the lateral ankle ligaments
Altered joint mechanics of the talocrural joint and distal tibiofibular joint - Synovial inflammation
- Soft tissue of bony impingement
- Degenerative changes
Functional instability is an ambiguous term that defines instability based on functional performance tests such as balance and proprioception, and a patient’s perception that the ankle feels ‘weak’ and ‘unstable’(14-17). This definition attempts to highlight and categorise the proprioceptive changes that follow lateral ligament injury. However, confusion and disagreement exists in the literature as to how mechanical and functional instability relate to each other – and if indeed they do interact(10).
Hertel (2002) proposed arguably the best model, which describes CAI as ‘having components of mechanical and functional instability that are not mutually exclusive and co-exist on a continuum, and when combined lead to recurrent sprain’(13). The changes with mechanical instability (anatomical) are proposed to lead to insufficiencies that predispose the person to further episodes of instability. Functional instability results from impairments such as impaired proprioceptive and neuromuscular control. When mechanical and functional insufficiencies are both present, recurrent sprain results and Hertel defined ‘recurrent sprain’ as his third subgroup (see Figure 2).
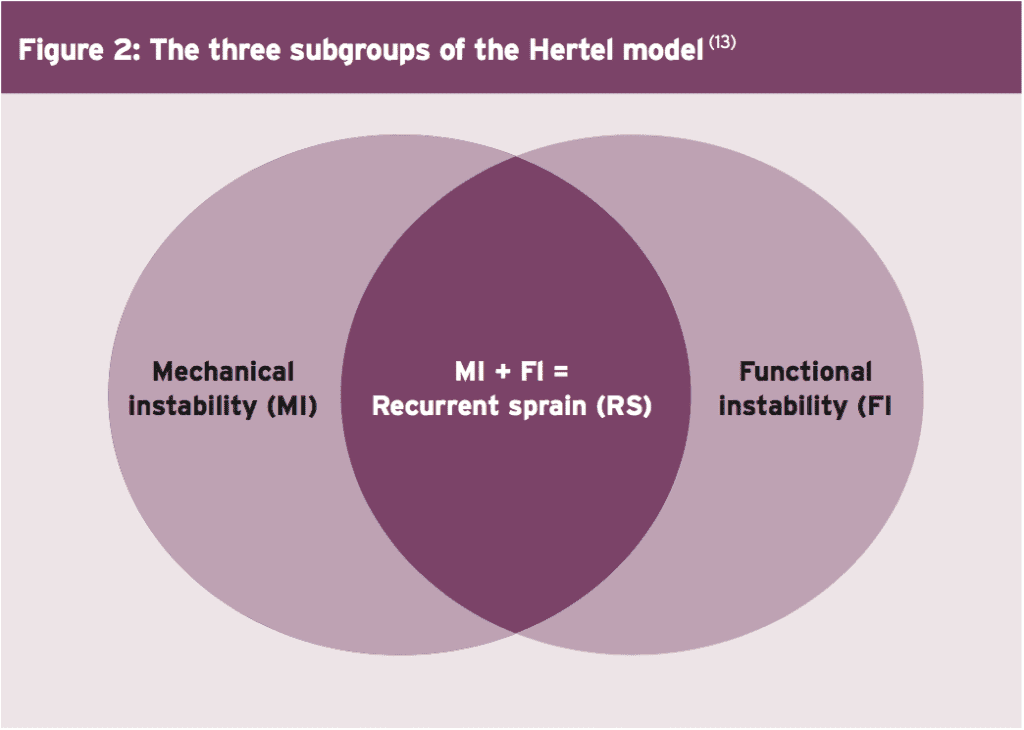
Anecdotally however, participants have reported residual feelings of instability and ankle laxity after ankle sprain but have not reinjured their ankles. Furthermore, studies on patients with both mechanical and functional instability performed differently to patients with only functional instability in areas such as postural sway(18) and peroneal reaction times(19). This suggests that the Hertel model may not be completely inclusive of all types of CAI.
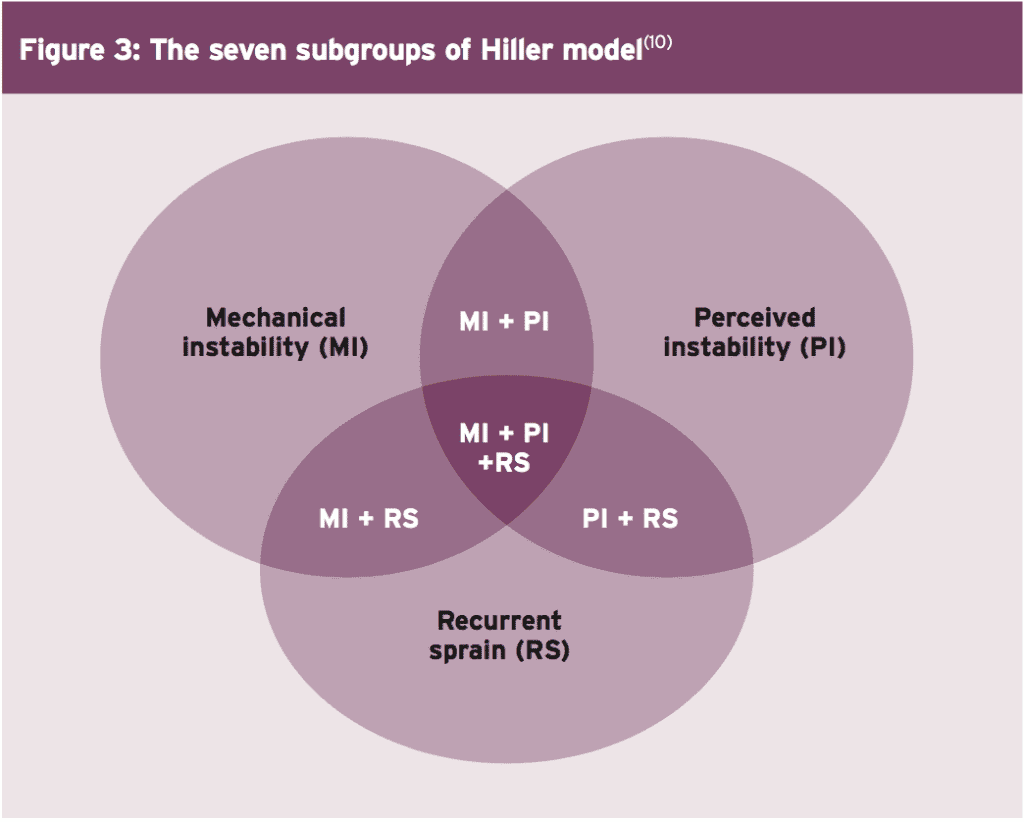
These inconsistencies led to an evolution of the Hertel model, which separates recurrent sprain from the presence of both instabilities. Hiller et al (2011) proposed to refine this model and expand the number of subgroups from 3 to 7 (see Figure 3)(10). They also redefined functional instability as ‘perceived instability’ because the key feature of this subgroup was the patient’s perception that their ankle felt unstable, even in the presence of normal testing with functional tests. They retained the subgroups called ‘recurrent sprain’ and ‘mechanical instability’ and argued that these three subgroups may exist independently or in combinations. For example, it is possible to have ‘mechanical instability’ and ‘perceived instability’ but to not have ‘recurrent sprains’.
The typical signs, symptoms and behaviours associated with CAI include(10):
- Giving way
- Mechanical instability (laxity on testing) Pain and swelling
- Loss of strength
- Recurrent sprains
- Functional instability (poor performance on balance and proprioception tests)
- Fear of uneven grounds
- Decreasing level of exercise and withdrawing from sport
Identifying CAI In Patients
Identifying patients who may in fact be suffering CAI may appear on first inspection to be relatively simple. However there are significant differences in how researchers classify CAI exist. In the simplest sense, mechanical instability (anatomical) is identifiable on physical examination (anterior draw tests and talar tilt) and stress radiographs. Functional instability however reflects subjective, patient-reported complaints of the ankle instability with or without clinical laxity(20,21). For the clinician therefore, it can often be difficult to identify patients who do indeed have accepted CAI. They may appear to be unstable on physical testing such as laxity on the anterior draw and talar tilt but they may perform well on functional assessment. They may complain of no sensations of feeling vulnerable.
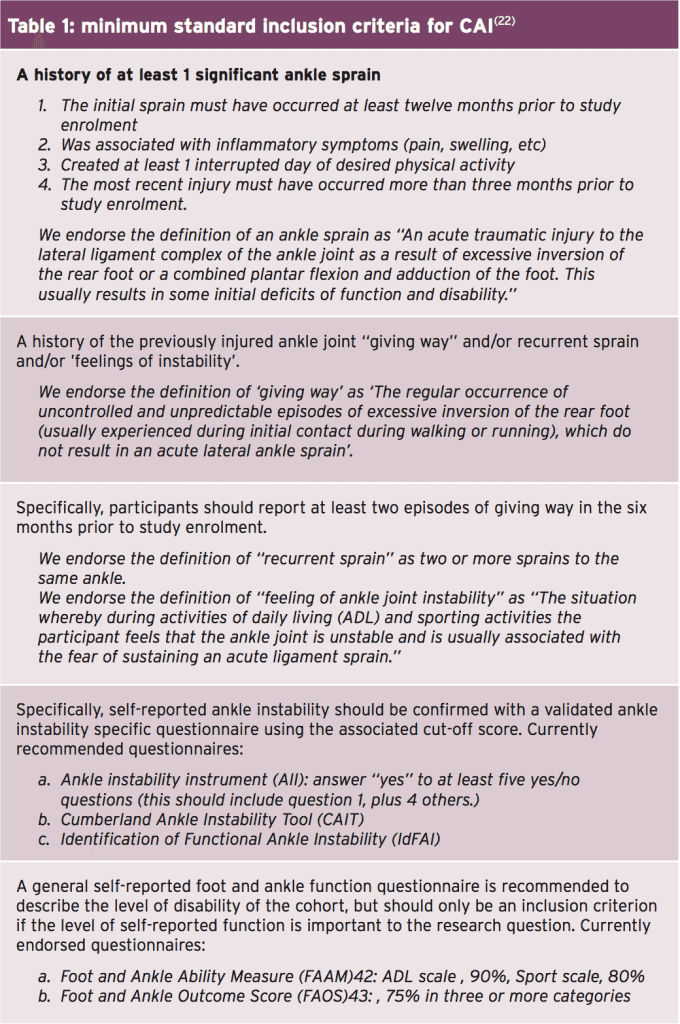
The International Ankle Consortium (a large focus group) attempted to categorise particular features of ankle injury that would lead to a consensus on how to actually define CAI, and to provide a selection criteria for patients with CAI(22). The primary purpose of this consortium was to categorise the selection criteria to define CAI for future research; however the clinician may extrapolate these criteria to help the identify patients in clinic who may be suffering CAI.
Table 1 (developed by The International Ankle Consortium) shows the minimum standard inclusion criteria for enrolling patients that fall within the heterogeneous condition of CAI. Although the purposes of this criteria list was to select patients with CAI into future research studies, the therapist may use this framework as a basis for deciding whether or not their patient does indeed suffer from CAI.
Signs &Â Symptoms Of CAI
It has been mentioned above that conflict exists as to the exact nature and definition of what is CAI. For the treating clinician, decisions must be made – for example conservative management or referral to an orthopaedic specialist for an opinion on surgical options. So what are the classic signs and symptoms that may alert a clinician that this CAI may require surgical intervention? The summary points below may act as a guide but are by no means exhaustive. Many of these points have been adapted based on findings referred to above(10,13,22):
1. Definite episode of previous lateral ankle sprain that led to pain, swelling, functional limitations and the need to avoid training and/or competition.
2. The timeframes suggested from initial acute injury to present CAI may be one year from initial injury; if the sprains have been recurrent, then the previous one in the previous 3 months.
3. A current awareness that the ankle still gives way and feels vulnerable, and this has occurred at least twice in the last six months.
4. Poor scores on a selected range of functional questionnaires.
On examination, the following signs may or may not be present and these will highlight both the mechanical and functional contributions if they exist:
1. Increased anterior draw test
2. Possible increase in talar tilt
3. Reduced ankle dorsiflexion as measured with a knee to wall test
4. More than 4cms difference on the forward reach with the Star Excursion Balance Test (23).
Imaging findings such as stress radiographs, ATFL attenuation on MRI and other soft tissue abnormalities may also indicate to the clinician that a degree of mechanical instability is present.
Conclusion
Ankle sprains continue to be an area of interest in sports medicine. Although research has produced advancements in prevention, diagnosis, and management, recent epidemiology studies have revealed that lateral ankle sprains remain a dominant sports injury. The majority of acute ankle sprains are managed conservatively, and on balance, the majority do have good functional outcomes. However, a small percentage of these ankle sprains may result in CAI, and these are the injuries that may require surgical intervention. The patho-anatomical reasons for CAI are multifactorial, relating to both anatomical deficits that lead to mechanical instability, and neuromuscular changes that lead to functional instability (or perceived instability). As a result recurrent sprains may be present. In the next edition of the Sports Injury Bulletin, part two will focus on possible surgical options to manage CAI and what is involved in the lengthy rehabilitation process.
References
1. Sports Med. 2007;37(1):73–94
2. Am J Sports Med. 1977;5:241–242.
3. United States Bone and Joint Initiative. The
Bone and Joint Decade: The Burden of
Musculoskeletal Diseases in the United States.
http:// www.boneandjointburden.org/.
Accessed November 1, 2013
4. Am J Med. 2008;121(4): 324–331, e6
5. Br J Sports Med. 2001;35:103–108
6. J Athl Train. 2002;37(4):376–380
7. Am J Sports Med. 1985;13:295–300.
8. Am J Sports Med. 1994;22:72–77.
9. Foot Ankle. 1988;9:59– 63
10. Journal of Athletic Training 2011;46(2):133–141
11. J Neurol Neurosurg Psychiatry.
2003;74(2):163–169.
12. Br J Sports Med. 2005;39(3):e14
13. J Athl Train. 2002;37(4):364–375.
14. J Bone Joint Surg Br. 1965;47:678– 685
15. J Athl Train. 2002;37(4):512–515.
16. J Orthop Sport Phys Ther. 1990; 11(12):605–611.
17. J Bone Joint Surg Br. 1984;66(2):209–212.
18. Int J Sports Med. 1985;6(3):180–182.
19. Foot Ankle Surg. 2000;6(1):31–38
20. Foot Ankle Int 2006; 27: 854-866
21. J Am Acad Orthop Surg 2008; 16: 608-615
22. Gribble et al (2014) Selection Criteria for
Patients With Chronic Ankle Instability in
Controlled Research: A Position Statement of
the International Ankle Consortium. Journal of
Athletic Training 2014;49(1):121–127.
23. J Orthop Sports Phys Ther. 2006
Dec;36(12):911-9
Post Disclaimer
Professional Scope of Practice *
The information herein on "Ankle Injury: When Instability Becomes Chronic Part I" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness, Personal Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and our family practice-based chiromed.com site, and focuses on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card





 Again, We Welcome You.
Again, We Welcome You.
Comments are closed.